Abstract
Myocardial infarction is diagnosed when blood levels of biomarkers are increased in the clinical setting of acute myocardial ischemia. Among the biomarkers, troponin I is the preferred biomarker indicative of myocardial necrosis. It is tissue specific for the heart. Myocardial infarction is rarely reported following seizure. We report a case of elevated troponin I in a patient after an episode of generalized tonic-clonic seizure. The diagnosis was type 2 myocardial infarction.
Elevation in cardiac troponin (I or T) reflects myocardial necrosis.1) If there are no other etiologies of myocardial necrosis, such as myocarditis, aortic dissection, pulmonary embolism, congestive heart failure and renal failure, cardiac troponin elevation is indicative of myocardial infarction due to acute myocardial ischemia.1-3) Cardiac troponin (I or T) is nearly absolutely myocardial specific and has high clinical sensitivity, reflecting microscopic zones of myocardial necrosis.2) Ischemic electrocardiographic (ECG) changes following seizure have been documented in refractory epileptic patients.4) However, clinically defined myocardial infarction is a rare complication of epilepsy.5) We herein report a patient referred to us for elevated cardiac biomarker levels following an episode of generalized tonic-clonic seizure.
A 50 year-old man with history of recurrent epileptic seizure was admitted to the emergency room after an episode of seizure in July 2010. He had collapsed suddenly due to generalized tonic-clonic seizure lasting 5 minutes. On admission, he denied symptoms such as chest pain, shortness of breath, recent history of fever, or flu-like illness. He was known to experience recurrent epileptic seizures of traumatic origin after a fall, for which he was treated for intracranial and subdural hemorrhage in 2007. Since then, he had been on antiepileptic medication. Other past history was unremarkable and he had no cardiovascular risk factors.
On admission, neurologic examinations were normal and the patient was alert. Emergent brain magnetic resonance imaging (MRI) showed stabilized chronic damage secondary to the previous fall, in the absence of any findings suggestive of recent cerebral damage (Fig. 1). His vital signs were stable: blood pressure 110/70 mm Hg; heart rate 72 beats per minutes and breathing rate 18 per minutes. His chest was clear on auscultation. Cardiovascular examination was normal. His heart rhythm was regular without associated gallops or murmurs. His ECG showed normal sinus rhythm. Blood tests were within the normal limits, with the exception of creatine phosphokinase (231 U/L, normal <180 U/L), myoglobin (157 ng/mL, normal <92.5 ng/mL) and cardiac troponin I (0.91 ng/mL, normal <0.07 ng/mL). After 3 hours, cardiac troponin I and MB fraction of creatinine phosphokinase were 7.29 ng/mL (normal <0.07 ng/mL) and 8.1 ng/mL (normal <3.6 ng/mL), respectively. Echocardiography revealed normal global and regional wall motion with an ejection fraction of 68%. Computed tomography (CT) for coronary artery showed more than 50% stenosis in the middle left anterior descending coronary artery (Fig. 2). So, coronary angiography was performed, showing about 30% stenosis of the middle left anterior descending coronary artery (Fig. 3) and ergonovine provocation test was negative. Finally, the patient was diagnosed clinically with type 2 myocardial infarction. The lesion was treated with diltiazem and nitrate until ergonovine test was performed. Antiepileptic medication and diltiazem was continued for secondary prevention. Cardiac troponin I was normalized after 5 days of diagnosis.
Various types of myocardial infarction can be clinically classified. Among them, type 2 myocardial infarction is caused by ischemia due to either increased oxygen demand or decreased oxygen supply.3) The possible causes of type 2 myocardial infarction after a seizure are numerous, but mainly related to an imbalance between oxygen supply and myocardial metabolic demand.6) This can be caused by increased muscular activity associated with seizures or by massive catecholamine release from sympathetic nerve endings, causing increase in heart rate, arterial blood pressure and myocardial contractility. Elevation of troponin I may occur frequently in patients with supraventricular tachycardia, even in the absence of coronary artery disease.7) Generalized tonic-clonic seizure can be considered a physiological cardiac stress test. It is well known that acute cerebrovascular events can induce cardiac disorders.8) However, in our patient, we excluded acute cerebrovascular causes on radiological and clinical grounds.
There are several non-cardiac and cardiac conditions other than acute coronary syndrome that lead to increase in cardiac troponin I, such as myocarditis, aortic dissection, pulmonary embolism, congestive heart failure and renal failure.9) In our patient, we could not identify evidence of other etiologies causing elevation in cardiac troponin I.
For diagnosis of acute myocardial infarction, there should be at least one symptom of ischemia, ECG changes indicative of new ischemia and imaging evidence of new loss of viable myocardium or new regional wall motion abnormality, in addition to elevation in cardiac biomarkers (preferably troponins).3) However, in cases concordant with a seizure episode, it will be difficult to apply these diagnostic criteria of myocardial infarction due to the following reasons. Chest pain may be absent in as many as 75% of documented episodes of myocardial ischemia, with 30% of myocardial infarction being either silent or associated with atypical chest pain.10) In addition, an epileptic cannot complain of symptoms, such as chest pain or discomfort during a seizure. The ECG is not sufficiently diagnostic in 20% of patients with myocardial infarction.11) In one multi-hospital observational study, only 57% of patients with acute myocardial infarction had diagnostic ECG and 7.9% had normal ECG, who tended to be younger and being male12) and it is difficult to obtain an ECG during a seizure. The troponin levels are valuable for early diagnosis, and the prediction of the long term prognosis in ACS patients with a normal ECG.13) Imaging techniques, such as echocardiography, radionuclide ventriculography, myocardial perfusion scintigraphy and MRI may play roles in patients with suspected myocardial infarction. However, it has been known that when an infarction thickness of myocardium is 20% or more, wall motion abnormality can be detected in echocardiography. Therefore, in cases with microscopic (focal) or small infarction, wall motion abnormality may not be detected by conventional echocardiography. In addition, although radionuclide imaging is the only commonly available direct method of assessing viability, it has relatively low image resolution for detecting small areas of infarction. However, contrast enhanced cardiovascular MRI (CMR) systematically detects subendocardial infarcts missed by single photon emission computed tomography.14) Therefore, CMR would play an important role in the detection of suspected myocardial infarction.
In one analytic cross-sectional study, cardiac troponin I following seizure was within the normal limits in 49 patients with uncomplicated epileptic seizures and healthy cardiovascular systems.15) No elevation in cardiac troponins levels was seen in 11 patients after monitored seizure, indicating that myocardial injury does not occur during uncomplicated seizure.16) In two studies, however, the duration of seizure was short and this induced only moderate tachycardia. The mean age of monitored patients in these studies was 21 and 34 years, respectively. This means that seizures as physiologic cardiac stress did not exceed myocardial functional reserve of epileptics. If there were elderly epileptics with lower myocardial functional reserve, or when duration of a seizure was long enough, elevation of troponin I may be seen.
Sudden unexplained death in epilepsy exceeds the expected rate of sudden death in the general population by nearly 24 times.17) Cardiac pathologic conditions indicative of myocardial injury have been reported in association with sudden unexplained death in epileptic patients.18) These findings lead to the consideration of suspected coronary artery disease in patients showing elevated cardiac troponins following a seizure. In previously reported cases, two patients had significant stenosis of the coronary arteries and five patients had no or mild stenosis of coronary artery despite elevated cardiac troponins.7)19)20) In the first two cases, only a minor increase in metabolic demand due to short seizure might have caused myocardial infarction due to lower myocardial functional reserve.
In the management of type 2 myocardial infarction follow-ing seizure, antiepileptic medication is important treatment that reduces episodes of increased oxygen demand. Assuming that type 2 myocardial infarction after a seizure is related to excess catecholamine release, beta blocker and non-dihydropyridine calcium channel blocker may have preventive effects on secondary changes, such as increased heart rate and arterial blood pressure. The correction of risk factors for coronary artery disease may be helpful to improve myocardial functional reserve.
In conclusion, in patients with no significant coronary artery disease, myocardial infarction can occur following seizure activity, especially in patients with lower myocardial functional reserve. This is type 2 myocardial infarction. Although elevation of cardiac troponins is among the three established criteria for the diagnosis of acute myocardial infarction after seizure, type 2 myocardial infarction should be considered and be excluded first, before calling it a false positive assay for cardiac troponins.
Figures and Tables
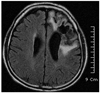 | Fig. 1Fluid attenuated inversion recovery brain magnetic resonance image. This showed high signal intensity around a previous hemorrhage site in the left frontal lobe, indicating malatic change after hemorrhage without evidence of newly developed lesions. |
References
1. Jaffe AS, Babuin L, Apple FS. Biomarkers in acute cardiac disease: the present and the future. J Am Coll Cardiol. 2006. 48:1–11.
2. Jaffe AS, Ravkilde J, Roberts R, et al. It's time for a change to a troponin standard. Circulation. 2000. 102:1216–1220.
3. Thygesen K, Alpert JS, White HD, et al. Universal definition of myocardial infarction. Circulation. 2007. 116:2634–2653.
4. Tomson T, Walczak T, Sillanpaa M, Sander JW. Sudden unexpected death in epilepsy: a review of incidence and risk factors. Epilepsia. 2005. 46:Suppl 11. 54–61.
5. Chin PS, Branch KR, Becker KJ. Myocardial infarction following brief convulsive seizures. Neurology. 2004. 63:2453–2454.
6. Montepietra S, Cattaneo L, Granella F, et al. Myocardial infarction following convulsive and nonconvulsive seizures. Seizure. 2009. 18:379–381.
7. Kim SK, Kim YD, Kim MJ, et al. The elevation of serum cardiac troponin I in patients with supraventricular tachycardia without evidence of coronary artery disease. Korean Circ J. 2006. 36:381–386.
8. Samuels MA. The brain-heart connection. Circulation. 2007. 116:77–84.
9. Khan IA, Tun A, Wattanasauwan N, et al. Elevation of serum cardiac troponin I in noncardiac and cardiac diseases other than acute coronary syndromes. Am J Emerg Med. 1999. 17:225–229.
10. Kannel WB. Prevalence and clinical aspects of unrecognized myocardial infarction and sudden unexpected death. Circulation. 1987. 75:II4–II5.
11. Turi ZG, Rutherford JD, Roberts R, et al. Electrocardiographic, enzymatic and scintigraphic criteria of acute myocardial infarction as determined from study of 726 patients (A MILIS Study). Am J Cardiol. 1985. 55:1463–1468.
12. Welch RD, Zalenski RJ, Frederick PD, et al. Prognostic value of a normal or nonspecific initial electrocardiogram in acute myocardial infarction. JAMA. 2001. 286:1977–1984.
13. Lim SY, Jeong MH, Bae EH, et al. The clinical significance of elevated troponin in patients with acute coronary syndrome with normal electrocardiogram. Korean Circ J. 2003. 33:385–392.
14. Wagner A, Mahrholdt H, Holly TA, et al. Contrast-enhanced MRI and routine single photon emission computed tomography (SPECT) perfusion imaging for detection of subendocardial myocardial infarcts: an imaging study. Lancet. 2003. 361:374–379.
15. Hajsadeghi S, Afsharian S, Fereshtehnejad SM, Keramati MR, Mollahoseini R. Serum levels of cardiac troponin I in patients with uncomplicated epileptic seizure. Arch Med Res. 2009. 40:24–28.
16. Woodruff BK, Britton JW, Tigaran S, et al. Cardiac troponin levels following monitored epileptic seizures. Neurology. 2003. 60:1690–1692.
17. Ficker DM, So EL, Shen WK, et al. Population-based study of the incidence of sudden unexplained death in epilepsy. Neurology. 1998. 51:1270–1274.
18. Natelson BH, Suarez RV, Terrence CF, Turizo R. Patients with epilepsy who die suddenly have cardiac disease. Arch Neurol. 1998. 55:857–860.
19. Brobbey A, Ravakhah K. Elevated serum cardiac troponin I level in a patient after a grand mal seizure and with no evidence of cardiac disease. Am J Med Sci. 2004. 328:189–191.
20. Parvulescu-Codrea S, Britton JW, Bruce CJ, Cascino GD, Jaffe AS. Elevations of troponin in patients with epileptic seizures? What do they mean? Clin Cardiol. 2006. 29:325–326.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download