Abstract
Background and Objectives
Renal insufficiency (RI) has been reported to be associated with unfavorable clinical outcomes in patients undergoing percutaneous coronary interventions (PCI). However, little data is available regarding the impact of moderate to severe RI on clinical outcomes in patients with acute myocardial infarction (AMI) undergoing PCI.
Subjects and Methods
Between March 2003 and July 2007, 878 patients with AMI who underwent PCI were enrolled. Based on estimated glomerular filtration rate (eGFR) using the Modification of Diet in Renal Disease (MDRD) equation, patients were divided into two groups: eGFR <60 mL/min·m2 (moderate to severe RI, group A) and eGFR ≥60 mL/min·m2 (normal to mild RI, group B). The primary endpoint was all-cause mortality at 1-year after successful PCI. The secondary endpoints were non-fatal myocardial infarction (MI), target lesion revascularization (TLR), target vessel revascularization (TVR), stent thrombosis (ST) and major adverse cardiac events (MACE) at 1-year.
Results
In group A, patients were more often male and older, with diabetes and hypertension. Compared to patients in group B, group A showed significantly higher incidences of all-cause mortality, cardiac mortality, non-fatal MI and MACE. The needs of TLR and TVR, and the incidence of ST were not significantly different between the two groups. Independent predictors of 1-year mortality were eGFR <60 mL/min·m2, male gender, older age and a lower left ventricular ejection fraction.
Renal insufficiency (RI) has been reported to be one of the most important risk factors of mortality in patients who undergo percutaneous coronary intervention (PCI).1) It is also known to be associated with poor cardiovascular outcomes in patients with acute myocardial infarction (AMI).2-5) Little is known, though, about the impact of moderate to severe RI on the long-term clinical outcome in patients with AMI who undergo PCI. In fact, moderate to severe RI has been excluded in most large clinical trials because of both the high rate of comorbidity and the failure to use adequate medications such as β-blockers and acetylcholine esterase inhibitor, due to the hemodynamic instability during the procedure and admission period.6)
A Recent study showed that estimated glomerular filtra-tion rate (eGFR) <60 mL/min·m2 was associated with unfavorable clinical outcomes in patients undergoing PCI.1)7) The RI with eGFR <60 mL/min·m2 may be a pre-clinical sign of end-stage renal disease which has been documented to have a poor clinical outcome in patients with AMI who undergo PCI.8) Therefore, the purpose of this study was to evaluate the impact of moderate to severe RI (eGFR <60 mL/min·m2) on the clinica outcomes in patients with AMI who undergo PCI.
Between March 2003 and July 2007, 878 patients with AMI (within 72 hours) who underwent PCI were consecutively enrolled. Patients with ST-segment elevation MI (STEMI) underwent primary PCI, and patients with non-ST segment elevation MI (NSTEMI) underwent emergent or elective PCI. Patient age was limited to 18 to 80 years. Based on eGFR, using the Modification of Diet in Renal disease (MDRD) equation, patients were divided into two groups: group A, with eGFR <60 mL/min·m2 (moderate to severe RI; n=255) and group B, with eGFR ≥60 mL/min·m2 (normal to mild RI; n=623). Dermographic, clinical, and angiographic characteristics, as well as follow-up data were collected in both groups. Medical records were reviewed and family members were interviewed, when necessary, to determine cause of death.
Exclusion criteria were as follows: 1) thrombolysis before PCI, 2) cardiogenic shock, 3) acute renal failure before PCI, 4) renal transplantation before PCI, 5) under dialysis at the time of presentation.
Renal function was estimated according to the calculated creatinine clearance which was derived from eGFR, which in turn was estimated from the concentration of serum creatinine at admission, before PCI, by using MDRD equation : eGFR (mL/min per 1.73 m2 of body surface)=186×{serum creatinine (mg/dL)}-1.154×{age (in years)}-0.203 (for women, the value was multiplied by 0.742). This equation is from the 2002 Kidney Disease Outcomes Quality Initiative (KDOQI) guideline,9) and has a close correlation with measured GFR (correlation coefficient 90.3).
Myocardial infarction was defined by the presence of two of three criteria: chest pain persisting at least 20 minutes, electrocardiographic changes and cardiac enzyme level increased to at least twice the upper limit of the normal range.10) The number of diseased coronary arteries was defined by those major coronary arteries with luminal diameter stenosis greater than or equal to 70%. As well, patients with stenosis of the left main coronary artery that was more than or equal to 50% were considered as having two-vessel disease. Successful PCI was achieved if procedural success was obtained, defined as no remaining vessel stenosis more than or equal to 30%, without in-hospital major adverse cardiac events (MACE).
Mortality from cardiac disease, non-fatal MI, target lesion revascularization (TLR), target vessel revascularization (TVR) and stent thrombosis (ST) were included in MACE. Cardiac death was considered to have occurred if death was associated with documented MI or other cardiac causes, such as congestive heart failure and arrhythmia. ST was recorded according to the definition of the American Research Consortium.11)
The relationship between presence of certain characteristics or risk factor and clinical outcome was evaluated by binary comparison with the Pearson chi-square test and presented as counts and percentages. The associations between continuous variables were evaluated using ANOVA test and were presented as their means and standard deviations. After testing all variables with univariate analysis, those with p-value less than 0.1 and with possible risk factors documented in previous studies were entered in a multivariate Cox proportional hazards regression model, in order to evaluate independent predictive power for mortality and MACE. The event-free survival curves were constructed using the Kaplan-Meier method. P≤0.05 were considered significant. The Statistical Package for the Social Sciences (SPSS) software package (version 15.0 for windows; SPSS Inc., Chicago, IL, USA) was used for statistical analysis.
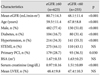
The baseline demographics are shown in Table 1. The study population consisted of 878 patients including 385 with STEMI and 493 patients with NSTEMI. Patients tended to be older and male, diabetic and hypertensive in group A (p<0.001 for all comparisons). Left ventricular ejection fraction (LVEF) and incidence of STEMI were not significantly different between the two groups.
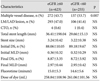
Angiographic results are demonstrated in Table 2. The incidence of multiple vessel disease was higher in group A. Diseased vessel, stent length, stent size, initial diameter of stenosis and presence of chronic total occlusion were not different between two groups.
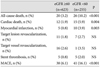
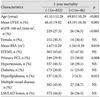
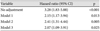
Mean follow-up period was 381.0±34.9 days. The 1-year follow-up results are shown in Table 3. The incidence of all-cause mortality was 10.2% in group A and 3.2% in group B (p<0.001), and cardiac mortality rate was 5.9% in group A and 1.9% in group B (p=0.004). The incidence of non-fatal MI was 3.9% in group A and 0.8% in group B (p=0.003). Th-erefore the incidence of MACE was significantly higher in group A than it was in group B (16.1% vs. 6.1%, p<0.001). However the needs of TLR, TVR and ST were not significantly different between two groups. Risk factors of 1-year mortality were shown in Table 4. Multivariate analysis identified that eGFR <60 mL/min·m2, male gender, older age and lower LVEF were independent predictors of 1-year mortality (Table 5). Hazard ratios for 1-year mortality of eGFR <60 mL/min·m2, male gender, age and LVEF were 2.02 {95% confidence interval (CI), 1.05-3.87; p=0.033}, 2.52 (95% CI, 1.19-5.32; p=0.015), 1.06 (95% CI, 1.03-1.10; p<0.001) and 0.94 (95% CI, 0.90-0.98; p=0.004), respectively. Hazard ratio for 1-year mortality of eGFR <60 mL/min·m2 with no adjustment was 3.28 (95% CI, 1.83-5.88; p<0.001), and there was significant predictive value after adjustment for age, sex, and LVEF (Table 6).
The occurrence of death during follow-up is depicted in Fig. 1. Kaplan-Meier curves revealed that patients in group A had a higher cumulative rate of death after 1-year follow-up (p<0.001).
This study demonstrated that patients with moderate to severe RI have a significantly higher incidence of all-cause mortality, cardiac mortality, non-fatal MI, and MACE. Furthermore, moderate to severe RI, being male, a higher age and LVEF were independent predictors of 1-year mortality after successful PCI in patients with AMI.
Atherosclerotic risk factors seem to be associated with renal function in the general population. One previous study suggested that age, diabetes and hypertension were related to RI because of the involutional process or atherosclerotic changes.12) However, there has been controversy in defining gender as a risk factor of RI. Hsu et al.12) and Plantinga et al.13) demonstrated that RI was more prevalent in males than in females, and in another study, males had an increased risk of RI.1) Increased incidence atherosclerosis is a possible cause of the increased risk of RI in males.
Isolated measurement of plasma creatinine has been commonly used for assessing renal function. However, Levey et al.14) reported the inaccuracy of plasma creatinine for eGFR because plasma creatinine could change easily with the patient's circumstances, such as age and gender. The authors suggested MDRD equation as the most reliable method to estimate GFR, as it takes into consideration both age and gender when estimating GFR. In this study, MDRD equation by KDOQI was used for the estimation of GFR, translating into a more reliable evaluation of real kidney function.
The possible explanations of the unfavorable clinical outcomes in AMI patients with moderate to severe RI are that RI is frequently associated with congestive heart failure and diabetes mellitus which are known to be associated with poor clinical outcomes.5) Moreover, RI itself has a hazardous effect on the patient with AMI, partly due to raised oxidative stress and inflammation,15) alteration of lipid metabolism,16)17) calcium-phosphate homeostasis, elevated homocystein,18)19) coagulation and endothelial dysfunction.20,21) Numerous studies have shown that advanced age, female gender, congestive heart failure, diabetes and RI were important predictors of mortality in patients with end-stage renal disease and AMI,22)24) which is, except for diabetes, in line with our study. In this study, low-density lipoprotein (LDL) levels in patients with diabetes were significantly lower than those of patients without diabetes (121.7±36.6 vs. 129.6±39.1, p=0.014), suggesting that early survelliance of dyslipidemia and vigorous treatment with lipid-lowering agent may affect this result.
Moderate to severe RI was associated with increase of 1-year mortality and MACE in patients with AMI undergoing PCI. Furthermore, eGFR <60 mL/min·m2 using MDRD equation by KDOQI was the strongest predictor of 1-year mortality. Close surveillance, intense medical treatment and lifestyle modification should be required in this patient subset.
This study has several limitations. First, the number of patient is relatively small and, being a retrospective study with a single center experience, it may have a source of selection bias. Also, because of the limited number of patients in each group, it was underpowered to detect a statistical significance. Second, a more stratified RI, such as normal, mild, moderate and severe, could provide a more precise impact of RI on clinical outcomes in this patient subset. Third, patients receiving dialysis were not included in this study. This may have some limitations for evaluation of the real impact of severe RI on patients with AMI undergoing PCI. Fourth, there was no consideration of contrast induced nephropathy. Therefore, a randomized study which is stratified with the grade of RI and which has a larger number of patients will have more value and could be useful to do the future.
Figures and Tables
References
1. Best PJ, Lennon R, Ting HH, et al. The impact of renal insufficiency on clinical outcomes in patients undergoing percutaneous coronary interventions. J Am Coll Cardiol. 2002. 39:1113–1119.
2. Singh M, Rihal CS, Selzer F, Kip KE, Detre K, Holmes DR. Validation of Mayo Clinic risk adjustment model for in-hospital complications after percutaneous coronary interventions, using the National Heart, Lung, and Blood Institute dynamic registry. J Am Coll Cardiol. 2003. 42:1722–1728.
3. Feldman DN, Gade CL, Slotwiner AJ, et al. Comparison of outcomes of percutaneous coronary interventions in patients of three age groups (<60, 60 to 80, and >80 years) (from the New York State Angioplasty Registry). Am J Cardiol. 2006. 98:1334–1339.
4. Gruberg L, Dangas G, Mehran R, et al. Clinical outcome following percutaneous coronary interventions in patients with chronic renal failure. Catheter Cardiovasc Interv. 2002. 55:66–72.
5. Klein LW, Block P, Brindis RG, et al. Percutaneous coronary interventions in octogenarians in the American College of Cardiology-National Cardiovascular Data Registry: development of a nomogram predictive of in-hospital mortality. J Am Coll Cardiol. 2002. 40:394–402.
6. Beattie JN, Soman SS, Sandberg KR, et al. Determinants of mortality after myocardial infarction in patients with advanced renal dysfunction. Am J Kidney Dis. 2001. 37:1191–1200.
7. Zhang RY, Zhu ZB, Zhang Q, et al. Impact of moderate or severe renal insufficiency on long-term outcomes in patients undergoing drug-eluting stent based coronary intervention. Int J Cardiol. 2009. 136:72–79.
8. Yamaguchi J, Kasanuki H, Ishii Y, et al. Prognostic significance of se-rum creatinine concentration for in-hospital mortality in patients with acute myocardial infarction who underwent successful primary percutaneous coronary intervention (from the Heart Institute of Japan Acute Myocardial Infarction [HIJAMI] Registry). Am J Cardiol. 2004. 93:1526–1528.
9. Kidney National Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002. 39:2 Suppl 1. S1–S266.
10. Shlipak MG, Heidenreich PA, Noguchi H, Chertow GM, Browner WS, McClellan MB. Association of renal insufficiency with treatment and outcomes after myocardial infarction in elderly patients. Ann Intern Med. 2002. 137:555–562.
11. Cutlip DE, Windecker S, Mehran R, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007. 115:2344–2351.
12. Hsu CY, Iribarren C, McCulloch CE, Darbinian J, Go AS. Risk factors for end-stage renal disease: 25-year follow-up. Arch Intern Med. 2009. 169:342–350.
13. Plantinga LC, Boulware LE, Coresh J, et al. Patient awareness of chronic kidney disease: trends and predictors. Arch Intern Med. 2008. 168:2268–2275.
14. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. Modification of Diet in Renal Disease Study Group. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med. 1999. 130:461–470.
15. Kanani PM, Sinkey CA, Browning RL, Allaman M, Knapp HR, Haynes WG. Role of oxidant stress in endothelial dysfunction produced by experimental hyperhomocyst(e)inemia in humans. Circulation. 1999. 100:1161–1168.
16. Massy ZA, Kasiske BL. Hyperlipidemia and its management in renal disease. Curr Opin Nephrol Hypertens. 1996. 5:141–146.
17. Romanic AM, Arleth AJ, Willette RN, Ohlstein EH. Factor XIIIa cross-links lipoprotein(a) with fibrinogen and is present in human atherosclerotic lesions. Circ Res. 1998. 83:264–269.
18. Busch M, Franke S, Muller A, et al. Potential cardiovascular risk factors in chronic kidney disease: AGEs, total homocysteine and metabolites, and the C-reactive protein. Kidney Int. 2004. 66:338–347.
19. Bjorkbacka H, Kunjathoor VV, Moore KJ, et al. Reduced atherosclerosis in MyD88-null mice links elevated serum cholesterol levels to activation of innate immunity signaling pathways. Nat Med. 2004. 10:416–421.
20. Cheung AK, Sarnak MJ, Yan G, et al. Atherosclerotic cardiovascular disease risks in chronic hemodialysis patients. Kidney Int. 2000. 58:353–362.
21. Choi JH, Kim KL, Huh W, et al. Decreased number and impaired angiogenic function of endothelial progenitor cells in patients with ch-ronic renal failure. Arterioscler Thromb Vasc Biol. 2004. 24:1246–1252.
22. Herzog CA, Ma JZ, Collins AJ. Poor long-term survival after acute myocardial infarction among patients on long-term dialysis. N Engl J Med. 1998. 339:799–805.
23. Chertow GM, Normand SL, Silva LR, McNeil BJ. Survival after acute myocardial infarction in patients with end-stage renal disease: results from the cooperative cardiovascular project. Am J Kidney Dis. 2000. 35:1044–1051.
24. Wright RS, Reeder GS, Herzog CA, et al. Acute myocardial infarction and renal dysfunction: a high-risk combination. Ann Intern Med. 2002. 137:563–570.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download