Abstract
We report a case of a 46-year-old woman who presented with subacute exertional dyspnea and severe hypoxia. A large cystic mass compressing the right side of the heart along with right-to-left atrial shunt flow through an alleged atrial septal defect (ASD) were detected on echocardiography. CT scan of the chest and MRI of the heart revealed a loculated cystic mediastinal mass with hemorrhage measuring 5.5×8 cm compressing the right atrium and ventricle. The patient underwent cyst resection and primary closure of the ASD. This report illustrates a case of an unusual symptomatic pericardial mass compressing the right atrium and ventricle in a patient with an secundum ASD.
Pericardial masses usually do not cause any symptoms, and come to medical attention as an incidental finding on chest imaging modalities. This is a report on a case of an unusual symptomatic pericardial mass-like lesion in a patient with an secundum atrial septal defect (ASD). As a result of the compression of the right side of the heart, severe right to left shunting of blood developed through the ASD. The patient presented with sub-acute hypoxia, exertional dyspnea and reactive erythrocytosis similar to those in patients with Eisenmenger's syndrome.
A 46-year-old woman who had undergone peripheral stem cell transplantation for acute undifferentiated leukemia 1.5 years ago was admitted for operation of graft-versus-host disease of the eye. Prior to the operation, markedly decreased SaO2 and PaO2 were noted and hence a comprehensive re-evaluation of her medical problems was performed.
The patient's echocardiogram before undergoing the peripheral stem cell transplantation had revealed a small secundum ASD with left-to-right shunt accompanied with mild right atrial enlargement and mild tricuspid regurgitation (Fig. 1). The surgery for ASD had been planned after completion of the treatment for leukemia.
When the patient was admitted for the eye operation, she presented with severe hypoxia (SaO2 79.8%, Qp/Qs 0.87) and subacute dyspnea on exertion. On physical examination, mild cyanosis of the lips and tachycardia were noted and no other specific findings could be found. Peripheral blood smear showed erythrocytosis as a result of the prolonged hypoxemia. But despite oxygen replacement, hypoxia could not be corrected. Her electrocardiogram revealed sinus tachycardia. The follow-up echocardiogram 1.5 years after the initial echocardiogram revealed a huge pericardial mass which was compressing the right atrium and ventricle almost completely (Fig. 2A). Using contrast echocardiography, the extra-cardiac mass and compression of the right side of the heart due to it could be clearly delineated (Fig. 2B). No flow was seen between the mass and the heart or the vascular structures, and the direction of the shunt flow through the ASD had changed from left-to-right to right-to-left due to increased intra-cardiac pressure in the right side of the heart as a result of the external compression (Fig. 2C). Chest CT and MRI of the heart showed a loculated cystic mediastinal mass with hemorrhage measuring 5.5×8 cm compressing the right atrium and ventricle. Axial T2 weighted MR image showed a dark fluid-fluid level within the dependent portion of the mass (Fig. 3C).
Resection of the pericardial cystic mass and primary closure of the ASD were performed. The cyst was firmly adherent to the anterior epicardium of the right side of the heart and was filled with brownish fluid resembling the fluid inside an old hematoma. The right atrium and ventricle were collapsed due to external compression (Fig. 4B). The diagnosis of an organizing hematoma with thick fibrotic walls was confirmed on biopsy. After the removal of this cystic mass, there was normalization of the right ventricular size and no remnant shunt flow was seen on follow-up echocardiography. On follow-up arterial blood gas analysis, SaO2 and PaO2 were normalized and the patient did not have any signs and symptoms of congestive heart failure such as dyspnea or cyanosis.
This is an unusual case of a rare complication of a pericardial cystic mass-which was initially thought to be a primary pericardial cyst or a thymic cyst that had developed following chemotherapy-where severe hypoxia was developed in a subject with ASD. Most primary pericardial cysts are congenital anomalies. Other less common causes include benign thymic, bronchogenic, enteric and thoracic duct cyst as well as malignant cysts of thyroid, parathyroid, lymphoma, thymomas, teratoma and seminoma.1)2) There has been a report on development of a benign thymic cyst in the anterior mediastinum following chemotherapy for non-Hodgkin's lymphoma.3)
A rare cause of a pericardial cystic mass is an acute or chronic cystic hematoma as in the case presented here. Pericar-dial cystic masses are usually asymptomatic and found incidentally on routine chest X-rays. The clinical presentation described includes chest pain, tachycardia, persistent cough, dyspnea, cardiac arrhythmia and lower respiratory tract infection.4-9) The symptoms can result from the pressure of the mass on the adjacent organs.11) The pericardial masses have also been associated with multiple complications including right ventricular outflow tract obstruction, pulmonary stenosis related to extrinsic compression, torsion of a vascular pedi-cle, subsequent development of ischemia-related lesion of the cyst, spontaneous internal hemorrhage and tamponade, partial erosion into the superior vena cava or the anterior wall of the right ventricle. These masses can lead to constrictive pericarditis and congestive heart failure, but it is unknown whether a particular size or position of the cyst corresponds with a higher rate of complications.5)6)11-13) In the present case, the pericardial cystic mass became large enough to compress the right side of the heart and cause a rare complication due to the reversal of the direction of the shunt flow through the ASD.
The direction and magnitude of the shunt through ASDs are determined by the size of the defect and the relative compliance of the ventricles. As a rule, left atrial blood is shunted to the right atrium in the early phase of the disease. Most patients with ASD will have impaired exercise tolerance and exertional dyspnea, but these symptoms may be well compensated for years. If the right ventricle fails or its compliance declines, the left-to-right shunting diminishes in magnitude and right-to-left shunting may occur.14) In the present case, the change in direction of the shunt flow developed due to increased pressure in the right side of the heart due to extra-cardiac compression as a result of increased size of the pericardial cystic mass. As a result, persistent hypoxia and cyanosis developed, which could be corrected by the resection of the cystic mass.
Pericardial organizing hematoma can be subject to internal hemorrhage and consequent growth in size as seen in the present case. As a result, our case presented with reversal in the direction of the shunt flow through the ASD from left-to-right to right-to-left. But even in other cases without any accompanying abnormalities of the heart, the heart can be compressed due to external pressure resulting in a decrease in the cardiac output and deterioration of the patient's health. Hence, the knowledge of such likely complications, especially in cases of hematologic malignancies such as acute leukemia, is crucial for early detection and curative treatment.
Figures and Tables
Fig. 1
Initial echocardiogram. Apical four-chamber view is showing an atrial septal defect (A and B). On color doppler echocardiogram, the direction of the shunt flow through the septal defect is shown to be left-to-right.
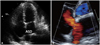
Fig. 2
Follow-up echocardiogram. A: in apical four-chamber view, the pericardial cyst is compressing the right side of the heart (*) almost completely. B: contrast echocardiogram demonstrating the pericardial cyst compressing the right atrium and ventricle (*). Cystic mass does not show enhancement of contrast. C: color doppler echocardiogram showing a huge pericardial cyst and an atrial septal defect. The direction of the shunt flow (white arrow) through the septal defect is shown to be right-to-left.

Fig. 3
Chest CT and MRI of the heart. Coronal view of chest CT (A) shows a cystic lesion in the right pericardial space. A short axis cine image view (B) demonstrates a compressed right ventricle (*) and an intact left ventricle. There is no communication between the mass and the heart. Axial T2-weighted view (C) shows a dark fluid-fluid level within the dependent portion of the mass.

References
1. Koshy T, Sinha PK, Misra S, Unnikrishnan M. Pericardial cyst. Ann Card Anaesth. 2008. 11:129–130.
2. Modi S, Chenzbraun A, Fewins H, Binukrishnan S, Ramsdale DR. Giant asymptomatic pericardial cyst. J Cardiovasc Med (Hagerstown). 2009. 10:646–648.
3. Borgna-Pignatti C, Andreis IB, Rugolotto S, Balter R, Bontempini L. Thymic cyst appearing after treatment of mediastinal non-Hodgkin lymphoma. Med Pediatr Oncol. 1994. 22:70–72.
4. Elamin WF, Hannan K. Pericardial cyst: an unusual cause of pneumonia. Cases J. 2008. 1:26.
5. Tanoue Y, Fujita S, Kanaya Y, Tominaga R. Acute cardiac tamponade due to a bleeding pericardial cyst in a 3-year-old child. Ann Thorac Surg. 2007. 84:282–284.
6. Borges AC, Gellert K, Dietel M, Baumann G, Witt C. Acute right-sided heart failure due to hemorrhage into a pericardial cyst. Ann Thorac Surg. 1997. 63:845–847.
7. Bandeira FC, de Sa VP, Moriguti JC, et al. Cardiac tamponade: an unusual complication of pericardial cyst. J Am Soc Echocardiogr. 1996. 9:108–112.
8. Ogah OS, Akisanya CO, Timeyin AO, Adebiyi AA, Adebo OA. A large pericardial cyst presenting with severe chest pain: a case report and review of literature. Afr J Med Med Sci. 2009. 38:83–86.
9. Chopra PS, Duke DJ, Pellett JR, Rahko PS. Pericardial cyst with partial erosion of the right ventricular wall. Ann Thorac Surg. 1991. 51:840–841.
10. Lesniak-Sobelga AM, Olszowska M, Tracz W, et al. Giant pericardial cyst compressing the right ventricle. Ann Thorac Surg. 2008. 85:1811.
11. Komodromos T, Lieb D, Baraboutis J. Unusual presentation of a pericardial cyst. Heart Vessels. 2004. 19:49–51.
12. Lee JA, Kim BS, Cho HJ, et al. A case of constrictive pericarditis with localized pericardial effusion simulating a cystic mass. Korean Circ J. 1991. 21:791–796.
13. Jin KH, Lee WS, Lee IK, Kim KS, Kim YN, Kim KB. Pericardial cysts: three cases report. Korean Circ J. 1987. 17:795–801.
14. Brickner ME, Hillis LD, Lange RA. Congenital heart disease in adults: second of two parts. N Engl J Med. 2000. 342:334–342.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download