Abstract
Hepatocellular carcinoma (HCC) with metastasis to the heart is uncommon. We report a rare case of left atrial metastasis of HCC which was resected palliatively as a live-saving procedure with the use of cardiopulmonary bypass. Despite chemoembolization, which was undertaken 11 times, cardiac metastasis occurred. Moreover, the right and left atria and left ventricle were involved simultaneously. The severe dyspnea improved dramatically after surgery. Following this, the patient underwent systemic chemotherapy and lived a life without recurrence of symptoms associated with mitral valve obstruction.
The majority of tumors of the heart are metastatic from extracardiac tumors. Primary tumors of the heart are rare, with a prevalence of 0.001-0.03% in an autopsy series.1) Approximately 75% of primary cardiac tumors are benign, with cardiac myxomas accounting for >50% of benign cardiac tumors. Hepatocellular carcinoma (HCC) is the most common primary malignant tumor of the liver. The most common sites of HCC metastasis are the lungs, followed by the regional lymph nodes and adrenal glands.2) The heart is an uncommon site for HCC metastasis with the right atrium (RA) the most common site.3-5) Surgical treatment of metastatic HCC is generally performed for symptomatic patients. We recently managed a patient with metastatic HCC in the RA, left atrium (LA), and left ventricle (LV) who underwent an emergent tumorectomy for symptomatic relief.
A 48-year-old male was admitted to our hospital for evaluation of a left pleural effusion demonstrated by CT scan 1 day earlier. He complained of NYHA II dyspnea. Twenty-nine months earlier, he had been diagnosed with HCC with lung metastasis, for which he had received chemoembolization 11 times. Nevertheless, a CT scan performed 3 months ago showed tumor thrombi within the right hepatic vein (RHV), inferior vena cava (IVC), and RA (Fig. 1).
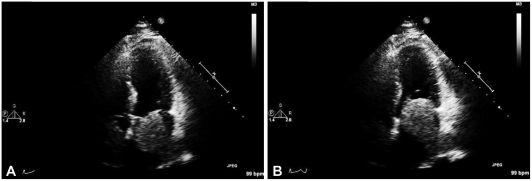
On hospital day 2, a sonography-guided left thoracentesis was performed. The laboratory data for the pleural fluid was as follows: lactate dehydrogenase, 312 U/L; white blood cell, >1,000/uL; and polymorphonuclear leukocytes, 40%. These results were consistent with an exudate. In addition, cytologic and microbiological studies showed negative results. Thus, the pleural fluid was thought to be a malignant or parapneumonic effusion. A chest X-ray revealed bilateral lower lung haziness, consistent with a pneumonia, thus antibiotics were started. A CT scan was obtained 1 day prior to admission and demonstrated intracardiac tumor thrombi of the IVC, RA, and LA (Fig. 2). Moreover, LV invasion was also suspected. Transthoracic echocardiography (TTE) revealed a LA thrombus obstructing the mitral valve (Fig. 3). The dyspnea worsened, and became intolerable on hospital day 8. We thus performed an emergent left atrial tumorectomy with the use of cardiopulmonary bypass (CPB) and a large tumor thrombus was extracted (Fig. 4). In the operating room, we applied CPB quickly because of unstable vital signs. After the left atriotomy was performed, we easily identified a large (5×4×4 cm), multi-lobulated, firm mass. The mass originated from the left pulmonary veins and protruded to the entire mitral valve orifice, but definite invasion into the mitral valve was not present. After confirmation, we extracted the mass at the origin of the pulmonary vein as much as possible. Then, we confirmed pulmonary venous return flow. During surgery, we had to reduce the CPB time (145 minutes) and aortic cross-clamp time (53 minutes) because of related co-morbidities. Therefore, we left the RA mass in situ, which did not cause symptoms of IVC obstruction. On pathologic examination of the specimen, we demonstrated metastatic HCC with necrosis and an organizing hematoma.
After surgery, the dyspnea resolved. In addition, follow-up echocardiography also demonstrated absence of the left atrial mass (Fig. 5). However, during the immediate post-operative period, acute renal failure developed and he received continuous renal replacement therapy in the intensive care unit. After he recovered from the renal failure, he received chemotherapy (5-fluorouracil and mitomycin-C). He was discharged with no dyspnea on hospital day 54 and lived a life without recurrence of the symptoms associated with mitral valve obstruction until the last outpatient follow-up, which was done 5 months post-operatively. However, 1 week after the last follow-up, he was admitted to our hospital complaining of hematemesis and melana. The hematemesis was recurrent during the admission and led to his death.
Roughly one-fourth of cardiac tumors are malignant. Metastatic cardiac tumors are 20-40 times more common than primary cardiac tumors.1) The most common malignancy that involves the heart is lung, followed by lymphoma, breast, leukemia, stomach, melanoma, liver, and colon.6)
Extrahepatic metastasis is frequent in advanced HCC, and the prognosis is poor. The common metastatic sites for HCC are the lung, regional lymph nodes, adrenal glands, peritoneum, and bones.2)7) Although HCC is prone to vascular invasion and extension, metastasis to the cardiac cavity is very rare.8)9) Kojiro et al. reported 18 cases of intracavitary metastasis in 439 HCC autopsy cases (4.1%). In addition, intracavitary metastasis occurs mostly in the RA,3-5) with few reports of other cardiac chamber involvement.10-12)
Two-dimensional echocardiography is considered to be the most important primary screening imaging modality for cardiac tumors.13) TTE reveals tumor size, location, mobility, and associated findings. Although TTE remains the initial diagnostic tool, transesophageal echocardiography (TEE) affords more detailed and accurate information. Matsumura et al.14) showed that TEE is superior to TTE in detecting cardiac masses, recognizing abnormal flow, and estimating the anatomic relationship between tumors or thrombi and cardiac structures. Moreover, TEE provides better resolution because it is closer to the heart and uses a higher frequency transducer. Regardless of the advantages, there are limitations. TEE has relatively low spatial resolution and is unable to penetrate bone or lung. We did not perform TEE because there was sufficient information regarding the HCC by TTE and CT.
CT is a superior modality for demonstrating the morphology, location, and extent of cardiac tumors. The advantage of CT over echocardiography is the ability to characterize the lesions and evaluate the pericardium, great vessels, and extracardiac structures, which makes it possible to delineate the extent of tumor involvement.1)15) In addition, CT provides the opportunity to investigate mediastinal structures, including lymph nodes, which could be involved in cases with cardiac tumors.16) CT images are also present in several formats, including traditional transverse, coronal images and sagittal images. Magnetic resonance is also useful in evaluating cardiac tumors. In our case, thoracic CT and echocardiography provided the diagnosis of cardiac metastasis, including the RA, LA, and LV.
Generally, surgical treatment is not an option for metastatic tumors, and is rarely performed.17) This is true for HCC. Surgical resection is reserved for symptomatic patients due to poor prognosis, i.e., short life expectancy and the inability to perform a radical excision. In addition, there is concern about systemic spread of cancer during CPB surgery.18) In spite of these concerns, surgical resection should be considered when palliative symptom relief is needed. In our case, this aim was accomplished uneventfully. Chemoembolization is an alternative strategy for cardiac metastasis.19)20) However, systemic chemotherapy is a disappointing treatment strategy, which has yielded lower response rates for HCC (<20%).2)
In conclusion, we report a patient with cardiac metastasis from HCC, who was treated by palliative surgical resection because of life-threatening dyspnea, followed by chemotherapy.
Based on our case, it would be worthwhile to mention two points which would be helpful in treating similar patients: 1) echocardiography and CT are useful tools to find cardiac metastasis in case of HCC; 2) although surgical resection is generally not indicated due to poor prognosis for HCC, it could be a better alternative to conservative management or chemoembolization for relieving life-threatening symptoms.
References
1. McManus B, Lee CH. Libby P, Bonow RO, Mann DL, Zipes DP, editors. Primary tumors of the heart. Braundwald's Heart Disease: a Textbook of Cardiovascular Medicine. 2007. 8th ed. Philadelphia: W.B. Saunders;p. 1815–1828.
2. Kew MC. Feldman M, Friedman LS, Brandt LJ, editors. Hepatic tumors and cysts. Sleisenger & Fordtran's Gastrointestinal and Liver Disease. 2006. 8th ed. Philadelphia: W.B. Saunders;p. 2007–2033.
3. Martínez Baca-López F, Ramírez-Arias E, Rayas-Gómez AL, Bernal-Ruiz EA, Saturno-Chiu G. Hepatocellular carcinoma with invasion into right cardiac cavities: report of a case and literature review. J Am Soc Echocardiogr. 2004; 17:192–194. PMID: 14752497.
4. Uemura M, Sasaki Y, Yamada T, et al. Surgery hepatocellular carcinoma with tumor thrombus extending into the right atrium: report of a successful resection without the use of cardiopulmonary bypass. Hepatogastroenterology. 2004; 51:1259–1262. PMID: 15362727.
5. Mansour Z, Gerelli S, Kindo MJ, Billaud PJ, Eisenmann B, Mazzucotelli JP. Right atrial metastasis from hepatocellular carcinoma. J Card Surg. 2007; 22:231–233. PMID: 17488426.
6. Abraham KP, Reddy V, Gattuso P. Neoplasms metastatic to the heart: review of 3314 consecutive autopsies. Am J Cardiovasc Pathol. 1990; 3:195–198. PMID: 2095826.
7. Masci G, Magagnoli M, Grimaldi A, et al. Metastasis of hepatocellular carcinoma to the heart: a case report and review of the literature. Tumori. 2004; 90:345–347. PMID: 15315319.
8. Ayoola EA, Olubuyide IO, Thomas J. Cardiovascular systemic invasion by hepatocellular carcinoma: incidence and pattern in a west African population. Afr J Med Med Sci. 1994; 23:61–66. PMID: 7839948.
9. Kojiro M, Nakahara H, Sugihara S, Murakami T, Nakashima T, Kawasaki H. Hepatocellular carcinoma with intra-atrial tumor growth: a clinicopathologic study of 18 autopsy cases. Arch Pathol Lab Med. 1984; 108:989–992. PMID: 6095786.
10. Lei MH, Ko YL, Kuan P, Lien WP, Chen DS. Metastasis of hepatocellular carcinoma to the heart: unusual patterns in three cases with antemortem diagnosis. J Formos Med Assoc. 1992; 91:457–461. PMID: 1358318.
11. Barasch E, Frazier OH, Silberman H, Shannon RL, Wilansky S. Left atrial metastasis from hepatocellular carcinoma: a case report. J Am Soc Echocardiogr. 1994; 7:547–549. PMID: 7986554.
12. Ryu KH, Zang DY, Park SS, et al. Intracavitary cardiac metastasis in primary hepatoma. Korean Circ J. 1993; 23:123–128.
13. Salcedo EE, Cohen GI, White RD, Davison MB. Cardiac tumors: diagnosis and management. Curr Probl Cardiol. 1992; 17:73–137. PMID: 1735241.
14. Matsumura M, Takamoto S, Kyo S, Yokote Y, Omoto R. Advantages of transesophageal color Doppler echocardiography in the diagnosis and surgical treatment of cardiac masses. J Cardiol. 1990; 20:701–714. PMID: 2131359.
15. Ekmektzoglou KA, Samelis GF, Xanthos T. Heart and tumors: location, metastasis, clinical manifestations, diagnostic approaches and therapeutic considerations. J Cardiovasc Med (Hagerstown). 2008; 9:769–777. PMID: 18607239.
16. Godwin JD, Axel L, Adams JR, Schiller NB, Simpson PC Jr, Gertz EW. Computed tomography: a new method for diagnosing tumor of the heart. Circulation. 1981; 63:448–451. PMID: 7449067.
17. Lee KS, Lee HH, Youn TJ, Nam GB, Kim DW, Cho MC. Resection of cardiac metastasis of malignant melanoma. Korean Circ J. 2000; 30:1170–1174.
18. Lin YS, Jung SM, Tsai FC, et al. Hepatoma with cardiac metastasis: an advanced cancer requiring advanced treatment. World J Gastroenterol. 2007; 13:3513–3516. PMID: 17659700.
19. Kotani E, Kiuchi K, Takayama M, et al. Effectiveness of transcoronary chemoembolization for metastatic right ventricular tumor derived from hepatocellular carcinoma. Chest. 2000; 117:287–289. PMID: 10631235.
20. Dazai Y, Katoh T, Katoh I, Sueda S, Yoshida R. Effectiveness of chemoembolization therapy for metastatic right atrial tumor thrombus associated with hepatocellular carcinoma. Chest. 1989; 96:434–436. PMID: 2546719.
Fig. 1
Tumor thrombi within right hepatic vein, inferior vena cava (A) and right atrium (B) demonstated by CT scan 3 months before surgical resection.
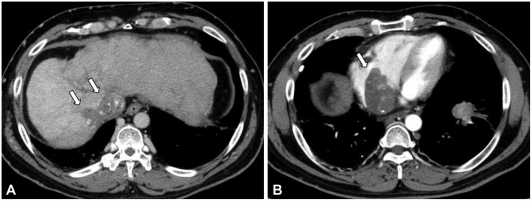
Fig. 2
Persistent tumor thrombi within right hepatic vein, inferior vena cava (A) and right atrium (B) demonstated by CT scan just days before surgical resection.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download