Abstract
Myocardial involvement with clinical symptoms is a rare manifestation of systemic lupus erythematosus (SLE), despite the relatively high prevalence of myocarditis at autopsies of SLE patients. In this review, we report the case of a 19-year-old male SLE patient who initially presented with myopericarditis and was successfully treated with high dose of glucocorticoids.
Myocardial involvement is not uncommon in systemic lupus erythematosus (SLE). Sometimes lupus myocarditis can be a life-threatening complication of SLE. But, SLE-related myopericarditis is very rare in a young male patient.
We report a case of SLE-associated myopericarditis in a young male without clear evidence of viral infection based on viral markers in blood. The patient's cardiac function dramatically improved after treatment with steroids without any additional complications.
A 19-year-old male was admitted to the Combined Armed Forces Hospital with a 7-day history of fever, cough, dyspnea, orthopnea, and chest pain. Based on the chest radiograph and computed tomography, he was diagnosed with a pericardial effusion and pneumonia (Fig. 1A), and was transferred to our hospital for evaluation of the cause and treatment. His medical and family histories were unremarkable.
On examination, his blood pressure was 110/70 mmHg, pulse rate was 112 beats/min, respiratory rate was 24 breaths/min, and body temperature was 38℃. Jugular veins were engorged. On cardiac auscultation, the cardiac rhythm was regular and rapid, summation gallops were heard at the cardiac apex, and there were pericardial friction rubs along with left lower sternal border in the sitting position. Bilateral pretibial pitting edema was present on admission.
On admission, blood tests showed white blood cell count of 5,420/mm3, hemoglobin 10.6 g/dL and platelet count of 94,000/mm3. C-reactive protein was 4.59 mg/L (normal, 0-3 mg/L). The blood chemistry revealed blood urea nitrogen to be 24.0 mg/dL, creatinine 1.1 mg/dL, total protein 5.7 g/dL, and albumin 2.6 g/dL. Quantitative analysis of proteinuria revealed 8.0 g/day of proteinuria.
He had hypoxemia due to ventilation-perfusion mismatch. The levels of cardiac markers were elevated; troponin-I 0.87 ng/mL (normal, 0-0.05 ng/mL) and myoglobin 371 ng/dL (normal, 16.3-96.5 ng/dL). Sputum smear and polymerase chain reaction tests were negative for acid-fast bacillus. An electrocardiogram (ECG) revealed sinus tachycardia and diffuse T-wave inversion in which leads (Fig. 2A). Echocardiography demonstrated severe left ventricular systolic dysfunction {left ventricular ejection fraction (LVEF) was 18%} with severe global hypokinesia and preserved wall thickness (Fig. 2B). A large amount of pericardial effusion was observed 13 mm anterior to the right ventricle, 18 mm around the right atrium and 2 mm posterior to the LV. There were no signs of cardiac tamponade on both echocardiography and clinical findings. At first, we suspected viral myopericarditis, and started conservative treatment for congestive heart failure and pericarditis. But, there was no improvement in LVEF as well as in the clinical findings. Viral markers for cytomegalovirus, Coxsackie virus B type 2, Herpes simplex virus, and Epstein-Barr virus were all negative. During conservative treatment, he complained of new-onset ankle joint pain and tender erythematous swellings in both the ankles. The immunofluorescence tests were positive for anti-nuclear antibody (1 : 640 titre), anti-dsDNA antibodies (683.4 IU/mL), and anti-extractable nuclear antigen antibodies (anti-Sm, anti-RNP, anti-Ro, and anti-La), and the complement level was low (Table 1). We concluded that the patient had SLE according to the American Rheumatism Association/American College of Rheumatology classification criteria for SLE. On the 13th day of admission, we started treatment with high-dose glucocorticoids (methylprednisolone 1,000 mg intravenously daily for three days followed by 1 mg/kg per day in divided doses). On follow-up examination, ECG showed normalization of T-wave inversion (Fig. 2C) and echocardiography obtained just before discharge showed improved systolic function (Fig. 2D). Chest X-ray also showed improving consolidation in both the lung fields and cardiomegaly (Fig. 1B). Complement 3 was normalized and anti-dsDNA antibodies decreased from 683.4 IU/mL to 383.8 IU/mL (WHO u/mL, normal 0-93). He was discharged on the 33rd day of admission with oral prednisolone, and he visited the outpatient department 1 month later. In this 1 month, he had no symptoms. Echocardiography revealed normal LVEF, without significant valvular disease and pericardial effusion compared to the last examination (Table 2). Subsequently, the steroid medication was tapered and it was planned to maintain him on SLE-specific treatment in the Rheumatologic department.
SLE is an autoimmune inflammatory disease of unknown etiology that affects various parts of the body, including all components of the cardiovascular system.1) The prevalence of lupus ranges from approximately 40-150 cases per 100,000 in the USA.2) In adults, the female-to-male ratio is 7-15 : 1.3)
Cardiac involvement in SLE may comprise of involvement of the pericardium, myocardium, endocardium, heart valves, and coronary or pulmonary arteries.4)
Pericardial involvement is the most frequent cause of symptomatic cardiac disease5) and is the most common echocardiographic finding in SLE patients. The pericardium can be involved by acute and chronic inflammatory changes; granular deposition of immunoglobulin and C3, demonstrated by direct immunofluorescence,6) supporting the role of immune complexes in the development of pericarditis.
Myocarditis is an uncommon, often asymptomatic manifestation of SLE with a prevalence of 8-25% in different studies.7) Global hypokinesis may be an echocardiographic indication of myocarditis and is present in approximately 6% of SLE patients.8) The gold standard for diagnosing myocarditis in SLE remains the endomyocardial biopsy.9) However, an endomyocardial biopsy is invasive with procedure-related risks and the diagnostic yield is low in 10-20% of cases, so it is not powerful enough to confirm the diagnosis.10) Lupus myocarditis can be diagnosed based on clinical suspicion and echocardiographic evidence of a reduced LVEF and segmental or global wall motion abnormality, once the other etiologies, such as viral and ischemic cardiomyopathy, have been excluded.9)11)
Immunofluorescence studies demonstrate fine granular immune complexes and complement deposition in the walls and perivascular tissues of myocardial blood vessels, supporting the hypothesis that lupus myocarditis is an immune complex-mediated disease.
The treatment of lupus myopericarditis has not been assessed in controlled trials.
Lupus myocarditis, although mild, has to be treated immediately with high-dose corticosteroids. In the most severe forms, it is necessary to use intravenous pulse corticosteroid therapy (methylprednisolone 1 g/day for three consecutive days) followed by high doses of oral prednisone. Immunosuppressants, namely cyclophosphamide or azathioprine, and intravenous IgG may be beneficial in the treatment of myocarditis.5) Early mechanical circulatory supports help to save the life and prevent multi-organ failures in patients with fulminant myocarditis.12)
In the present case, the patient was initially diagnosed with myopericarditis on the basis of his symptoms, diffuse T-wave inversion on ECG, elevated cardiac markers and echocardiographic findings. He was given conservative management with angiotensin-converting enzyme inhibitors and diuretics. However, there was no improvement in his symptoms and the common cardiotrophic viral markers were all negative. Also, the patient had pericarditis, thrombocytopenia and proteinuria. Because the previous typical clinical signs and the positive immunofluorescence tests were suitable for making the diagnosis of SLE, we confirmed the diagnosis of myopericaditis associated with SLE in this patient. After a provisional diagnosis of myopericarditis with SLE was made, he was treated with intravenous corticosteroid pulse therapy (methylprednisolone 1 g/day for three consecutive days) followed by high doses of oral prednisone. After 3 days of steroid therapy, the patient's signs and symptoms were stabilizing and echocardiographic findings were improved.
Initially, we had considered myopericarditis to be caused by viral infection; however, the final diagnosis was myopericarditis during presentation of primary SLE based on the clinical manifestations, echocardiography, immunofluorescence tests and good response to steroid therapy. Because the treatment of SLE induced myopericarditis should be needed for some specific therapy such as corticosteroid, this case shows that careful investigation is needed for search of the cause of myopericarditis in a young male, and not only viral infection but also autoimmune disease should be investigated for.
In this report, we described the first case of a Korean young male SLE patient in whom the first manifestation was of myopericarditis and treatment with glucocorticoids resulted in a good clinical outcome.
Figures and Tables
Fig. 1
Chest X-ray. A: chest X-ray shows patchy consolidation with multiple nodular densities in both the lower lung fields and cardiomegaly. B: chest X-ray following treatment with steroids shows improving consolidation and cardiomegaly.
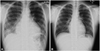
Fig. 2
Electrocardiogram and Echocardiogram. A: electorcardiogram (ECG) shows sinus tachycardia and diffuse T-wave inversion in which leads on the day of admission. B: parasternal short axis view shows pericardial effusion and decreased left ventricular ejection fraction. C: ECG shows normal sinus rhythm and left ventricular hypertrophy after glucocorticoid treatment. D: parasternal short axis views show improving left ventricular ejection fraction and decreasing pericardial effusion after glucocorticoid treatment.

References
1. Tan EM, Cohen AS, Fries JF, et al. The 1982 revised criteria for the classification of systemic lupus erythematosus (SLE). Arthritis Rheum. 1982. 25:1271–1277.
2. Chakravarty EF, Bush TM, Manzi S, Clarke AE, Ward MM. Prevalence of adult systemic lupus erythematosus in California and Pennsylvania in 2000: estimates obtained using hospitalization data. Arthritis Rheum. 2007. 56:2092–2094.
3. Lahita RG. The role of sex hormones in systemic lupus erythematosus. Curr Opin Rheumatol. 1999. 11:352–356.
4. Wijetunga M, Rockson S. Myocarditis in systemic lupus erythematosus. Am J Med. 2002. 113:419–423.
5. Doria A, Iaccarino L, Sarzi-Puttini P, Atzeni F, Turriel M, Petri M. Cardiac involvement in systemic lupus erythematosus. Lupus. 2005. 14:683–686.
6. Bidani AK, Roberts JL, Schwartz MM, Lewis EJ. Immunopathology of cardiac lesions in fatal systemic lupus erythematosus. Am J Med. 1980. 69:849–858.
7. Mandell BF. Cardiovascular involvement in systemic lupus erythematosus. Semin Arthritis Rheum. 1987. 17:126–141.
8. Moder KG, Miller TD, Tazellar HD. Cardiac involvement in systemic lupus erythematosus. Mayo Clin Proc. 1999. 74:275–284.
9. Feldman AM, McNamara D. Myocarditis. N Engl J Med. 2000. 343:1388–1398.
10. Murphy JG, Franz RP. Cooper LT, editor. Endomyocardial biopsy in myocarditis. Myocarditis: From Bench to Bedside. 2003. Totowa, NJ: Humana, Press;371–389.
11. Noutsias M, Pauschinger M, Poller WC, Schultheiss HP, Kühl U. Current insights into the pathogenesis, diagnosis and therapy of inflammatory cardiomyopathy. Heart Fail Monit. 2003. 3:127–135.
12. Park JI, Jeon ES. Mechanical circulatory supports in the treatment of fulminent myocarditis. Korean Circ J. 2005. 35:563–572.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download