Abstract
Various electrocardiography (ECG) abnormalities have been reported in patients who present with pulmonary embolism (PE). Severe sepsis is also associated with ECG changes that may mimic ST elevation myocardial infarction. We report a case of an elderly patient with PE and septic shock associated with striking ECG changes.
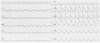
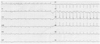
A 92-year-old woman was admitted with acute dyspnea, altered mental status and a 3-day history of fevers and rigors. On arrival, she was febrile, hypotensive and tachycardic. Electrocardiography (ECG) showed multifocal atrial tachycardia and widespread concave ST segment elevation in the precordial and lateral leads (Fig. 1). Bedside echocardiogram revealed a large, free-floating, right atrial thrombus intermittently prolapsing through the tricuspid valve into the right ventricle. Right and left ventricular systolic functions were preserved and no regional wall motion abnormalities (RWMA) were present. Contrast-enhanced CT pulmonary angiogram demonstrated multiple large bilateral pulmonary emboli. She was successfully resuscitated with intravenous colloids, piperacillin/tazobactam, antipyretics and unfractionated heparin infusion. Repeat ECG obtained one hour later revealed persistence tachyarrhythmia but spontaneous resolution of ST segment elevation (Fig. 2). At which point the patient had became afebrile and normotensive, while echocardiographic manifestations remained unchanged. Admission electrolytes were normal and Troponin I peaked at 0.79 ng/dL. Blood and urine cultures isolated a multisensitive strain of Escherichia Coli.
Several ECG changes have been identified in patients with pulmonary embolism (PE).1) Precordial ST segment elevation has been previously described in patients with extensive PE.2)3) However, similar ECG manifestations have been described in patients with severe sepsis and normal coronary arteries.4)5) In our patient, despite the absence of RWMA and significant enzyme increase, acute coronary syndrome, coronary vasospasm and acute myocarditis constituted the differential diagnoses, as coronary angiography and endomyocardial biopsy were not readily available.
References
1. Ryu HM, Lee JH, Kwon YS, et al. Electrocardiography patterns and the role of the electrocardiography score for risk stratification in acute pulmonary embolism. Korean Circ J. 2010. 40:499–506.
2. Goslar T, Podbregar M. Acute ECG ST-segment elevation mimicking myocardial infarction in a patient with pulmonary embolism. Cardiovasc Ultrasound. 2010. 8:50.
3. Lin JF, Li YC, Yang PL. A case of massive pulmonary embolism with ST elevation in leads V1-4. Circ J. 2009. 73:1157–1159.
4. Martinez JD, Babu RV, Sharma G. Escherichia coli septic shock masquerading as ST-segment elevation myocardial infarction. Postgrad Med. 2009. 121:102–105.
5. Terradellas JB, Bellot JF, Sarís AB, Gil CL, Torrallardona AT, Garriga JR. Acute and transient ST segment elevation during bacterial shock in seven patients without apparent heart disease. Chest. 1982. 81:444–448.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download