Abstract
Background and Objectives
The drug-eluting balloon (DEB) catheter system was developed to treat restenosis. Furthermore, DEB angioplasty has been shown to reduce restenosis risk when compared to drug-eluting stents (DES) in patients with in-stent restenosis (ISR) or small vessel disease (SVD). In addition, DEB angioplasty reduces costs due to fewer revascularizations and reduced clopidogrel treatment length. The objective of this study was to predict the expected cost-savings when DEB is substituted for DES in patients with ISR or SVD.
Subjects and Methods
The subjects included were patients treated by DES at Seoul National University Hospital from January 2006 to June 2009, with clinical data after percutaneous coronary intervention, were. A model was developed to allow the costs of DES and the calculated costs of DEB incurred by patients with ISR or SVD to be compared. The overall cost of DEB was calculated to be 1,256,150 won and the overall cost of DES was 2,102,500 won, and the cost of clopidogrel was 2,168 won. Expected repeat revascularizations within 12 months of DEB were calculated based on information provided by the Paclitaxel-Eluting PTCA-Balloon Catheter in Coronary Artery (PEPCAD) I and II trials.
The introduction of coronary stents was one of the most remarkable clinical developments in the field of interventional cardiology, and although the long-term success of coronary stents is limited by in-stent restenosis (ISR), the incidence of ISR was reduced by 5-35% by the introduction of drug-eluting stents (DESs). But it still remains a significant challenge in ISR lesion and small vessel disease (SVD), and increased expense for our health care system incurred by their high prices and by a high demand of DESs by physicians.1)
DESs are currently considered the best possible device for treating ISR,2)3) but the stent-in-stent approach introduces a metal component intraarterially, thus, reduces the vascular lumen. On the other hand, polymeric coatings on stents containing antiproliferative drugs can induce inflammation and thrombosis,4) and require long-lasting antiplatelet therapy to reduce late thrombotic complications.
Recently, non-stent-based local balloon delivery systems have been developed for the delivery of antiproliferative drugs. The concept behind this technology is that the rapid release of antiproliferative drugs into arterial tissue is more effective than their gradual release, as exemplified by DESs.5)6) Another benefit of drug-eluting balloon (DEB) based technology is that it is potentially cheaper as balloon catheters are invariably cheaper than stents. Furthermore, a clinical trial demonstrated the efficacy of a balloon coated with a paclitaxel-iopromide mixture at inhibiting neointimal proliferation in coronary ISR patients.7) SVD patients are also at elevated risk of needing repeat coronary procedures and also present the health care system with a substantial cost burden.8)9) However, a clinical trial concluded that treatment of SVD with a DEB catheter was well tolerated by patients and that this method may offer an alternative to DES implantation.10)
Furthermore, as compared to DESs, clopidogrel consumption would be significantly reduced by the use of DEBs,11) and reducing the duration of clopidogrel therapy might have clinical advantages in terms of safety, when there are concerns about bleeding or the need for surgical intervention.
Therefore, the use of DEBs may present an alternative treatment option for patients with ISR in any type of coronary artery stent or SVD, although these findings need to be confirmed by longer follow-up studies, and this might be particularly true when there are clinical reasons for minimizing the duration of clopidogrel treatment or when the placement of further stents is not technically feasible.
Evaluations of the usefulness of a new device require a formal assessment of its cost implications, and no such assessment has yet been performed for the treatment of ISR or SVD with DEBs. In this study, we calculated the expected cost-saving associated with the use of DEBs versus DESs in patients with ISR or SVD.
This study was initiated by ourselves, and no third party was involved in the study design, conduct, or analysis. Patients with SVD or ISR and had stable or unstable angina, and who were at least 18 years old, had a positive stress test, and scheduled to undergo PCI in a native coronary artery were considered eligible for this study. ISR was defined as stenosis of ≥50% of the arterial diameter at a stent site in vessels that were 3.0-5.0 mm in diameter with a lesion length of <25 mm in patients who underwent successful (<30% residual stenosis without complications) angioplasty using balloons (alone or in combination), ablative devices, or additional stents. SVD was defined as a lesion involving a de novo coronary artery with a vessel diameter of <2.8 mm. Consecutive patients that underwent DES implantation at Seoul National University Hospital from January 2006 to June 2009 were identified using a cardiology database. Candidates were excluded if follow-up duration was less than 12 months. Finally, 585 patients were included in the study (Fig. 1).
We evaluated potential cost-savings when all 585 study subjects with ISR (n=189) or SVD (n=396) that underwent DES were theoretically converted to DEB. We developed a model to compare the initial costs of DES and DEB for treating ISR (ISR group) and SVD (SVD group) patients: 1) a group was treated with a DES (DES group); and 2) a group was assumed to use DEB (length 17 to 30 mm, diameter 2.5 to 3.5 mm; SeQuent Please, B. Braun Melsungen) (DEB group) instead of DES. We also compared the overall long-term costs of DES and DEB group, respectively, for ISR and SVD group. We supposed the extra costs, except PCI, during admission and follow-up costs between DES and DEB group would be identical. The number of devices used per patient between DES and DEB group was supposed to be the same. All patients were assumed to be on a lifelong prescription of aspirin at ≥100 mg. Clopidogrel (75 mg/day) was administered for 6-12 months after DES, and was presumed to have been administered for 1 month after DEB. Clinical and angiographic follow-ups were performed at least 9 months after initial DES, as is performed routinely at our institution.
We evaluated the frequency of target-lesion revascularization (TLR) during the 12 months following DES. TLR was defined as revascularization of the target lesion in the presence of recurrent angina and/or angiographic findings at follow-up. Expected repeat revascularizations within 12 months of DEB group were calculated based on the findings of The Paclitaxel-Eluting PTCA-Balloon Catheter in Coronary Artery (PEPCAD) I and II trials. In the PEPCAD I trial, of 82 SVD patients with a single de novo lesion in a native small caliber coronary artery, restenosis occurred in 4 (4.9%) during the 12-month period following DEB.10) The PEPCAD II trial was a randomized controlled trial of 131 ISR patients treated by DEB or DES, and reported 12-month TLR rates of 6.3% for DEB and 15.4% for DES.7) In the present study, the costs of repeat revascularizations and of clopidogrel therapy were compared for DEB and DES.
According to the Health Insurance Review & Assessment Service that the cost of DEB is 1,256,150 won, the cost of DES is 2,101,500 won and that the cost of clopidogrel is 2,168 won per tablet.
Coronary angiograms were obtained in a routine manner. All patients received intracoronary isosorbide dinitrate before initial and postprocedural angiograms to achieve maximal vasodilatation. Angiograms were analyzed by an independent angiographer using an automated edge-detection quantitative coronary angiography system (Quantcor QCA version 4.0., Pie Medical Imaging, the Netherlands). Angiographic binary restenosis at follow-up was defined as ≥50% diameter narrowing within the stent and in the adjacent segment including the stent plus its edges (within 5 mm).
Data are expressed as means±SDs for continuous variables and as numbers (%) for categorical variables, as appropriate. Differences between the total cost for patients who underwent DES and the expected total cost for patients had they undergone DEB were compared using the paired t-test for asymmetric distributions, as determined using the Shapiro-Wilk test. Differences between the cost of repeated PCI after DES and the expected cost of repeated PCI after DEB were compared using the non-parametric one sample test.
All statistical analyses were performed using SAS version 9.0 for Windows (SAS, Cary, NC, USA). Significance was accepted for p<0.05.
A total of 1,146 patients, all patients were followed for 12 months, that underwent DES implantation from January 2006 to June 2009 were identified, but 561 were excluded for not meeting the inclusion criteria (ISR or SVD). Accordingly, 585 patients were enrolled in this study; 189 patients had ISR and 396 SVD.
Repeat revascularization for ISR was performed in the 189, 117 patients received a DES and 24 patients received a BMS at initial stent implantation, patients. Patients' mean age was 64.91±9.72 years old, and 34.8% were women. Their baseline characteristics are summarized in Table 1. The pattern of ISR was predominantly focal. Mean duration of antiplatelet therapy with clopidogrel was 258.69±158.93 days. Three patients died during follow-up, but no patient underwent coronary bypass grafting.
The baseline clinical and angiographic characteristics of the 396 SVD patients are shown in Table 2. Mean patient age was 64.11±8.54 years old and 36.6% were women. Mean vessel diameter was 2.45±0.27 mm and lesions were predominantly of type C. Clopidogrel was prescribed for 202.50±85.19 days. Of the 396 patients enrolled, 10 patients myocardial infarctions occurred after DES during follow-up and 3 patients died.
Of the 189 ISR patients, 62 received DES, 104 received a plain balloon, and 93 received a cutting balloon. An average of 0.33 stents/patient was implanted in the DES group. The cost was 2,102,500 won per number of DES at initial enrollment, therefore, the cost of 62 DES was 130,355,000 won (i.e., 62 DES×2,102,500 won per DES) in the DES group and the cost of 62 DEB in the DEB group was 77,881,300 won (p<0.01) (Fig. 2).
The total medical cost of clopidogrel for the 189 ISR patients treated by DES was 97,904,712 won, and for ISR patients treated by DEB with a duration of clopidogrel therapy of 4 weeks, the total medical cost of clopidogrel would have been 12,292,560 won (97,904,712 won versus 12,292,560 won; p<0.01) (Fig. 2).
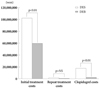
An average of 1.2 DESs per patient were implanted in the SVD group. The cost of DES group at initial treatment was KWR 1,023,735,290 won (i.e., 1.2×2,102,500 won per stent×396 patients), whereas the cost of DEBs in this group was 596,671,250 won (p<0.01) (Fig. 3). Mean duration of clopidogrel antiplatelet therapy was 202.50±85.19 days for patients treated by DES, and clopidogrel cost for these patients was 459,616 won/patient. The total medical costs of clopidogrel for patients treated by DES and DEB were 181,856,176 and 25,755,840 won, respectively (p<0.01), and thus, the expected cost saving for antiplatelet therapy was 156,100,336 won.
Restenosis occurred in 33 of 189 patients with ISR during follow-up. All lesions were treated by plain balloon dilatation, or cutting balloon dilatation. Additional DES was used, as required, to optimize final angiographic results or to cover unstented lesion regions (including edge dissection). Of these 33 patients, 13 received DES, 18 received a plain balloon, and 10 received a cutting balloon. The mean number of DESs used per patient for TLR during the 12-month follow-up was 0.4. The cost of 13 DES was 27,319,500 won (i.e., 13 DES×2,102,500 won per DES). For repeat PCI performed during follow-up, if DEB was used for initial treatment, we predicted repeat PCI rates after DEB of 6.3% during the subsequent 12 months based on PEPCAD II findings, which meant that 12 of 189 patients would need a repeat PCI. Therefore, the needed number of DEB was 4.8 after 12 months of follow-up in DEB group, and then the cost of 4.8 DEB was 5,938,163 won (i.e., 0.4 DEBs per patient×1,256,150 won per DEB×12 patients). Accordingly, a cost saving of 22,865,878 won was predicted for repeat revascularization.
Angiographically proven ISR was recorded in 24 of the 396 SVD patients at 12 months after DES implantation, a ISR incidence of 6.1%. Of these 24 patients, 8 received a DES, 13 received a plain balloon, and 8 received a cutting balloon. The number of devices used per patient was 1.21 and the mean cost of used devices was 1,738,920 won per patient. An average of 0.33 DESs were implanted in the 396 patients. However, had DEB been used instead, using PEPCAD I findings, revascularization would have occurred in 4.9% with SVD at 12 month, that is, in 19 patients. We assumed that 0.33 DEB would be required by the 19 patients, which equated to a total DEB number of 6.33. Accordingly, the costs of DES and DEB in SVD patients were 16,820,000 and 7,955,616 won, respectively (p=NS) (Fig. 3).
We defined "total cost" to be the sum of initial treatment DES or DEB cost, repeat revascularization cost, and clopidogrel therapy cost over 12 months of follow-up.
The expected total cost of DES treatment for 189 patients was 533,914,452 won and the total cost of DEB treatment was 354,769,296 won (p<0.001), and thus, the use of DEB led to an expected 1-year total cost savings of 179,145,156 won.
Expected total costs of DES and DEB based treatments in the SVD were 1,247,325,556 and 651,305,979 won, respectively, and thus, the expected total cost saving was 596,019,577 won, showing that conversion of the current PCI population from DES to DEB would result in a 48% saving in total costs.
ISR remains a challenge despite the availability of DES. Approximately 25 percent of patients treated with a bare-metal stent and about 10 percent of patients treated with a DES experience an overgrowth of vascular tissue and intrastent renarrowing or ISR.12)13) Treating ISR with a DES is a complex procedure that adds another layer of metal, and thus, can create mechanical problems. Furthermore, polymeric matrixes containing embedded antiproliferative drugs on stents can lead to inflammation and thrombosis.4) For these reasons, DEB may offer a simpler alternative. The balloon is coated with the antimitotic drug paclitaxel to reduce restenosis and has the benefit of a matrix of paclitaxel and a hydrophilic spacer on its surface, which creates a large contact surface area between the lipophilic drug and the vessel wall and increases the bioavailability of the embedded drug and facilitates its rapid drug absorption by the vessel wall (PACCOCATH technology).14) This use of a hydrophilic spacer allows the uniform and complete administration of the drug after first balloon inflation. In addition, to avoiding the introduction of a second metal stent, DEBs also contain iopromide, the commonly used contrast agent, to bind paclitaxel to the balloon.15) This meets concerns about the reactions of arteries to the polymers used to bind paclitaxel and other anti-restenosis medications to DESs. Furthermore, as compared to DES, DEB reduces the duration of clopidogrel administration.11)16)
The complex, vexing problem of restenosis after balloon angioplasty is influenced by a variety of clinical and anatomic factors. Vessel size is an important anatomic factor,17) and in fact, restenosis rate is inversely related to vessel diameter.18) It has been reported that angiographic and clinical outcomes after balloon angioplasty and elective stent placement are best in vessels slightly smaller than 3 mm,19) and regarding the treatment of stenotic coronary arteries with diameters below 3 mm, previous studies have demonstrated the superiority of implanting DES for restenosis reduction as compared to BMS implantation in SVD.20)21) Furthermore, data for DES in SVD shows the benefit of antiproliferative drug, however, DES introduces an another layer of metal to a small vessel, and thus, reduces available vascular lumen. Since none of the above-mentioned options for the percutaneous treatment of SVD seems to be universally recommendable, the DEB catheter is to be considered an alternative. A previous study showed that DEB offers benefit as compared to DES in SVD.10) However, in the PICCOLETO study, DEB failed to show equivalence to DES during PCI in SVD,22) but several aspects of this study were questionable. First, the balloon used (Dior; Eurocor, Bonn, Germany) was not based on PACCOCATH technology, and the cohort was relatively small, and thus, the results obtained did not allow clinical conclusions to be drawn.
Although results of initial DEB studies were good, interventionalists are conservative in their views on potential applications of DEBs in the coronary bed. This study suggested that DEB provided a viable alternative not only for treatment effect but also for cost saving. In the present study, we estimated the cost savings offered by DEB as compared to DES for the treatments of ISR and SVD. The principal finding of this study, based on economic analyses of results by substituting DEB for DES and clinical trials of PEPAD I and II, is that will DEB reduce treatment cost. However, in the present study, we assumed that follow-up costs would be the same, but the reduced requirement for repeat revascularization procedures after DEB treatment would undoubtedly reduce follow-up costs and increase cost savings. We made the assumption that the number of DEB per patient was the same as the number of DES per patient because several DEBs could be required to treat a long lesion.
DEB seems to be helpful in the treatment of ISR or SVD, because it is potentially cheaper and reduces the duration of clopidogrel therapy, and thus, increases safety. Therefore, ISR and SVD may be proper indications for DEB.
In patients with ISR or SVD, the use of DEB may result in significant cost savings as compared to using DES. DEB will reduce the incidence of restenosis, and therefore, the costs associated with subsequent re-intervention for coronary stenoses, and it will reduce the costs of clopidogrel therapy. However, more long-term data is needed to assess the safety and cost-effectiveness of DEB.
Our study has several limitations that should be considered. The major limitation of this study was the introduction of selection bias. Second, the study does not include a DEB case group, and therefore, we adopted a repeated revascularization rate in-line with those determined by comparative clinical trials on the costs of DEB and DES treatments. As a result, the cost difference between DEB and DES group can be changeable in practice. It is not really clear whether this uncertainty leads to cost savings being overestimated or underestimated. And validation of present study model was not approved. Therefore potential value of our analysis was limited. Third, the study is inherently limited by its retrospective, single centre nature. Fourth, the patients enrolled in this study all met the 12-months follow-up criterion, which may limit the generalizability of our results. Fifth, the long-term clinical outcomes after angioplasty with DEB in patients with ISR and SVD are not available yet. Therefore, it may be too early to discuss the cost-effectiveness of DEB compared to DES.
Figures and Tables
Fig. 2
Comparative cost analysis in patients with in-stent restenosis. DES: drug-eluting stent, DEB: drug-eluting balloon.
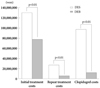
Fig. 3
Comparative cost analysis in patients with small vessel disease. DES: drug-eluting stent, DEB: drug-eluting balloon.
Acknowledgments
The authors would like to thank Nam-Beom Gim for his expert advice on statistics.
This study was supported by a grant from the Center of Ischemic Heart Disease (0412-CR02-0704-0001) sponsored by the Ministry of Health & Welfare, the Republic of Korea.
References
1. Stone GW, Ellis SG, Cannon L, et al. Comparison of a polymer-based paclitaxel-eluting stent with a bare metal stent in patients with complex coronary artery disease: a randomized controlled trial. JAMA. 2005. 294:1215–1223.
2. Iofina E, Haager PK, Radke PW, et al. Sirolimus- and paclitaxel-eluting stents in comparison with balloon angioplasty for treatment of in-stent restenosis. Catheter Cardiovasc Interv. 2005. 64:28–34.
3. Kastrati A, Mehilli J, von Beckerath N, et al. Sirolimus-eluting stent or paclitaxel-eluting stent vs balloon angioplasty for prevention of recurrences in patients with coronary in-stent restenosis: a randomized controlled trial. JAMA. 2005. 293:165–171.
4. Virmani R, Guagliumi G, Farb A, et al. Localized hypersensitivity and late coronary thrombosis secondary to a sirolimus-eluting stent: should we be cautious? Circulation. 2004. 109:701–705.
5. Posa A, Hemetsberger R, Petnehazy O, et al. Attainment of local drug delivery with paclitaxel-eluting balloon in porcine coronary arteries. Coron Artery Dis. 2008. 19:243–247.
6. Cremers B, Speck U, Kaufels N, et al. Drug-eluting balloon: very short-term exposure and overlapping. Thromb Haemost. 2009. 101:201–206.
7. Unverdorben M, Vallbracht C, Cremers B, et al. Paclitaxel-coated balloon catheter versus paclitaxel-coated stent for the treatment of coronary in-stent restenosis. Circulation. 2009. 119:2986–2994.
8. Hong SJ, Ahn TH, Kim MH, et al. Comparison of the predictors of cronary restenosis after drug-eluting stent implantation in diabetic and nondiabetic patients. Korean Circ J. 2007. 37:530–537.
9. Elezi S, Kastrati A, Neumann FJ, Hadamitzky M, Dirschinger J, Schömig A. Vessel size and long-term outcome after coronary stent placement. Circulation. 1998. 98:1875–1880.
10. Unverdorben M, Kleber FX, Heuer H, et al. Treatment of small coronary arteries with a paclitaxel-coated balloon catheter. Clin Res Cardiol. 2010. 99:165–174.
11. Scheller B, Hehrlein C, Bocksch W, et al. Two year follow-up after treatment of coronary in-stent restenosis with a paclitaxel-coated balloon catheter. Clin Res Cardiol. 2008. 97:773–781.
12. Bauters C, Hubert E, Prat A, et al. Predictors of restenosis after coronary stent implantation. J Am Coll Cardiol. 1998. 31:1291–1298.
13. Novack V, Nguyen MC, Rooney M, et al. Effect of coronary target lesion revascularization on late cardiac events after insertion of sirolimus-eluting or bare metal stents. Am J Cardiol. 2010. 106:774–779.
14. Scheller B, Speck U, Abramjuk C, Bernhardt U, Böhm M, Nickenig G. Paclitaxel balloon coating, a novel method for prevention and therapy of restenosis. Circulation. 2004. 110:810–814.
15. Scheller B, Speck U, Romeike B, et al. Contrast media as carriers for local drug delivery: successful inhibition of neointimal proliferation in the porcine coronary stent model. Eur Heart J. 2003. 24:1462–1467.
16. Scheller B, Hehrlein C, Bocksch W, et al. Treatment of coronary in-stent restenosis with a paclitaxel-coated balloon catheter. N Engl J Med. 2006. 355:2113–2124.
17. Lee CW, Park SJ. Predictive factors for restenosis after drug-eluting stent implantation. Korean Circ J. 2007. 37:97–102.
18. Kuntz RE, Safian RD, Carrozza JP, Fishman RF, Mansour M, Baim DS. The importance of acute luminal diameter in determining restenosis after coronary atherectomy or stenting. Circulation. 1992. 86:1827–1835.
19. Savage MP, Fischman DL, Rake R, et al. Efficacy of coronary stenting versus balloon angioplasty in small coronary arteries: Stent Restenosis Study (STRESS) Investigators. J Am Coll Cardiol. 1998. 31:307–311.
20. Ardissino D, Cavallini C, Bramucci E, et al. Sirolimus-eluting vs uncoated stents for prevention of restenosis in small coronary arteries: a randomized trial. JAMA. 2004. 292:2727–2734.
21. Whang YJ, Kim HS, Kim KM, et al. The efficacy of drug eluting stents on restenosis reduction in small coronary arteries. Korean Circ J. 2006. 36:450–457.
22. Cortese B, Micheli A, Picchi A, Coppolaro A, et al. Paclitaxel-coated balloon versus drug-eluting stent during PCI of small coronary vessels, a prospective randomised clinical trial: the PICCOLETO Study. Heart. 2010. 96:1291–1296.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download