Abstract
Background and Objectives
In patients with fibromyalgia (FM) syndrome, stress and pain may chronically enhance sympathetic activity, altering cardiovascular responses and inducing the arterial wall-stiffening process. We investigated arterial stiffness in FM patients using pulse wave velocity (PWV) and analyzed whether arterial stiffness was affected by the clinical parameters of FM.
Subjects and Methods
This study included 108 female FM patients (51.5±8.9 years) without any known cardiovascular diseases and 76 healthy female controls (50.1±8.9 years). FM patients underwent a manual tender point survey for tender point counts, and completed the visual analogue scale (VAS) of pain and fibromyalgia impact questionnaire (FIQ), which were composed of a physical and feel score. Brachial-ankle pulse-wave velocity (baPWV) was measured with an automated device. The study participants were subdivided into 2 groups based on the sum of the FIQ score (group A: FIQ ≥50, group B: <50).
Results
Patients with FM had significantly higher baPWV than the controls, and significant increase were noted in baPWV values of group A compared with those of group B. BaPWV showed a significant positive correlation (correlation coefficient=6.83, p=0.022) with severity of disease assessed by FIQ.
Conclusion
The patients with FM showed significantly increased arterial stiffness, suggesting a pathophysiologic link between FM and endothelial dysfunction. This study provides a basis for clarifying the mechanism by which chronic pain syndrome is associated with an increased risk of vascular stiffness.
Fibromyalgia (FM) syndrome, characterized by chronic widespread pain and discomfort, has diverse characteristics including widespread musculoskeletal pain with discrete points of tenderness along with fatigue, sleep disturbance, cognitive dysfunction, and depressed mood. FM is considered to result from deregulation of pain modulator systems involving altered interactions between central and peripheral nervous systems and immune systems.1) In patients with FM, stress and pain may chronically enhance sympathetic activity. Several lines of evidence indicate that sympathetic nervous system (SNS) function is altered in patients with FM.2)3) SNS activity is an important determinant of the arterial wall-stiffening pro-cess. Chronically enhanced sympathetic activity may alter cardiovascular responses and induce endothelial dysfunction. Using a nonhuman primate model of atherogenesis, it has been observed that psychosocial stress can alter the autonomic balance towards a state of sympathetic arousal leading to the development of coronary artery disease (CAD), perhaps through impairing endothelial function4) and intensification of endothelium-mediated atherogenic processes.5) In recent years, several studies have shown a decrease in endothelial function in association with clinical depression or sub-clinical mood states or personality traits such as depression, anxiety, type A personality (hostility) or anger.6)7)
Since stiffened arteries transmit pulse waves faster than the more elastic blood vessels, pulse wave velocity (PWV) is an ideal indicator of arterial stiffness, and brachial artery pulse wave velocity (baPWV) is used to assess endothelial function by measuring the status of large and small arteries in the lower extremity.8) We proposed that even in FM patients, we can observe a decrease in endothelial function, considering that psychological symptoms including anxiety, stress, and depression are often observed in FM.9) This study investigated arterial stiffness in FM patients using baPWV, and analyzed whether arterial stiffness was affected by the clinical parameters of FM, which were assessed by the fibromyalgia impact questionnaire (FIQ).
This study was conducted from January 2010 to December 2010, and enrolled 108 consecutive female FM patients and 76 healthy female controls that were matched to the FM patients by their age, blood pressure (BP), heart rate, height, cholesterol and glucose levels. Diagnosis of FM was confirmed by a board-certified rheumatologist according to the guidelines outlined by the American College of Rheumatology.10) Patients with history of major atherosclerotic risk factors including hypertension and diabetes, history of CAD, congestive heart failure, history of neurological illness, smoking, obesity with body mass index above 26 and abnormal C-reactive protein (CRP) were excluded from the study. Controls were recruited from the cardiology clinic and health screening center and included subjects without chronic widespread pain. The study was approved by the Maryknoll medical center institutional review board and all subjects gave their written informed consent.
At each visit, patients with FM were asked to rate their current level of pain on the 10 cm Visual Analog Scales (VASs, 0=no pain, 10=worst pain imaginable), a scale for rating pain intensity. Subjects then filled out the Korean Fibromyalgia Impact Questionnaire (kFIQ),11) which is a validated, self-administered test, scored out of 100, that evaluates physical function, work status, depression, anxiety, sleep, pain, stiffness, fatigue, and well being. The study participants were also subdivided into 2 groups based on the sum of the FIQ score (group A: FIQ ≥50, group B: <50). Subjects were then assessed for the number of positive tender points by digital palpation over the 18 characteristic tender point sites in the ACR criteria for the diagnosis of FM. The subjects were requested to identify if a given point was painful as slow steady digital pressure was applied. The self-administered questionnaire, the Beck Depression Inventory (BDI) scale, and Brief Fatigue Inventory (BFI) scale, assessed symptoms of depression and fatigue, respectively.
Arterial stiffness was assessed by measuring brachial-ankle (ba) PWVs using an automatic waveform analyzer (VP-1000; Colin Co., Komaki, Japan).12) The VP-1000 simultaneously records pulse waves, BP (both arms and ankles), ankle-brachial pressure index (ABI), electrocardiography, and heart sounds, as described elsewhere.12)13) ABI was calculated by the ratio of the ankle systolic BP divided by the arm systolic BP, and the lower value of the ankle systolic BP was used for the calculation. For measuring baPWV, pulse waves obtained from the brachial and tibial arteries were recorded simultaneously, and the transmission time, which was defined as the time interval between the initial increase in brachial and tibial waveforms, was determined. The transmission distance from the arm to each ankle was calculated according to body height. The baPWV was automatically computed as the transmission distance divided by the transmission time. All participants included in the present study had a normal ABI (>0.9). A high baPWV was defined as the gender-specific highest quartile of the values among the study subjects {baPWV (the mean of the right and left values) ≥1,490 cm/s in females}.
All data were expressed as mean±standard deviation. Data were analyzed using standard statistical software (Statistical Package for the Social Sciences package version 11.0, Chicago, IL, USA) and comparisons of all measurements were made with paired Student's t-test for continuous variables and Pearson correlation test for correlation. Multivariate analysis was performed with logistic regression for the associations between demographic, atherosclerotic risk factors and baPWV. P<0.05 was considered statistically significant.
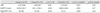
There were no significant differences between the FM and control groups in terms of age and the other parameters that are known to affect the PWV, including height, BP, heart rate and the total cholesterol levels (Table 1). There were also no significant differences in these variables except disease duration of the FM syndrome (p=0.007) (Table 2) between the groups A and B (Table 2). The value of tender point counts, pain VAS, FIQ scores, scales of anxiety, fatigue and depression were significantly higher in group A, as compared to group B (Table 2).
The parameters of arterial stiffness, represented baPWV, of the FM patients and controls are shown in Table 1. The baPWV values of the FM and control groups (1,378.9±242.2 cm/s vs. 1,284.0±186.27 cm/s, p=0.005) were significantly different (Table 1). Significant increases were also noted in baPWV values of group A compared with those of group B (1,438.9±281.7 vs. 1,330.4±184.3, p=0.013) (Table 3), and the same result was observed with the control group included (Table 3). The baPWV value of the subgroup (less than 130 mm Hg of systolic BP, and less than 200 mg/dL of total cholesterol, and less than 60 years of age) were also significantly different in patients with FM, as compared to controls (n=55, 1,338.4±228.6 vs. 1,241.9±181.9, p=0.005).
BaPWV showed a significant positive correlation with FIQ (r=0.29, p=0.003) (Fig. 1A) using Pearson's correlation coefficient. Significant positive correlations were also founded between baPWV and parameters of physical and emotional stress such as pain VAS, depression, anxiety, and fatigue subscales (Fig. 1). Multiple regression analysis was used to adjust for any potential confounding influences of age, cholesterol, the duration of the disease and the clinical variables of FM. This relationship remained highly significant on multivariate regression analysis to determine the independent contribution FIQ score to baPWV (adjusted r=0.194, p=0.022). However, grade of depression, fatigue scale, pain VAS, and tender point counts exhibited no significant effect on baPWV (Table 4). The proportion of patients with high baPWV was significantly greater in the patients group compared to the control, and group A compared to group B (all p<0.01).
For over a century, it has been thought that abnormal activity of the SNS may be involved in the pathogenesis of chronic pain syndromes. This assumption was based on the observation that pain is spatially correlated with signs of autonomic dysfunction and that blocking the efferent sympathetic supply to the affected region relieves the pain.14) Several mechanisms of endothelial damage concomitant with, or downstream to, SNS activation have been proposed. Recent data suggest that elevated systemic levels of catecholamines are central to the pathophysiology of these kinds of disorders.15) The mechanisms of catecholamine-induced endothelial damage, however, are thought to be multifactorial, including persistent activation of calcium channels, membrane damage, and microvascular spasms.16) Microvascular endothelial dysfunction can sensitize the coronary circulation to the vasoconstrictor effects of catecholamines.17) Microvascular spasm and cardiac syndrome X are also associated with female predominance, particularly in the postmenopausal years, congruent to the gender differences seen in transient left ventricular (LV) dysfunction.18) Previously, we examined myocardial function in patients with FM with 2-dimensional strain echocardiography and assessed the relationship between clinical parameters of FM and myocardial function.19) In that study, we suggested that the severity of distress in patients with FM might be correlated with LV function and chronic distress might reduce myocardial longitudinal deformation by possible microcirculatory impairment or endothelial dysfunction due to excessive activation of the SNS. At that time, we expected that decrease in endothelial function could be observed in patients with FM, and in the recent study,20) we evaluated endothelial dysfunction reflected by an impaired brachial artery flow-mediated dilatation (FMD) response in patients with FM. We showed that FM patients exhibited decreased endothelial-dependent vasodilatation and endothelial-independent vasodilatation, and these parameters were in parallel with FIQ and pain parameters as well. Because FMD is endothelium-dependent and is largely controlled by the release of endothelial nitric oxide (NO),21) an impairment of endothelium-dependent FMD suggests that there is decreased endothelial NO activity, which has been found to directly regulate large artery stiffness in vivo.22)
In the present study, we compared ABI and baPWV in female FM patients and evaluated the factors affecting arterial stiffness in patients with FM. ABI was reported to be a good marker for atherosclerosis and useful in the diagnosis of peripheral artery occlusive disease.23)24) baPWV has been reported as a good marker for arterial stiffness.25) The results of smaller studies have shown that baPWV was an independent predictor of cardiovascular death and cardiac events in elderly persons in the community as well as in patients with CAD.26)27) Although data on the value of the baPWV for the prediction of cardiovascular events is limited, the baPWV is easy to measure and has the potential for screening applications.28) The ABI and baPWV measurement can be conducted at low cost using simple techniques and is non-invasive and not operator-dependent, like carotid ultrasound. In our study, FM patients showed decreased ABI values compared to the controls, but ABI showed no correlation with clinical parameters of FM, which suggests that the severity of disease is not associated with arterial stenosis. We found that the proportion of high baPWV was significantly higher in FM patients and baPWV was related to age and parameters of physical and emotional stress such as pain VAS, FIQ score, subscales of depression, anxiety, and fatigue. Increased arterial stiffness in FM patients suggested a pathophysiologic link between FM and endothelial dysfunction.
There were several limitations in our study. This study was performed in women, and the selected study population can be a limitation. However, male FM patients are more prone to smoking, old age, and dyslipidemia than female FM patients, which were well known confounding factors on arterial stiffness. Besides considering the gender effect itself on arterial stiffness, we wanted to evaluate the pure contribution of disease severity on arterial stiffness, so we excluded the male population. Second, we did not account for the menstrual cycle of patients during this study. Previous data has suggested that there are no effects of the different hormonal phases of the menstrual cycle on cardiovascular variables such as heart rate variability (HRV) and baroreflex sensitivity (BRS). Leicht et al.29) reported no alteration of HRV during different time points in a regular menstrual cycle. Similarly, Cooke et al.30) reported no alteration of BRS during different time points in a regular menstrual cycle. However, it is possible that this difference masked some additional discrepancies between the women with FM and the healthy controls. Finally, our participants were on a variety of medications. It is likely that antidepressants may have some effect on autonomic function, but we did not account for medication since the sample size was too small. Therefore, the findings of this study are only preliminary data, and large surveys with sampling of subjects by strict medical examination will be necessary in the future.
In conclusion, based on our findings, female FM patients had significantly increased arterial stiffness when compared with the healthy controls. This study provides a basis for clarifying the mechanism by which FM is associated with increased risk of vascular stiffness, but longitudinal studies employing a larger sample population are required to determine the pathophysiologic and prognostic implications of increased arterial stiffness in FM.
Figures and Tables
 | Fig. 1Regression analysis between parameters of fibromyalgia functional status and brachial-ankle pulse wave velocity (baPWV). FIQ (A), pain VAS (B) and subscales of depression (C), anxiety (D), and fatigue (E) showed significant effect on baPWV. FIQ: fibromyalgia impact questionnaire, VAS: visual analog scales. |
References
1. Wallace J, Clauw J. Wallace DJ, Clauw DJ, editors. Epidemiology of chronic widespread pain and fibromyalgia. Fibromyalgia and other Central Pain Syndromes. 2005. Philadelphia: Lippincott Williams & Wilkins;17–29.
2. Giske L, Vøllestad NK, Mengshoel AM, Jensen J, Knardahl S, Røe C. Attenuated adrenergic responses to exercise in women with fibromyalgia: a controlled study. Eur J Pain. 2008. 12:351–360.
3. Martinez-Lavin M. Biology and therapy of fibromyalgia: stress, the stress response system and fibromyalgia. Arthritis Res Ther. 2007. 9:216–222.
4. Strawn WB, Bondjers G, Kaplan JR, et al. Endothelial dysfunction in response to psychosocial stress in monkeys. Circ Res. 1991. 68:1270–1279.
5. Manuck SB, Kaplan JR, Adams MR, Clarkson TB. Effects of stress and the sympathetic nervous system on coronary artery atherosclerosis in the cynomolgus macaque. Am Heart J. 1988. 116:328–333.
6. Rajagopalan S, Brook R, Rubenfire M, Pitt E, Young E, Pitt B. Abnormal brachial artery flow-mediated vasodilation in young adults with major depression. Am J Cardiol. 2001. 88:196–198.
7. Harris KF, Matthews KA, Sutton-Tyrrell K, Kuller LH. Associations between psychological traits and endothelial function in postmenopausal women. Psychosom Med. 2003. 65:402–409.
8. Hirsch AT, Criqui MH, Treat-Jacobson D, et al. Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA. 2001. 286:1317–1324.
9. Wallace J, Clauw J. Wallace DJ, Clauw DJ, editors. Symptoms and signs of Fibromyalgia syndromes: an overview. Fibromyalgia and Other Central Pain Syndromes. 2005. Philadelphia: Lippincott Williams & Wilkins;127.
10. Wolfe F, Smythe HA, Yunus MB, et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia: report of the Multicenter Criteria Committee. Arthritis Rheum. 1990. 33:160–172.
11. Bae SC, Lee JH. Cross-cultural adaptation and validation of the Korean myalgia impact questionnaire in women patients with fibromyalgia for clinical research. Qual Life Res. 2004. 13:857–861.
12. Yamashina A, Tomiyama H, Takeda K, et al. Validity, reproducibility, and clinical significance of noninvasive brachial-ankle pulse wave velocity measurement. Hypertens Res. 2002. 25:359–364.
13. Tomiyama H, Yamashina A, Arai T, et al. Influences of age and gender on results of noninvasive brachial-ankle pulse wave velocity measurement: a survey of 12517 subjects. Atherosclerosis. 2003. 166:303–309.
14. Baron R, Levine JD, Fields HL. Causalgia and reflex sympathetic dystrophy: does the sympathetic nervous system contribute to the generation of pain? Muscle Nerve. 1999. 22:678–695.
15. Wittstein IS, Thiemann DR, Lima JA, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med. 2005. 352:539–548.
16. Zaroff JG, Rordorf GA, Titus JS, et al. Regional myocardial perfusion after experimental subarachnoid hemorrhage. Stroke. 2000. 31:1136–1143.
17. Vita JA, Treasure CB, Yeung AC, et al. Patients with evidence of coronary endothelial dysfunction as assessed by acetylcholine infusion demonstrate marked increase in sensitivity to constrictor effects of catecholamines. Circulation. 1992. 85:1390–1397.
18. Mohri M, Koyanagi M, Egashira K, et al. Angina pectoris caused by coronary microvascular spasm. Lancet. 1998. 351:1165–1169.
19. Cho KI, Lee JH, Kim SM, et al. Assessment of myocardial function in patients with fibromyalgia and the relationship to chronic emotional and physical stress. Korean Circ J. 2010. 40:74–80.
20. Cho KI, Lee JH, Kim SM, et al. Assessment of endothelial function in patients with fibromyalgia-cardiac ultrasound study. Clin Rheumatol. 2011. 30:647–654. doi: 10.1007/s10067-010-1599-8.
21. Joannides R, Haefeli WE, Linder L, et al. Nitric oxide is responsible for flow-dependent dilatation of human peripheral conduit arteries in vivo. Circulation. 1995. 91:1314–1319.
22. Wilkinson IB, Qasem A, McEniery CM, Webb DJ, Avolio AP, Cockcroft JR. Nitric oxide regulates local arterial distensibility in vivo. Circulation. 2002. 105:213–217.
23. Fishbane S, Youn S, Kowalski EJ, Frei GL. Ankle arm blood pressure index as a marker for atherosclerotic vascular diseases in hemodialysis patients. Am J Kidney Dis. 1995. 25:34–39.
24. Newman AB, Tyrrell KS, Kuller LH. Mortality over four years in SHEP participants with a low ankle arm index. J Am Geriatr Soc. 1997. 45:1472–1478.
25. Boutouyrie P, Tropeano AI, Asmar R, et al. Aortic stiffness is an independent predictor of primary coronary events in hypertensive patients: a longitudinal study. Hypertension. 2002. 39:10–15.
26. Lee YS, Kim KS, Nam CW, Kim YN. Increased arterial stiffness in patients with cardiac syndrome X-pulse wave velocity in cardiac syndrome X. Korean Circ J. 2005. 35:424–428.
27. Tomiyama H, Koji Y, Yambe M, et al. Brachial: ankle pulse wave velocity is a simple and independent predictor of prognosis in patients with acute coronary syndrome. Circ J. 2005. 69:815–822.
28. Rhee MY, Lee HY, Park JB. Measurements of arterial stiffness: methodological aspects. Korean Circ J. 2008. 38:343–350.
29. Leicht AS, Hirning DA, Allen GD. Heart rate variability and endogenous sex hormones during menstrual cycle in young women. Exp Physiol. 2003. 88:441–446.
30. Cooke WH, Ludwig DA, Hogg PS, Eckberg DL, Convertino VA. Does the menstrual cycle influence the sensitivity of vagally mediated baroreflexes? Clin Sci (Lond). 2002. 102:639–644.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download