Abstract
Aseptic endocarditis is an uncommon complication of Behçet's disease (BD). We describe a rare case of a 39-year-old female who had BD with aseptic endocarditis of the tricuspid valve (TV) presenting as tricuspid stenosis. She was diagnosed with BD four years ago. The mucocutaneous lesions were well-controlled with colchicine and short courses of corticosteroids. She remained free of signs and symptoms of BD for one year without any medication. Three months before admission, she gradually developed dyspnea on exertion and peripheral edema. Echocardiography revealed dilated right atrium and markedly thickened TV with severe stenosis. TV replacement was performed. Pathologic examination of the valve showed fibrinoid necrotic material and inflammatory cell infiltration. Blood cultures and cultures of the excised valve were negative for microorganisms.
Behçet's disease (BD) is characterized by recurrent aphthous stomatitis, genital ulcers, and various skin lesions. BD can also involve other systems such as ocular, gastrointestinal, articular, neurological and cardiovascular systems. The frequency of cardiovascular involvement is estimated to be 4-46%.1)2) Common vascular manifestations are thrombophlebitis and arteritis, which occur in as many as one-third of the patients.3) Aseptic endocarditis is a rare manifestation of BD and is mostly found in the form of intracardiac thrombus or endomyocardial fibrosis.3)4)
Nonrheumatic tricuspid valve stenosis (TS) is extremely rare, and to our knowledge, it has never been reported in the English literature in patients with BD. We describe a case of a female BD patient with aseptic tricuspid valve (TV) endocarditis presenting as TS.
A 39-year-old female was admitted to Kyungpook National University Hospital with a 3-month history of dyspnea on exertion and abdominal distension. Vital signs were normal and evidence for infectious disease was absent. Signs of right heart failure such as pitting edema, palpable liver and neck vein distension were noted on physical examination. She had been diagnosed with BD four years ago. Although her previous clinical courses fluctuated, she did not show any signs or symptoms of BD since one year before admission. At the time of admission, evidence of BD disease exacerbation was absent; ESR 20 mm/hr (reference 0-20 mm/hr), Ferritin 71.50 ng/mL (reference 13-150 ng/mL).
Transthoracic echocardiography (TTE) showed normal left ventricular function, normal aortic and mitral valve function, morphology, and a moderate to large amount of pericardial effusion. Right atrium was dilated. Pericardiocentesis was performed. However, precise evaluation of right heart was difficult on TTE due to poor echo window. Transesophageal echocardiography showed severe TS with an ill-margined echogenic mass, and a mild to moderate amount of pericardial effusion (Figs. 1 and 2). Blood cultures for the detection of microorganisms were negative. Any other possible causes of TS, such as cardiac tumors, carcinoid syndrome, marantic endocarditis, and Wegener's granulomatosis were not detected.
Symptoms of right heart failure gradually progressed despite the appropriate steroid and immunosuppressive therapy.5) She was operated for TS. The thickened TV was removed and was replaced with an artificial valve (Edwards-MIRA 31 mm). Blood cultures and cultures of the excised valve were negative for microorganisms. Pathologic examination showed valvulitis consisting of fibrinoid necrotic material and inflammatory cells (Figs. 3 and 4). The special stains revealed no bacteria or fungi in the excised valve. These pathologic findings were consistent with those of previous reports presenting aseptic endocarditis in BD.6)7)
After the TV replacement, she remained free from symptoms of right heart failure with immunosuppressive therapy and anticoagulant therapy.
Endocarditis in BD may be limited to the valve leaflets or may spread to the ventricular or atrial wall and can result in serious complications, such as valvulopathy, organized thrombus or endomyocardial fibrosis.3)4)9) However, most cases of endocarditis in BD were detected in the form of organized thrombus or endomyocardial fibrosis.3)4) Not only an intracardiac thrombus but also a massive endomyocardial fibrosis could cause serious functional obstruction of the TV.3)4)9) However, overt TS due to valvulitis has not been reported, even though the affected valve leaflets could either be thickened or replaced by fibrous tissues. Also, we could not find any evidence of other combined sequelae of endocarditis, such as intracardiac thrombosis, endomyocardial fibrosis or valvulopathy of other valves.
McDonald et al.10) reported for the first time, a case of endocarditis involving the normal mitral and aortic valves in a patient with BD. These lesions were clinically silent, and were found during autopsy. Histologic examination of these valves showed mononuclear infiltration with a few polymorphonuclear leukocytes and no fibrin deposits. Madanat et al.6) reported a case of BD and endocarditis with left atrial thrombosis mimicking myxoma. Postoperative pathologic examination revealed yellowish valvulitis involving the mitral valve leaflet with deep ulcerations on the valve surface, covered by fibrinous and necrotic masses with a significant growth of granulation tissue. In other case reports of endocarditis in BD, several granulomas were found within the central portion of the vegetations and polymorphonuclear cells and lymphocytes infiltrated the small vessels near the vegetations.7) In our case, the pathologic examination showed vegetations, consisting of fibrinoid necrotic material, granulation tissue, and inflammatory cells, which were predominantly mononuclear cells. Small arteries and arterioles in the subintimal area showed irregular thickening of the wall. Evidence of active vasculitis was not seen in the excised tissues. These pathologic findings are consistent with those of previous reports. Therefore, TS was caused due to valvulitis as a possible sequelae of endocarditis in BD.
As in this case, the cardiac lesions in BD might progress insidiously in the absence of concurrent signs or symptoms of BD, or they were even diagnosed at autopsy.10)11) Therefore, it might be difficult to detect endocarditis in the early stage. These findings suggest that screening for cardiac involvement is required for early detection of endocarditis or other heart diseases in patients with BD.
Figures and Tables
Fig. 1
Transesophageal echocardiography showed a dilated right atrium and a thickened and doming tricuspid valve with an ill-margined echogenic mass (2.1×1.6 cm in size) between the septal and posterior leaflet, and a mild to moderate amount of pericardial effusion.

Fig. 2
Peak velocity of the tricuspid inflow was 1.9 m/sec and the mean pressure gradient between the right atrium and right ventricle was estimated to be approximately 12.6 mmHg.

Fig. 3
A light microscopy showed endocarditis manifesting as valvulitis, consisting of fibrinoid necrotic material and inflammatory cells (hematoxylin and eosin staining; ×100).
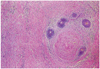
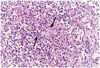
Fig. 4
Inflammatory cells were predominantly the mononuclear cells. In some areas, aggregation of neutrophils was also seen. Small arteries and arterioles in the subintimal area showed irregular thickening of the wall that might be due to previous vasculitis arrow (hematoxylin and eosin staining; ×400).
References
1. Atzeni F, Sarzi-Puttini P, Doria A, Boiardi L, Pipitone N, Salvarani C. Behçet's disease and cardiovascular involvement. Lupus. 2005. 14:723–726.
2. Park KM, Song JK, Kang DH, et al. Clinical characteristics of patients with cardiac involvement in Behçet's disease. Korean Circ J. 2005. 35:847–853.
3. Mogulkoc N, Burgess MI, Bishop PW. Intracardiac thrombus in Behçet's disease: a systematic review. Chest. 2000. 118:479–487.
4. Huong DL, Wechsler B, Papo T, et al. Endomyocardial fibrosis in Behçet's disease. Ann Rheum Dis. 1997. 56:205–208.
5. Dincer I, Dandachi R, Atmaca Y, Erol C, Caglar N, Oral D. A recurrent right heart thrombus in a patient with Behçet's disease. Echocardiography. 2001. 18:15–18.
6. Madanat WY, Prokaeva TB, Kotel'nikova GP, Alekberova ZS. Endocarditis with left atrial thrombus formation in Behçet's disease mimicking myxoma. J Rheumatol. 1993. 20:1982–1984.
7. Huycke EC, Robinowitz M, Cohen IS, et al. Granulomatous endocarditis with systemic embolism in Behçet's disease. Ann Intern Med. 1985. 102:791–793.
8. Silber H, Khan SS, Matloff JM, Chaux A, DeRobertis M, Gray R. The St. Jude valve: thrombolysis as the first line of therapy for cardiac valve thrombosis. Circulation. 1993. 87:30–37.
9. Candan I, Erol C, Sonel A, Akalin H. Behçet's disease: cardiac and pulmonary involvement. Eur Heart J. 1986. 7:999–1002.
10. McDonald BS, Gad-Al-Rab J. Behçet's disease with endocarditis and the Budd-Chiari syndrome. J Clin Pathol. 1980. 33:660–669.
11. Aouba A, Nebie L, Fabiani JN, Bruneval P, Patri B, De Bandt M. Tricuspid aseptic endocarditis revealing right endomyocardial fibrosis during an unrecognized Behçet's disease: a case report. Presse Med. 2004. 33:1367–1369.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download