Abstract
Background and Objectives
Morning hypertension is closely related to target organ damage and cardiovascular events. Little data is available concerning the baseline characteristics and comprehensive blood pressure analysis of hypertensive patients on treatment with morning hypertension.
Subjects and Methods
We evaluated 1,087 hypertensive patients who had taken stable anti-hypertensive medication at least 6 months. The enrolled patients measured their home blood pressure for 7 days. Baseline characteristics and the laboratory data were analyzed. Morning hypertension was defined as a morning blood pressure ≥135/85 mm Hg and systolic or diastolic blood pressure difference between morning and evening exceeding 10 mm Hg.
Results
One hundred seventy three patients with morning hypertension showed a preponderance of males, older patients, alcohol consumers, and greater waist circumference and waist-to-hip ratio despite the same body mass index. Impaired fasting glucose and metabolic syndrome were more prevalent in the patients with morning hypertension. The morning hypertensives took more anti-hypertensive drugs and displayed higher blood pressure in the clinic and at home.
Conclusion
The worse clinical variables and relatively poorly controlled blood pressure of those with morning hypertension supports a potential relationship of morning hypertension with poor cardiovascular outcome. Morning blood pressure should be monitored at home for the optimal treatment of hypertension.
Critical cardiovascular events frequently occur in the morning, especially just after awakening. This phenomenon is closely related with the circadian variation of blood pressure (BP) and the excessive elevation of BP in the morning.1)2) Numerous reports have advocated that this so-called morning hypertension (MH) is closely related to target organ damage and the risk of cardiovascular events.3-14)
While the prognostic value of MH is very well-known, little is known about the baseline characteristics of those who experience MH and its clinical implications. Old age, male gender, regular consumption of alcohol, more pronounce use of diverse types of antihypertensive drugs, greater use of beta-blockers and higher BP measured at the clinic were major determinants of the difference in BP between morning and evening in the Jichi Morning Hypertension Research study, in which BP was self-measured at home.15)16) Older age, male preponderance, regular alcohol consumption and BP measurement after bathing at night have been suggested as important determinants of the exaggerated difference in morning and evening home BP.17) Patients with metabolic syndrome have a higher prevalence of MH.18) Another study using ambulatory blood pressure monitoring showed that morning BP surge was associated with old age, elevated fasting plasma glucose and higher 24-hour systolic BP.19)
Comprehensive analysis of BP profiles in MH patients has rarely been done and the relationship between MH and other abnormal home BP categories, such as masked hypertension or uncontrolled hypertension, is still unclear. To address these knowledge shortfalls, the present cross-sectional and observational study was performed in a multi-center manner. The study aimed to evaluate the baseline characteristics of the patients with MH and to analyze their office and home BP profiles. The goal was to ascertain whether MH could be a new target in the treatment of hypertension.
The protocol of this cross-sectional, observational study was approved by the Institutional Review Boards of the participating institutions. We evaluated 1,087 hypertensive patients >18-years-of-age using self-measured home BP in the morning and evening. The patients were recruited from nine university hospitals in Korea that are part of the Hypertension Research Network. Participants had maintained stable anti-hypertensive medications at least for the previous 6 months. Clinical information about the subjects (e.g., age, sex, body weight, height, waist circumference, hip circumference, current medications, social, familial and past medical history) and laboratory data (e.g., C-reactive protein, lipid profiles, serum glucose and serum creatinine) were analyzed.
Physicians and well-trained nurses educated the patients how to measure and record home BP. After verifying their home BP measuring capability, patients were asked to measure their own BP once in the morning and once in the evening. The morning measurement was taken while in a sitting position, within 1 hour after awakening, before taking anti-hypertensive medication, before breakfast meal and after more than 2 minutes of rest. The evening measurement was taken in a sitting position, 1 hour before going to bed and after more than 2 minutes of rest, as specified by the Japanese guidelines for home BP measurement.20) Each subject was requested to obtain two consecutive measurements; if the difference of those values exceeded 10 mm Hg, BP was checked again and the second and third values were analyzed. BPs and pulse rates were recorded for 7 days and all measurements (≥20) were analyzed. The sphygmomanometer used in this study was a model HEM-747 cuff oscillometric device (Omron Healthcare, Kyoto, Japan).
Office BP and pulse rate were measured twice consecutively by physicians while the subject was in a sitting position after at least 2 minutes of rest. The same cuff oscillometric device model used for the home measurements was used.
MH was defined as a morning-evening systolic or diastolic BP difference exceeding 10 mm Hg. Morning BP was defined as a pressure ≥135/85 mm Hg. In cases where systolic or diastolic BP was in a different category, the higher category was applied. Four potential groups were suggested based on hospital BP (140/90 mm Hg) and home BP (135/85 mm Hg) levels: controlled hypertension (no hypertension in hospital and at home), white-coat hypertension (hypertension in hospital but not at home), masked hypertension (no hypertension in hospital but hypertension at home) and uncontrolled hypertension (hypertension in hospital and at home). White coat effect was defined as a difference of office and home BP. Optimal goal of BP control was considered to be <140/90 mm Hg in the office BP and <135/85 mm Hg in the home BP. In patients with diabetes mellitus (DM), the BP goal was <130/80 mm Hg both in the office and at home. Metabolic syndrome was categorized according to National Cholesterol Education Program Adult Treatment Panel Guideline III criteria (for obesity, a waist circumference >90 cm in males and >80 cm in females).
We organized a registry from the demographic, laboratory data and the BP profiles of the enrolled patients. The variables were compared between the MH patients and the non-MH patients. Intergroup comparisons of the baseline demographics and the clinical characteristics were performed using χ2-test, Fisher's exact test, t-test and linear by linear association. BP profiles were analyzed with t-test and analysis of variance. A p<0.05 was considered statistically significant. All of the data were expressed as mean±standard deviation unless otherwise stated. The software package Statistical Package for the Social Sciences (SPSS) 17.0 for Windows (SPSS, Chicago, IL, USA) was used for the statistical analyses.
Hypertensive patients (n=1,087, mean age 56.9±9.6 years, 519 males) taking anti-hypertensive medication were evaluated. One hundred seventy three patients (15.9%) met the definition of MH. The prevalence of controlled hypertension, white-coat hypertension, masked hypertension and uncontrolled hypertension was 38.2% (n=415), 23.5% (n=255), 11.2% (n=122) and 27.1% (n=295), respectively. Mean office systolic/diastolic BP was 138.5±15.9/82.7±10.5 mm Hg and mean home systolic/diastolic BP was 130.1±13.9/81.0±9.7 mm Hg in the morning and 127.3±13.5/77.4±9.7 mm Hg in the evening. The average home systolic/diastolic BP was 128.7±12.8/79.2±9.2 mm Hg. One hundred seventy eight patients (16.3%) were diagnosed with DM and 512 patients (47.0%) were categorized with metabolic syndrome.
The patients with MH were mainly male (56.6% vs. 46.1%, p=0.011), greater consumers of alcohol (49.7% vs. 35.9%, p=0.001) and had greater waist circumference (88.9±8.4 cm vs. 87.3±8.4 cm, p=0.026) and waist-to-hip ratio (90.2±5.1% vs. 88.9±5.6%, p=0.004) despite having the same body mass index (BMI; 25.2±3.0 vs. 25.1±2.9, p=0.512). Laboratory data were comparable in the two groups. Patients with MH took more classes of antihypertensive drugs (2.11±0.88 vs. 1.96±0.87, p=0.038). There was no significant difference of overall drug use between two groups (Table 1).
Metabolic syndrome was more prevalent in all enrolled patients than in the general population (n=512; 47.0% in study participants vs. 24.1% in Korean general population21)) and MH patients showed a higher prevalence of metabolic syndrome (59.5% vs. 49.5%, p=0.019) (Table 2). Laboratory data including fasting glucose and lipid profiles were comparable in the two groups and there was no difference in DM status (p=0.564). However, when impaired fasting glucose (IFG) was included, the composite of DM and IFG were more prevalent in the patients with MH (37.4% vs. 28.8%, p=0.024). MH patients had more metabolic components (p=0.049) (Fig. 1).
There was no significant difference of major risk factors for cardiovascular disease in two groups except age (p=0.021) (Table 3). But, the number of major risk factors showed an increasing tendency in the MH group (p=0.076). We evaluated the incidence of target organ damage related to hypertension. Target organ damages included left ventricular hypertrophy, angina, prior myocardial infarction, prior percutaneous coronary intervention and heart failure in the cardiovascular system, stroke and transient ischemic attack in cerebrovascular system, DM nephropathy and renal insufficiency (estimated glomerular filtration rate <60 mL/min, serum creatinine >1.5 mg/dL in males and >1.3 mg/dL in females) and proteinuria >300 mg over 24 hours in the renal system. There was a tendency of higher prevalence of target organ damage to kidney (p=0.068) in MH patients, but the prevalence of target organ damage in the cardiovascular and cerebrovascular systems was comparable in the two groups.
There was a significant difference in the distribution of BP categories between the MH and non-MH groups. MH patients showed higher prevalence of uncontrolled hypertension and masked hypertension (51.4% and 15.6%, respectively) compared with non-MH patients (22.5% and 10.4%, same respective order), while they showed lower prevalence of controlled hypertension (13.3% for MH vs. 42.9% for non-MH) (Fig. 2A). MH comprised 5.5% of all controlled hypertension and 13.3%, 23.1% and 30.2% of white-coat, masked and uncontrolled hypertension, respectively (Fig. 2B). Almost all masked hypertension and uncontrolled hypertension (96.7% and 94.9%, respectively) showed high morning BP (>135/85 mm Hg), whereas only 76.2% of masked hypertension and 79% of uncontrolled hypertension showed high evening BP (>135/85 mm Hg) (Fig. 2C).
Comparing office BP in both groups, both systolic and diastolic BP was higher in the patients with MH despite comparable pulse rate. When analyzing home BP, morning systolic and diastolic BP, evening systolic BP, average systolic and diastolic BP were significantly higher in the MH group. But, when calculating the BP difference of the two groups, the morning BP difference was significantly higher than the evening BP difference (Table 4). Comparing home BP profile between the MH and non-MH groups in the subgroup of controlled hypertension, white-coat hypertension, masked hypertension and uncontrolled hypertension revealed results were similar to the previous findings (Supplementary appendix 1).
If we set up the goal of controlling BP as a BP <140/90 mm Hg in the office <135/85 mm Hg at home, significantly fewer MH subjects than non-MH subjects achieved the office target (28.9% vs. 53.3%, respectively) and the home target (32.9% vs. 67.1%, respectively) (Supplementary appendix 2). Similar results were observed in the diabetic subset of subjects.
Morning rise of BP, high morning BP itself and the difference of morning-evening BP have been noted as predictors of target organ damage and cardiovascular events. As there is no consensus of home BP levels for the definition of hypertension, we used the cut-off values (≥135/85 mm Hg) for MH as proposed by the American Hypertension Society22) and added the significance of morning-evening BP difference (≥10 mm Hg).
We demonstrated that MH detected by home BP monitoring was related to old age, higher proportion of male and greater consumption of alcohol, similar to previous studies.15-17) MH was related to perilous clinical variables such as higher waist circumference, waist-to-hip ratio and IFG. Patients with MH had more major cardiovascular risk factors, higher prevalence of metabolic syndrome, higher BP profiles and took more drugs for BP control. These observations are consistent with a potential relationship of MH and poor cardiovascular outcome. In the 2007 ESH-ESC practice guidelines for the management of arterial hypertension, it was opined that all patients should be classified not only in relation to the grades of hypertension but also in terms of the total cardiovascular risk resulting from the coexistence of different risk factors, organ damage and disease.23) The guidelines defined the factors influencing prognosis as including age (male >55 years, female >65 years), smoking, dyslipidemia, IFG and abdominal obesity. Patients with metabolic syndrome, target organ damage or DM were regarded as having three or more risk factors, which indicated at least a moderate-to-high added risk even in normotensives. In our study, the patients with MH had these risk factors more frequently and the prevalence of metabolic syndrome was higher. That means MH should be treated more aggressively. Therefore, MH could be a new therapeutic target for preventing target organ damage and subsequent cardiovascular events in hypertensive patients.
When we calculated the BP difference between MH and non-MH subjects, morning BP difference was significantly higher than evening BP difference in the former. The difference of average home BP between the two groups was mainly due to the morning BP difference and not the evening BP difference. In the subgroup analysis of controlled hypertension, the MH group displayed a higher average home BP, although it was within the normal range. The morning BP difference was expected, despite comparable office BP. In this study, 30.2% of uncontrolled hypertension and 23.1% of masked hypertension involved MH subjects, whereas only 5.5% of subjects with controlled hypertension had MH. These observations likely reflect the fact that the home BP of the patients with MH had been relatively poorly controlled. Put another way, MH carries a greater likelihood of masked hypertension or uncontrolled hypertension, attributable to morning BP difference despite comparable evening BP.
These observations indicate that although several guidelines recommended that home BP should be measured both in the morning and in the evening,24) if it is difficult to measure BP twice per day, morning BP is likely more informative than evening BP. As is apparent in Fig. 2C, scrutiny of only evening BP could miss an appreciable portion of cases of uncontrolled hypertension (21%) and masked hypertension (24%). But, measuring BP once daily in the morning detects 95% of uncontrolled hypertension and 97% of masked hypertension. These results clearly indicate that, if it is impossible to check BP twice a day, BP measurement should be performed in the morning. Of course, MH subjects might have more cardiovascular risk factors as a result of their poorly controlled BP, but the fact that masked hypertension and uncontrolled hypertension, which have poor cardiovascular outcome, are more frequent in MH, is important per se.
Defining evening hypertension as a difference in systolic or diastolic BP between morning and evening of >10 mm Hg with the condition that the evening BP is ≥135/85 mm Hg, reveals that, similar to MH, subjects with evening hypertension less frequently display uncontrolled hypertension than MH (44.0% vs. 51.4%), and do not show significant difference in cardiovascular risk factors that tend to be more frequent in MH (e.g., higher waist circumference, waist-to-hip ratio, more frequent IFG, metabolic syndrome and use of more antihypertensive medications) compared to non-evening hypertension group.
The management of hypertension guided by the morning BP level might achieve an additional benefit by modifying cardiovascular risk. Morning BP should be monitored at home as a first step in the treatment of hypertension and the needs for more effective, long-acting antihypertensive therapy or drug prescriptions that consider pharmacokinetics and chronobiology can be magnified.
In this study, even among well-controlled hypertensives, 10.8% (46 patients) showed high morning BP (≥135/85 mm Hg). Several recent studies reported that patients with or without hypertension had the same 24-hour pattern of onset of cardiovascular events.2)3) These data strengthen the suggestion that high BP in the morning may also be harmful for normotensive subjects, and that MH may be crucial in cardiovascular events irrespective of the existence of hypertension. An accurate evaluation of MH and its treatment might be useful for controlled hypertensives as well, so morning BP should be monitored to diagnose undetected MH even in hypertensives who appear to be well-controlled in the clinic.
The cross-sectional and observational nature of our study imposed limitations. The study findings were insufficient to clarify whether MH is a unique form of hypertension or a consequence of undertreatment. Although the participants had been on a stable antihypertensive medication without any change for at least for 6 months and data on prescribed drug classes were available, we could not obtain a specific drug regimen considering a chronobiological effect (administered doses or dosing schedules). So, there is the possibility of a confounding effect of anti-hypertensive medications. Elevated morning BP level includes two different types of BP variation: nocturnal hypertension (such as non-dippers) and morning surge type.25) We could not distinguish between these types using conventional home BP devices. In this study, we could not prove the direct inter-relationship between MH and CV risk or TOD, maybe due to the relatively short follow-up period. The patients with MH were related to worse prognostic factors, but they could not be generalized to worsened cardiovascular outcome in the absence of long-term clinical follow-up and event analysis in our data. Despite the large number of participants, it is difficult to generalize the present findings to the general population, because this study was conducted in a hospital-based manner.
MH in treated hypertensives is more likely seen among patients who are male, older and more often consume alcohol. MH is related to worsened clinical variables such as higher waist circumference, higher waist-to-hip ratio, IFG and higher BP. So, a potential relationship of MH and poor cardiovascular outcome can be suggested. Home BP monitoring is essential for the treatment of hypertension and the patients with MH should be treated more vigorously for preventing unfavorable cardiovascular outcome in the future. Conduction of a large sized longer clinical follow-up trial is essential to clarify the clinical significance of MH.
Figures and Tables
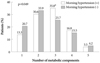 | Fig. 1The number of metabolic components in patients with morning hypertension showed increasing tendency (p=0.049). *The peak incidence in morning hypertensives was higher. |
 | Fig. 2The distribution of hypertensive patients is significantly different. A: the patients with morning hypertension showed higher prevalence of uncontrolled hypertension and masked hypertension and lower prevalence of controlled hypertension compared with the patients without morning hypertension. B: morning hypertension occupying much higher proportion in masked hypertension and uncontrolled hypertension. C: in the patients with masked hypertension or uncontrolled hypertension, there was a tendency to have high morning blood pressure. HT: hypertension. |
Table 2
The prevalence of metabolic syndrome and each metabolic component in patient with or without morning hypertension
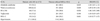
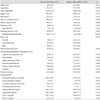
Table 3
Major risk factors of cardiovascular disease in patients with or without morning hypertension

Acknowledgments
This work was supported by the research grant of the Chungbuk National University in 2009.
References
1. Manfredini R, Gallerani M, Portaluppi F, Fersini C. Relationships of the circadian rhythms of thrombotic, ischemic, hemorrhagic, and arrhythmic events to blood pressure rhythms. Ann N Y Acad Sci. 1996. 783:141–158.
2. Giles TD. Circadian rhythm of blood pressure and the relation to cardiovascular events. J Hypertens Suppl. 2006. 24:S11–S16.
3. Ohkubo T, Imai Y, Tsuji I, et al. Prediction of mortality by ambulatory blood pressure monitoring versus screening blood pressure measurements: a pilot study in Ohasama. J Hypertens. 1997. 15:357–364.
4. Asayama K, Ohkubo T, Kikuya M, et al. Prediction of stroke by home "morning" versus "evening" blood pressure values: the Ohasama Study. Hypertension. 2006. 48:737–743.
5. Kario K, Ishikawa J, Pickering TG, et al. Morning hypertension: the strongest independent risk factor for stroke in elderly hypertensive patients. Hypertens Res. 2006. 29:581–587.
6. Kario K, Pickering TG, Umeda Y, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation. 2003. 107:1401–1406.
7. Gosse P, Cipriano C, Bemurat L, et al. Prognostic significance of blood pressure measured on rising. J Hum Hypertens. 2001. 15:413–417.
8. Gosse P, Lasserre R, Minifié C, Lemetayer P, Clementy J. Blood pressure surge on rising. J Hypertens. 2004. 22:1113–1118.
9. Polónia J, Amado P, Barbosa L, et al. Morning rise, morning surge and daytime variability of blood pressure and cardiovascular target organ damage: a cross-sectional study in 743 subjects. Rev Port Cardiol. 2005. 24:65–78.
10. Marfella R, Siniscalchi M, Nappo F, et al. Regression of carotid atherosclerosis by control of morning blood pressure peak in newly diagnosed hypertensive patients. Am J Hypertens. 2005. 18:308–318.
11. Ikeda T, Gomi T, Shibuya Y, et al. Morning rise in blood pressure is a predictor of left ventricular hypertrophy in treated hypertensive patients. Hypertens Res. 2004. 27:939–946.
12. Shibuya Y, Ikeda T, Gomi T. Morning rise of blood pressure assessed by home blood pressure monitoring is associated with left ventricular hypertrophy in hypertensive patients receiving long-term antihypertensive medication. Hypertens Res. 2007. 30:903–911.
13. Ishikawa J, Hoshide S, Shibasaki S, et al. Relationship between morning hypertension identified by home blood pressure monitoring and brain natriuretic peptide and estimated glomerular filtration rate: the Japan Morning Surge 1 (JMS-1) Study. J Clin Hypertens (Greenwich). 2008. 10:34–42.
14. Kamoi K, Miyakoshi M, Soda S, Kaneko S, Nakagawa O. Usefulness of home blood pressure measurement in the morning in type 2 diabetic patients. Diabetes Care. 2002. 25:2218–2223.
15. Ishikawa J, Kario K, Eguchi K, et al. Regular alcohol drinking is a determinant of masked morning hypertension detected by home blood pressure monitoring in medicated hypertensive patients with well-controlled clinic blood pressure: the Jichi Morning Hypertension Research (J-MORE) Study. Hypertens Res. 2006. 29:679–686.
16. Ishikawa J, Kario K, Hoshide S, et al. Determinants of exaggerated difference in morning and evening blood pressure measured by self-measured blood pressure monitoring in medicated hypertensive patients: Jichi Morning Hypertension Research (J-MORE) Study. Am J Hypertens. 2005. 18:958–965.
17. Kawabe H, Saito I. Determinants of exaggerated difference in morning and evening home blood pressure in Japanese normotensives. Hypertens Res. 2009. 32:1028–1031.
18. Tamaki S, Nakamura Y, Yoshino T, et al. The association between morning hypertension and metabolic syndrome in hypertensive patients. Hypertens Res. 2006. 29:783–788.
19. Shimizu M, Ishikawa J, Eguchi K, Hoshide S, Shimada K, Kario K. Association of an abnormal blood glucose level and morning blood pressure surge in elderly subjects with hypertension. Am J Hypertens. 2009. 22:611–616.
20. Imai Y, Otsuka K, Kawano Y, et al. Japanese society of hypertension (JSH) guidelines for self-monitoring of blood pressure at home. Hypertens Res. 2003. 26:771–782.
21. Lim S, Lee EJ, Koo BK, et al. Increasing trends of metabolic syndrome in Korea-based on Korean National Health and Nutrition Examination Surveys. J Korean Diabetes Assoc. 2005. 29:432–439.
22. Pickering T. Recommendations for the use of home (self) and ambulatory blood pressure monitoring: American Society of Hypertension Ad Hoc Panel. Am J Hypertens. 1996. 9:1–11.
23. Mancia G, De Backer G, Dominiczak A, et al. 2007 ESH-ESC Practice Guidelines for the Management of Arterial Hypertension: ESH-ESC Task Force on the Management of Arterial Hypertension. J Hypertens. 2007. 25:1751–1762.
24. Mengden T, Chamontin B, Phong Chau N, Luis Palma Gamiz J, Chanudet X. User procedure for self-measurement of blood pressure: First International Consensus Conference on Self Blood Pressure Measurement. Blood Press Monit. 2000. 5:111–129.
25. Kario K, White WB. Early morning hypertension: what does it contribute to overall cardiovascular risk assessment? J Am Soc Hypertens. 2008. 2:397–402.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download