Abstract
Background and Objectives
Arterial grafts have a better long-term patency rate than saphenous vein (SV) when used in off-pump coronary artery bypass surgery (OPCAB). However, arterial grafts in elderly patients are often diseased. We sought to compare the early outcomes achieved by using the two different types of composite grafts.
Subjects and Methods
We conducted a randomized trial to compare radial artery (RA) and SV composite grafts based on the in situ left internal mammary artery in 60 elderly (>70 years old) patients, who were scheduled to undergo OPCAB. Clinical outcomes and 1-year postoperative CT angiography results were compared. The quality of the conduit was evaluated by employing vascular ultrasonography, optical coherence tomography (OCT), and histologic examination.
Results
No differences in immediate postoperative morbidity and mortality were observed between the two groups. Early postoperative CT angiography revealed a SV patency rate of 100%, which was not different from that of RA composite grafts (99.1%). CT angiography after a year showed an overall patency rate of 96.3%. The overall patency rate of the SV group at 1 year was 94.7%, which was similar to that of the RA group (97.4%). Also, there was no difference in overall survival rate between the two groups. Vascular ultrasonographic images showed strong correlations between OCT and histopathology.
The long-term success of coronary artery bypass surgery depends on the patency of the employed conduits. Numerous previous studies have reported that the long-term patency rates of saphenous vein (SV) grafts are lower than those of internal mammary artery (IMA) grafts.1)2) Furthermore, there is a constant increase in the use of bilateral IMA, the radial artery (RA), or other arterial conduits to achieve total arterial myocardial revascularization.3-9) However, because of preexisting atherosclerosis in elderly patients, arterial conduits such as the RA are often diseased. Increasing age is strongly related to intimal thickening and medial thinning of the arterial conduits.10)11) In elderly patients, the SV is still widely used in grafts because of its accessibility, length, and ease of manipulation.
The lack of a convenient method in objectively assessing the intimal quality in real-time has created difficulties in establishing the effects of conduit selection practices. Vascular ultrasonography or catheter-based optical coherence tomography (OCT) have been shown to provide vascular images that yield morphologic information about the tissue that approaches histologic resolution.11)12)
Our aims in this study were to compare the outcomes of RA versus SV grafts in elderly patients (older than 70 years) scheduled to undergo isolated off-pump coronary artery bypass surgery (OPCAB), and to determine the feasibility of applying vascular ultrasonography or OCT preoperatively to screen conduits.
The present randomized single center trial was conducted from a period of March 2008 to December 2009 in the Department of Cardiovascular Surgery, Severance Hospital, Yonsei University Health System, Seoul, Korea. Sixty patients were allocated in a random ratio of 1 : 1 to two groups, according to the nature of composite graft used (35 patients in RA group, and 25 patients in SV group). This study was approved by the institutional review board (Yonsei IRB number: 4-2007-0249), and patients provided informed consent. Inclusion criteria were age ≥70 years and primary isolated OPCAB. Exclusion criteria were single-vessel disease, emergent surgery, a positive Allen test, or acute or chronic renal failure. Primary endpoints were early and 1-year graft patencies of the RA and SV in elderly patients who underwent OPCAB. Secondary endpoints were the incidence of diseased RA and SV in elderly patients, and the feasibility of preoperative vascular ultrasonography for RA when compared with OCT and histopathology.
All the patients underwent general endotracheal anesthesia with continuous Swan-Ganz catheter monitoring, transesophageal echocardiography, and arterial pressure monitoring.
After median sternotomy, the left IMA was harvested in all patients by using a skeletonization technique. At the same time, the RA or SV was harvested by using an open technique. The RA or SV was exposed by a longitudinal incision and all visible side branches were ligated. The SV was isolated together with a pedicle of surrounding fatty tissues (no-touch technique). After removal, the SV or RA was stored in heparinized blood. To check for leakage from the side branch, the grafts were flushed or distended manually. Heparin was administered just before Y anastomosis at a calculated dose to obtain an activated clotting time of greater than 350 seconds. Coronary artery bypass graft (CABG) was performed without cardiopulmonary bypass. The target arteries were stabilized by using a tissue stabilizer. In most instances, the left IMA was first anastomosed to the left anterior descending artery by using intracoronary shunts. A proximal silastic snare was used to anastomose other coronary arteries. Blood was removed from the sites of arteriotomy by using a misted CO2 blower and irrigation with warm saline.
Left IMA-RA or left IMA-SV Y anastomosis was initially performed for each RA or SV graft. Based on the requirement, sequential anastomosis or double Y anastomosis was performed on a case-by-case basis (Fig. 1).
Follow-up coronary CT and echocardiograms were performed on the seventh postoperative day and after a year of surgery. If newly developed angina or myocardial infarction occurred, additional coronary CT scans or angiograms were performed.
Bilateral evaluation of the radial arteries was performed by duplex ultrasound scanning (Acuson Sequoia C512; Siemens Medical Systems, Issaquah, WA, USA), using a 15 MHz probe after induction of general anesthesia. Each artery was imaged from the antecubital fossa to the wrist. The maximal intima-medial thickness was determined after sonography.
Discarded segments of the SVs or RA from the distal end of the conduit were stored in Hank's balanced salt solution at 4℃. Ex vivo evaluations were performed by using OCT (LightLab Imaging, Inc., Westford, MA, USA) within 2 hours of removal from the operative field. For the examination, a cannula was inserted into one end of the segment, and the other end was occluded with a heavy silk knot.
The OCT probe was introduced into the vessel though a Y connector attached to the cannula, allowing for gentle infusion of Hank's balanced salt solution during imaging, and automated pullback images were obtained. Plaques visualized in OCT cross-sectional images were categorized as fibrous, lipid-laden, or calcified based on prior reported criteria for OCT.12) Intimal disease within the analyzed conduit was quantified by determining the maximum intima-to-medial thickness ratio, and the severity of calcification (none, mild, and severe) was quantified by using intravascular ultrasonography as described previously.11)
Biopsy specimens for histologic processing were procured at the completion of the ex vivo scan. For exact matching of the OCT images with the corresponding histopathologic sections, the vessel sites at which the biopsy specimens were obtained were externally marked at the location of the catheter, as visualized by the rotating infrared light at the catheter tip. These image-guided biopsy specimens were then stored in solution before being embedded and frozen in a cutting compound. Additional sections were embedded in paraffin, sectioned at 5 µm, and stained with hematoxylin and eosin, Verhoeff-Van Gieson elastic fiber stain, and Masson's trichrome stain. The quality of the graft was graded in terms of the intima-media thickness ratio as determined by the image analyzer as follows: grade 0, intima-to-media ratio less than or equal to 0.25; grade 1, intima-to-media ratio greater than 0.25, but less than or equal to 0.5; grade 2, intima-to-media ratio greater than 0.5, but less than or equal to 0.75; grade 3, intima-to-media ratio greater than 0.75; grade 4, completely obliterated lumen due to thickening or thrombosis or both.13)
All values are expressed as means±standard deviations. Between-group differences in clinical variables were analyzed by the χ2 test, Fisher's exact test, unpaired t-test, or Mann-Whitney U test. The time-related events that we studied included major adverse cardiovascular events and death of the patient after being discharged from the hospital. Freedom from these time-related events was estimated by the nonparametric actuarial Kaplan-Meier method. All statistical analyses were performed by using Statistical Package for the Social Sciences (SPSS) 12.0.1 for Windows (SPSS, Inc., Chicago, IL, USA).
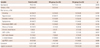
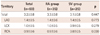
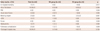
Preoperative characteristics of the patients (Table 1) and number of distal anastmosis according to the territories are described in detail (Table 2). The in-hospital mortality in the SVG and RA groups was 4.0 (1/25) and 0% (p=0.417), respectively. The incidence of postoperative morbidities including atrial fibrillation (n=16, 26.7%), acute renal failure (n=3, 5.0%), reoperation due to postoperative bleeding (n=3, 5.0%), low cardiac output syndrome (n=1, 1.7%), mediastinitis (n=1, 1.7%), pulmonary complications (n=2, 3.3%), and prolonged hospital stay (n=10, 16.7%) was not significantly different between the two groups (Table 3).
Early postoperative CT angiography demonstrated patency rates of 100 (75/75) and 99.1% (114/115) in the SVG and RA groups, respectively (p=0.412). In situ left IMA grafts showed a 100% (58/58) patency rate. The patency rate of SVG was 100% (50 of 50), which was not different from the overall patency rate of RA grafts {98.6% (72 of 73)} (Table 4).
One-year postoperative CT angiography demonstrated an overall graft patency rate of 96.3% (183/190). No significant difference was observed in the patency rate of the left IMA between the two groups (100%). The overall patency rate of the SVG group was 94.7% (71/75), which was not significantly different from that of the RA group {97.4% (112/115)}.
Histopathologic evaluation was performed with 23 RAs (66%), and 22 SVs (88%). Histopathologic examination revealed that the overall incidence of intimal hyperplasia of the radial arteries was 74% (17/23). One specimen (4.3%) showed an evidence of medial calcification. Five specimens exhibited an intima-to-media ratio of less than or equal to 0.25 (Kobayashi grade 0). Overall, 34.8% (8/23) of the radial arteries exhibited an intima-to-media ratio greater than 50% (Kobayashi grade 2 and above). According to the histopathology findings, fifty percent (11/22) of the SVs were reported to have diffused intimal hyperplasia.
The mean RA intima-to-media thickness (IMT) was found to be 0.511±0.046 (range, 0.233-0.7671).
The IMT as assessed by vascular ultrasonography was in strong correlation with that determined by OCT determination for the ex vivo RA segments (r=0.80, p<0.001), and histopathology (r=0.75, p<0.001).
The IMA graft is known to possess the best long-term patency rates of all conduits currently used in coronary artery bypass surgery, because of its resistance to atherosclerosis.14)15) Histologic characteristics, arterial wall metabolism, and tone regulation capability give rise to high resistance to atherosclerosis of the IMA. Although RA is generally successful as a graft, significant differences between the RA and the IMA have been noted in vasoreactivity and anatomy, which may explain the higher degree of atherosclerosis of the RA.16-18)
Total arterial coronary revascularization strategies were adapted to overcome the problems of the vein graft atherosclerosis and occlusion. Utilization of RA has increased up to 75% in all myocardial revascularization procedures. Therefore, atherosclerotic change in the RA has become crucial. Previous reports have stressed on the importance of the RA for total arterial coronary revascularization, by using Y- and T-grafting methods; overcoming RA spasm and probable etiologic factors for string sign have also been discussed, but preoperative RA atherosclerosis and postoperative patency were not mentioned.19) We believe that this could be a probable reason for the lower early rate of RA patency. It is important that vasospasm is resolved, but existing atherosclerosis cannot be evaluated after grafting.
Our results indicate that preoperative vascular ultrasonography can be used to assess the quality of the RA conduit before use, as the vascular ultrasonography results were in well correlation with the OCT and histopathology findings. Furthermore, we found that the early and 1-year CT angiographic patency rates of OPCAB by using the SV as a composite graft based on the in situ left IMA were similar to those of OPCAB by using a RA composite graft.
Previous studies have reported that in patients who underwent CABG, the long-term patency rate of SV grafts was lower than that of IMA grafts.1)2) However, SV grafts remain the most widely used graft because of the accessibility, length, and ease of use of the SV. The recent use of no-touch techniques to harvest the SV has been reported to significantly improve long-term graft patency.20)
In the present prospective randomized controlled study, either a RA or SV graft was used as a composite graft based on the left IMA. The preoperative characteristics of the RA and SV groups were similar. Early clinical outcomes, including hospital mortality and postoperative morbidity, as well as 1-year follow-up CT angiographic patency rates, were also similar between the two groups.
We used the SV as a composite graft on the left IMA based on the assumption that a vein graft anastomosed to the left IMA might be exposed to less pressure trauma or shearing stress than a graft anastomosed to the ascending aorta. We also hypothesized that the quality of the SV would be identical to that of the RA in elderly patients because the RA might have intimal hyperplasia or fibrous or calcified plaques in elderly patients.
We harvested the SV after systemic heparinization to prevent thrombus formation in the venous endothelium during vein harvest. Manipulation and tension were minimized and dilatation using a pressure syringe was avoided during harvest. These measures may have decreased intimal injury during harvest, thereby explaining the good patency rates.
Our study possesses the following limitations; the follow-up period of our study was relatively short. The mean follow-up period was only 8 months; a longer follow-up period is mandatory for accurate evaluation of the patency rates of the two types of graft conduits. Further studies involving large numbers of patients with a longer follow-up period are required.
In conclusion, based on the early clinical outcomes, our results indicate that the SVG could be used as an alternative composite graft to the RA in elderly patients.
Furthermore, vascular ultrasonography is an accurate, real-time, and reproducible means for assessing the quality of RA conduits.
Figures and Tables
Fig. 1
Construction of a composite graft with either the radial artery or saphenous vein based on the left internal mammary artery. LIMA: left internal mammary artery, LAD: left anterior descending artery, OM: obtuse marginal branch, Dx: diagonal branch, VD: vessel disease, RCA: right coronary artery.

Acknowledgments
The authors are deeply grateful to Sun-Hee Lim, RN. for collecting the data used in this study. This study was supported by a grant from the Korean Society of Cardiology for 2007 (7-2007-0382).
References
1. Loop FD, Lytle BW, Cosgrove DM, et al. Influence of the internal-mammary-artery graft on 10-year survival and other cardiac events. N Engl J Med. 1986. 314:1–6.
2. Cameron A, Davis KB, Green G, Schaff HV. Coronary bypass surgery with internal-thoracic-artery grafts: effects on survival over a 15-year period. N Engl J Med. 1996. 334:216–219.
3. Tagusari O, Kobayashi J, Bando K, et al. Total arterial off-pump coronary artery bypass grafting for revascularization of the total coronary system: clinical outcome and angiographic evaluation. Ann Thorac Surg. 2004. 78:1304–1311.
4. Fukui T, Takanashi S, Hosoda Y, Suehiro S. Total arterial myocardial revascularization using composite and sequential grafting with the off-pump technique. Ann Thorac Surg. 2005. 80:579–585.
5. Kim WS, Lee J, Lee YT, et al. Total arterial revascularization in triple-vessel disease with off-pump and aortic no-touch technique. Ann Thorac Surg. 2008. 86:1861–1865.
6. Glineur D, Hanet C, Poncelet A, et al. Comparison of saphenous vein graft versus right gastroepiploic artery to revascularize the right coronary artery: a prospective randomized clinical, functional, and angiographic midterm evaluation. J Thorac Cardiovasc Surg. 2008. 136:482–488.
7. Zacharias A, Schwann TA, Riordan CJ, Durham SJ, Shah AS, Habib RH. Late results of conventional versus all-arterial revascularization based on internal thoracic and radial artery grafting. Ann Thorac Surg. 2009. 87:19–26.e2.
8. Tatoulis J, Buxton BF, Fuller JA, et al. Long-term patency of 1108 radial arterial-coronary angiograms over 10 years. Ann Thorac Surg. 2009. 88:23–29.
9. Halbersma WB, Arrigoni SC, Mecozzi G, et al. Four-year outcome of OPCAB no-touch with total arterial Y-graft: making the best treatment a daily practice. Ann Thorac Surg. 2009. 88:796–801.
10. Osika W, Dangardt F, Gronros J, et al. Increasing peripheral artery intima thickness from childhood to seniority. Arterioscler Thromb Vasc Biol. 2007. 27:671–676.
11. Ozkan S, Akay TH, Gultekin B, et al. Atherosclerosis of radial and internal thoracic arteries used in coronary bypass: atherosclerosis in arterial grafts. J Card Surg. 2007. 22:385–389.
12. Burris N, Schwartz K, Tang CM, et al. Catheter-based infrared light scanner as a tool to assess conduit quality in coronary artery bypass surgery. J Thorac Cardiovasc Surg. 2007. 133:419–427.
13. Kobayashi H, Kitamura S, Kawachi K, Morita R, Konishi Y, Tsutsumi M. A pathological and biochemical study of arteriosclerosis in the internal thoracic artery, a vessel commonly used as a graft in coronary artery bypass surgery. Surg Today. 1993. 23:697–703.
14. Singh RA, Sosa JA, Green GE. Long-term fate of the internal mammary artery and saphenous vein graft. J Thorac Cardiovasc Surg. 1983. 86:359–363.
15. Sims FH. A comparison of coronary and internal mammary arteries and implications of the results in the etiology of arteriosclerosis. Am Heart J. 1983. 105:560–566.
16. Sperti G, Manasse E, Kol A, et al. Comparison of response to serotonin of radial artery grafts and internal mammary grafts to native coronary arteries and the effect of diltiazem. Am J Cardiol. 1999. 83:592–596.
17. Segarra G, Medina P, Vila JM, et al. Contractile effects of arginine analogues on human internal thoracic and radial arteries. J Thorac Cardiovasc Surg. 2000. 120:729–736.
18. Van Son JA, Smedts F, Vincent JG, van Lier HJ, Kubat K. Comparative anatomic studies of various arterial conduits for myocardial revascularization. J Thorac Cardiovasc Surg. 1990. 99:703–707.
19. Tatoulis J, Buxton BF, Fuller JA, Royse AG. Total arterial coronary revascularization: techniques and results in 3,220 patients. Ann Thorac Surg. 1999. 68:2093–2099.
20. Souza DS, Johansson B, Bojö L, et al. Harvesting the saphenous vein with surrounding tissue for CABG provides long-term graft patency comparable to the left internal thoracic artery: results of a randomized longitudinal trial. J Thorac Cardiovasc Surg. 2006. 132:373–378.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download