Abstract
Malignant pericardial mesothelioma is a rare and progressive cardiac tumor. There is no established standard treatment and the prognosis is poor. Most patients were retrospectively diagnosed from surgery or autopsy due to absence of specific clinical manifestation. Most patients with pericardial mesothelioma have demonstrated constrictive physiology on echocardiography or cardiac catheterization. Therefore, pericardial mesothelioma was often misdiagnosed as other causes of constrictive pericarditis. We report a case of primary pericardial mesothelioma misdiagnosed as pericardial metastasis of unknown origin.
Malignant pericardial mesothelioma is an extremely rare and progressive cardiac tumor. Its clinical manifestations are nonspecific. Echocardiography, computed tomography (CT) and magnetic resonance imaging (MRI) may be used as summative diagnostic tools to support correct diagnosis. However, most malignant pericardial mesotheliomas have been diagnosed by histology, including immunohistochemical staining, after surgery or autopsy. To determine the exact etiology of constrictive pericarditic disease, clinical suspicion and confirmative evaluation are needed in patients who exhibit the physiology of constrictive pericarditis in transthoracic echocardiography (TTE) or catheterization. There is no established standard treatment and the prognosis remains poor.
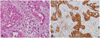
A 59 year-old woman presented to our hospital with a two-month history of intermittent shortness of breath and bilateral lower extremities edema. Otherwise her medical history was unremarkable. Arterial blood gas analysis showed no hypoxemia or hypercapnea, and serum liver function and kidney function test results were within the normal range. Chest radiograph revealed cardiomegaly. A 12-lead electrocardiography showed nonspecific findings. TTE demonstrated enlarged right atrium and ventricle associated with pericardial thickening around the posterior cardiac border (Fig. 1A) without pericardial effusion. TTE also showed dilated inferior vena cava (IVC) and IVC plethora. Echocardiographic Doppler examination demonstrated mitral flow early diastolic velocity decreased with inspiration and increased with expiration (Fig. 1B). The difference in peak early diastolic velocity between inspiration and expiration was approximately 30%. In addition, diastolic flow reversal of hepatic vein in expiratory phase was also demonstrated. Cardiac catheterization demonstrated rapid rising of early diastolic pressures and abrupt equalization in both ventricles, namely dip and plateau pattern (Fig. 2). Thoracic CT demonstrated pericardial thickening with multiple pericardial nodules, bilateral pleural effusion and lymphadenopathy in the cardiophrenic area (Fig. 3A). Abdomen CT demonstrated aortocaval lymphadenopathy with ascites (Fig. 3C), and coarse attenuation of liver parenchyma with periportal edema. We initially considered a diagnosis of malignancy of unknown origin with pericardial involvement. The first thoracoscopic pericardial biopsy revealed no malignant cells. Flexible gastroscopy, colonoscopy and breast ultrasonography showed no remarkable findings. F-18 fluorodeoxyglucose (FDG) positron emission tomography (PET) CT showed several hypermetabolic nodules in the pericardium, and the maximum standardized uptake value was 6.18 (Fig. 3B). However, no additional hypermetabolic lesions were noted (Fig. 3D). Primary pericardial malignancy was highly suspected from the imaging results. Thus, a second pericardial biopsy was planned. Pericardiectomy and exploration via sternotomy was performed to search malignancy tissue and to relieve symptoms. Microscopic examination revealed malignant mesothelioma of the epitheloid type. Immunohistochemical staining with calretinin and D2-40 (podoplanin) were positive, and with CEA and TTF-1 were negative (Fig. 4). Because the pericardium was the only lesion visible on PET-CT and there was no evidence of primary cancer origin in other organs, the patient was finally diagnosed with primary malignant pericardial mesothelioma.
The patient had taken sixth cycles of combination chemotherapy with pemetrexed and carboplatin. After chemotherapy, repeat thoracic CT showed similar cancer volume compared to that obtained on imaging prior to chemotherapy. She is still alive 8 months after diagnosis and is currently on conservative management.
Malignant pericardial tumors are rare causes of cardiac tumors. Secondary tumors are more common causes of cardiac tumors, which originate mostly from the lung, breast, melanomas, lymphoma, or leukemia. The incidence of malignant pericardial involvement with an underlying malignancy has been reported between 0.15 and 21% in the literature, of all patients with an underlying malignancy.1) Primary malignant pericardial mesothelioma is extremely rare, although it is the most common primary malignant pericardial tumor. Its incidence was 0.0022% among 500,000 cases in an autopsy study.2)
The clinical manifestation of malignant pericardial mesothelioma is nonspecific. Common clinical manifestations of pericardial tumors include constrictive pericarditis, pericardial effusion, cardiac tamponade, and heart failure caused by myocardial infiltration.3) Pericardial mesothelioma can often be misdiagnosed as other cause of constrictive pericarditis prior to undergoing pericardial tissue biopsy. Clinical suspicion is the most important factor for correct diagnosis. Echocardiographic evaluation is the most commonly used diagnostic tool. Cardiac catheterization examination can demonstrate constrictive physiology, which shows a dip and plateau pattern.4) MRI and CT used to aid making diagnosis. CT scan can demonstrate the extent of cardiac tumor, the extent of pericardial thickening, the mediastinal lymph node and the extracardiac lesions. These are helpful to distinguish primary pericardial tumors from the other cause of constrictive pericarditis, especially tuberculosis pericarditis. Mediastinal lymphadenopathy in patients with tuberculosis pericarditis has characteristically central low attenuation and coalescing of adjacent lymph nodes. In tuberculosis, pericarditis, aortopulmonary, paratracheal, and carinal lymph node invasion is common, but hilar lymphadenopathy is rare.5) The delayed phase image of CT scan or MRI is helpful to diagnose the pericardial tumor. In delayed phase image, pericardial soft tissue is distinguished from pericardial effusion. Furthermore, it is possible to observe hyperenhancement. These are useful to distinguish the primary pericardial tumors from tuberculous pericarditis.6) MRI is generally able to depict the tumor and its relation to surrounding cardiac structure.7) In a recent report, PET-CT was useful in the staging and preoperative evaluation of pleural8) or pericardial9) mesothelioma, detection of unsuspected nodal and occult distant metastases. However, most cases of malignant pericardial mesothelioma have been diagnosed by histology, including immunohistochemical staining after surgery or autopsy.10)
Malignant pericardial mesothelioma has poor prognosis and a progressive clinical course. Average survival was 10 months regardless of therapy.11) Moreover, standard treatment has not been established. Curative surgical resection can be performed only in patients with localized disease. Palliative surgery, includes pericardiectomy, may prevent cardiac tamponade and relieve pericardial constriction. In addition, pericardial mesothelioma responds poorly to radiation therapy. Recently, pemetrexed and carboplatin combination chemotherapy has demonstrated modest activity against malignant pleural mesothelioma as first line treatment.12) Irinotecan has also been reported to demonstrate clinical activity against pleural mesothelioma in a clinical trial.13)
In this case, because of ascites, pleural effusion and multiple lymphadenopathy, we initially suspected malignancy with multiple systemic metastases. However, significant FDG uptake in PET-CT was restricted in the pericardium. In retrospect, ascites and pleural effusion were only signs of pericardial constriction.
In conclusion, primary pericardial malignant mesothelioma is an extremely rare neoplasm. Advanced malignant pericardial mesothelioma has no established treatment modality and is often misdiagnosed as other cause of constrictive pericarditis. Clinical suspicion is the most important factor to correct diagnosis and early detection of this disease.
Figures and Tables
Fig. 1
A: transthoracic echocardiography demonstrated pericardial thickening (arrow) without pericardial effusion on the short axis view. B: Doppler echocardiography demonstrated difference in peak early diastolic velocity between inspiration (blue 1) and expiration (blue 2). LV: left ventricle, RV: right ventricle.

Fig. 2
Cardiac catheterization demonstrated rapid rising of early diastolic pressures and abrupt equalization in both ventricles (red arrow), namely the dip and plateau pattern. Diastolic pressures of the left and right ventricles are demonstrated.

Fig. 3
A: chest CT demonstrated thickened pericardium with multiple pericardial nodules (arrow) and bilateral pleural effusion. B: PET-CT demonstrated significant FDG uptake in the pericardium (arrow) with a maximal standardized uptake value of 6.18. C: abdominal CT demonstrated a 1.4 cm sized aortocarval lymphadenopathy (arrow). D: PET-CT demonstrated no significant FDG uptake in the aortocarval lymph node (arrow). PET: positron emission tomography, FDG: fluorodeoxyglucose.

References
1. Kralstein J, Frishman W. Malignant pericardial diseases: diagnosis and treatment. Am Heart J. 1987. 113:785–790.
2. Gossinger HD, Siostrznek P, Zangeneh M, et al. Magnetic resonance imaging findings in a patient with pericardial mesothelioma. Am Heart J. 1988. 115:1321–1322.
3. Suman S, Schofield P, Large S. Primary pericardial mesothelioma presenting as pericardial constriction: case report. Heart. 2004. 90:e4.
4. Ha CB, Huh JY, Shin YW, Shin YK. Doppler flow patterns of constrictive pericarditis. Korean Circ J. 1989. 19:47–54.
5. Cherian G, Habashy A, Uthaman B, Cherian J, Salama A, Anim J. Detection and follow-up of mediastinal lymph node enlargement in tuberculous pericardial effusions using computed tomography. Am J Med. 2003. 114:319–322.
6. Ha JW, Ko YG, Choi BW. Images in cardiology: delayed hyperenhancement of the pericardium by magnetic resonance imaging as a marker of pericardial inflammation in a patient with tuberculous effusive constrictive pericarditis. Heart. 2006. 92:494.
7. Kaminaga T, Takeshita T, Kimura I. Role of magnetic resonance imaging for evaluation of tumors in the cardiac region. Eur Radiol. 2003. 13:Suppl 6. L1–L10.
8. Flores RM, Akhurst T, Gonen M, et al. Positron emission tomography defines metastatic disease but not locoregional disease in patients with malignant pleural mesothelioma. J Thorac Cardiovasc Surg. 2003. 126:11–16.
9. Ost P, Rottey S, Smeets P, Boterberg T, Stragier B, Goethals I. F-18 fluorodeoxyglucose PET/CT scanning in the diagnostic work-up of a primary pericardial mesothelioma. J Thorac Imaging. 2008. 23:35–38.
10. Lagrotteria DD, Tsang B, Elavathil LJ, Tomlinson CW. A case of primary malignant pericardial mesothelioma. Can J Cardiol. 2005. 21:185–187.
11. Kaul TK, Fields BJ, Kahn DR. Primary malignant pericardial mesothelioma: a case report and review. J Cardiovasc Surg (Torino). 1994. 35:261–267.
12. Ceresoli GL, Zucali PA, Favaretto AG, et al. Phase II study of pemetrexed plus carboplatin in malignant pleural mesothelioma. J Clin Oncol. 2006. 24:1443–1448.
13. Kindler HL, Herndon JE, Zhang C, Green MR. Irinotecan for malignant mesothelioma A phase II trial by the Cancer and Leukemia Group B. Lung Cancer. 2005. 48:423–428.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download