Abstract
Background and Objectives
Percutaneous cardiopulmonary support (PCPS) has proven to be a valuable technique in high-risk coronary patients undergoing percutaneous coronary intervention (PCI). However, there have been few studies on PCI associated with PCPS in Korea. We summarized our experience with PCPS-supported PCI.
Subjects and Methods
We retrospectively reviewed 19 patients with PCPS-supported PCI between August 2005 and June 2009. PCPS was used as an elective procedure for 10 patients with at least two of the following conditions: left-ventricular ejection fraction <35%, target vessel(s) supplying more than 50% of the viable myocardium, high risk surgical patients, and patients who refused coronary bypass surgery. In the remaining 9 patients PCPS was used as an emergency procedure, to stabilize and even resuscitate patients with acute myocardial infarction and cardiogenic shock, in order to attempt urgent PCI.
Results
Among the 19 patients who were treated with PCPS-supported PCI, 11 (57.9%) survived and 8 (42.1%) patients did not. ST elevation myocardial infarction with cardiogenic shock was more prevalent in the non-survivors than in the survivors (75% vs. 27.3%, p=0.04). The elective PCPS-supported PCI was practiced more frequently in the survivors than in the non-survivors (72.7% vs. 25%, p=0.04). In the analysis of the event-free survival curve between elective and emergency procedures, there was a significant difference in the survival rate (p=0.025). Among the survivors there were more patients with multi-vessel disease, but a lower Thrombolysis in Myocardial Infarction grade in the culprit lesions was detected in the non-survivors, before PCI. Although we studied high-risk patients, there was no procedure-related mortality.
Percutaneous cardiopulmonary support (PCPS) provides hemodynamic support via the femoral artery and vein, using a closed artificial heart-lung system which is usually composed of a centrifugal pump and a membranous artificial lung.1)2) In terms of cardiac failure, the most common indications for PCPS are post-cardiotomy (in which cardiopulmonary bypass cannot be taken off the patient following cardiac surgery), post-heart transplant (usually due to primary graft failure) and severe cardiac failure due to almost any other cause (eg., decompensated cardiomyopathy, myocarditis, acute coronary syndrome with cardiogenic shock, profound cardiac depression due to drug overdose or sepsis). In terms of respiratory failure, the most common indications include adult respiratory distress syndrome, pneumonia, trauma, and primary graft failure following lung transplantation.2-4) In particular, PCPS has proven to be a technique of value in high-risk coronary patients who undergo percutaneous coronary intervention (PCI).5-9) However, there have been few studies on PCPS-supported PCI in Korea. Thus, we summarized our experience with PCPS-supported PCI.
We combined the use of PCPS and coronary stent revascularization in 19 patients between August 2005 and June 2009, at the Yonsei Cardiovascular Center. PCPS was used as an elective procedure in 10 patients who satisfied at least two of the selection criteria: left ventricular ejection fraction (LVEF) <35%, target vessel(s) supplying more than 50% of the viable myocardium, high risk surgical patients {old age, impending end stage of renal disease, chronic obstructive pulmonary disease, a history of coronary artery bypass graft surgery (CABG)}, and patients who refused CABG surgery. In the remaining 9 patients, PCPS was used as an emergency procedure to stabilize and even resuscitate patients with acute myocardial infarction (AMI) and cardiogenic shock, in order to attempt urgent PCI. We compared the clinical characteristics, PCPS and angiographic findings, and clinical outcomes of the survivors and non-survivors.
The PCPS system used in our study was the Capiox Emergency Bypass System® (Terumo, Inc., Tokyo, Japan), which is an all-in-one package of a heparin-coated membrane oxygenator that is preassembled with bypass circuits and a cone for the centrifugal pump. The PCPS apparatus is ready for emergency use, by a well-trained team at our hospital, ready to prepare the patient for pump placement within minutes. For the percutaneous technique, the tip of the arterial cannula was advanced and positioned in the common iliac artery; the tip of the venous catheter was placed at the junction of the right atrium and the superior vena cava along a rigid backup guidewire under the fluoroscopic guidance. The patients were fully heparinized with continuous injection at the rate of 3 mg/kg/min, to maintain an activated clotting time greater than 200 seconds. The pump and cannulas were purged, and extracorporeal circulation was initiated. The centrifugal pump provided a non-pulsatile flow at a rate between 1 and 5 L/min. During the procedure the flow was increased or decreased with inotropic drugs or fluids as needed. Then, both cannulas were clamped, and the pump was interrupted. At this point, one-to-one protamine neutralization of the circulating heparin was performed, allowing removal of the cannulas and prolonged groin compression.
The data are expressed as means±standard deviations for the continuous variables, and as absolute and relative frequencies for the categorical variables. Student's unpaired t-test was used to compare the continuous variables between the groups. Categorical variables were compared with using the Chi-square test. Event-free survival curves were constructed by the use of the Kaplan-Meier method. Probability values <0.05 were considered to be statistically significant.
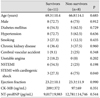
The demographics and pre-existing co-morbidities were similar between the survivors and non-survivors. Unstable angina and non-ST elevation myocardial infarction patients were more common among the survivors; ST elevation myocardial infarction (STEMI) with cardiogenic shock was more prevalent in the non-survivor group compared to the survivors (75% vs. 27.3%, p=0.04). EF was not significantly different between the survivors and non-survivors. The cardiac biomarkers (creatine kinase-MB, N-terminal pro-B-type natriuretic peptide) were not significantly different between the survivors and non-survivors either (Table 1).
The elective PCPS-supported PCI was more frequently practiced among the survivors compared to the non-survivors (72.7% vs. 25%, p=0.04). All patients were weaned from PCPS in the survivor group and 6 (75%) patients were weaned from PCPS among the non-survivors. The median durations of PCPS support were not significantly different between the survivors and non-survivors. There were no significant differences in culprit lesions between the survivors and non-survivors. More patients with multi-vessel disease were in the survivors than in the non-survivors (90.9% vs. 50%, p=0.046), however, a lower Thrombolysis in Myocardial Infarction (TIMI) grade (0-1) in the culprit lesions before PCI was detected among the non-survivors. After PCI, TIMI grade 3 was maintained in all patients. There were no significant differences in the use of Intra-aortic balloon pump (IABP) or in the number of stents between the survivors and non-survivors (Table 2).
Patients who survived were discharged from the hospital and closely followed at the outpatient department. The mean clinical follow-up period was 541.1±548.6 days. Overall in-hospital mortality was 31.6% (6 of 19), of which 4 deaths were cardiac-related and 2 were not. The causes of non-cardiac-related deaths were sepsis associated with pneumonia and upper gastrointestinal bleeding (Table 3). We also compared the survival rates of patients who underwent elective procedure and emergency procedure. In the analysis of the event free survival curve between elective procedure and emergency procedure, there were significant differences in the survival rate (p=0.025) (Fig. 1). Although we studied high-risk patients, there was no procedure-related mortality. The most common complications were hematomas near the catheter insertion site, which disappeared by the time of discharge from hospital. One patient who underwent emergency procedure had lower limb ischemia and gangrene, but survived without sequelae.
Based on the results of previous studies the application of PCPS-supported PCI on high risk patients with severe LV dysfunction is accepted as helpful.5-9) PCPS provides complete systemic hemodynamic support independent of intrinsic cardiac function and rhythm, and has been successfully used prophylactically in high-risk patients during PCI. This preventative support allows for precise diagnostic and therapeutic occlusive maneuvers {e.g., Intravascular ultrasound (IVUS), kissing balloon of bifurcated lesions} while preserving systemic perfusion pressures, and preventing both circulatory collapse and malignant arrhythmia.10)11) In one study, although it was from a small number of patients, the authors recommended prophylactic cardiopulmonary bypass support in unstable patients undergoing angioplasty with EF <25%, or in patients whose EF is low and in whom the only patent artery is the target of dilatation.12) Even stable patients with EF <20% may benefit from prophylactic cardiopulmonary bypass support.7) PCPS may also be helpful when used as an emergency procedure to recover hemodynamic stability in patients with AMI and cardiogenic shock. PCPS markedly decreases myocardial oxygen consumption and work, creating favorable hemodynamic conditions to impede progression of myocardial infarction. Complications such as ventricular arrhythmias frequently appear in cardiogenic shock and are also transient and reversible under PCPS. Once the patient is stabilized, a coronary angiogram can be safely performed, after which a planned reperfusion and stent revascularization can be accomplished.13-15) In 1995, Ha et al.16) reported, for the first time, a successful case of PCPS-supported PCI on a high risk patient. In 2006, Rhee et al.17) reported the effectiveness of PCPS on patients with cardiac arrest or cardiogenic shock.
We analyzed, for the first time in Korea, the high-risk patients who underwent PCPS-supported PCI, being the elective case group and emergency case group. Even though the patients in both groups had similar pre-existing co-morbidities and lower EF, the patient conditions were quite different. Those in the emergency group were in shock status even after inotropic drug administration, while patients in the elective group were in a relatively stable condition (under general anesthesia, transfusion, etc.). For this reason, among the survivors, the number of patients who underwent elective PCPS-supported PCI was significantly higher than among the non-survivors. Also the in-hospital mortality rate was lower in the elective case group.
In this study, elective PCPS-supported PCI was applied on 10 patients exhibiting at least two of the following conditions: LVEF <35%, target vessel(s) supplying more than 50% of the viable myocardium, high risk surgical patients and those who refused coronary bypass surgery. PCPS was weaned off from all patients without serious procedure-related complications and there was no procedure-related mortality. Due to underdevelopment of vascular device and stenting technology in the past, procedure-related complications were common in high risk patients who were subjected to application of LV assist.18) In this study, the use of a more advanced vascular device helped reducing procedure-related complications. All patients received drug-eluting stents and even IVUS was done if necessary. We could expect a more favorable prognosis with elective PCPS-supported PCI on high risk patients.
In the case of emergency PCPS-supported PCI, urgent PCI was done to stabilize in patients who showed signs of STEMI with cardiogenic shock and cardiac arrest. PCPS was weaned off quite successfully (in 78% patients) after its application. However, the prognosis was not favorable, resulting in 44.4% of cardiac related death and 55.6% of in-hospital mortality. According to the results of previously published data, AMI with cardiogenic shock led to a ≥80% mortality rate, and IABP, though still applied to lower the mortality rate, resulted a relatively high mortality rate.13)19) In this study, we were unable to restore cardiogenic shock of 5 patients by applying IABP alone, thus need a PCPS-support. In other studies PCPS-supported PCI in emergency cases was more successful than that with IABP support alone.18) Three patients of this study survived after PCPS application and are now under outpatient department follow-up. However, further study about the benefits of this procedure will be needed, considering the small number patients, and their conditions (vital sign, co-morbidities, etc.), in this study.
Our study has some limitations: first, this is a retrospective observational analysis of a relatively very small number of patients. Second, in the elective case group, we have not yet demonstrated that this approach is necessary or superior to unsupported angioplasty or to IABP, or to coronary bypass surgery where feasible. A randomized trial of supported versus unsupported (with cardiopulmonary support on standby) angioplasty maybe warranted. Third, in the emergency case group, we have applied IABP first in most of our cases, thus it is hard to conclude that the benefits came from PCPS alone.
Our experience suggests that PCPS may be helpful in high-risk patients being or to be treated with PCI, especially in the elective cases. However, PCPS-supported PCI still bears considerable risks in the emergent cases. To this day, a clear guideline or indication criteria have not been established for PCPS guided PCI. More aggressive and larger scale studies of PCPS will be needed.
Figures and Tables
Table 2
PCPS and angiographic findings of the study patients

Values are in n (%) or mean±standard deviation. PCPS: percutaneous cardiopulmonary support, LAD: left anterior descending coronary artery, LCx: left circumflex coronary artery, RCA: right coronary artery, Lt main: left main trunk, TIMI: Thrombolysis In Myocardial Infarction, IABP: intra-aortic balloon pump
References
1. Hill J, O'Brient T, Murray J, et al. Prolonged extracorporeal oxygenation for acute post-traumatic respiratory failure (shock-lung syndrome). Use of the Bramson membrane lung. N Engl J Med. 1972. 286:629–634.
2. Phillips S, Zeff R, Kongtahworn C, et al. Percutaneous cardiopulmonary bypass: application and indication for use. Ann Thorac Surg. 1989. 47:121–123.
3. Sawa Y. Percutaneous extracorporeal cardiopulmonary support: current practice and its role. J Artif Organs. 2005. 8:217–221.
4. Marasco SF, Lukas G, McDonald M, McMillan J, Ihle B. Review of ECMO (Extra Corporeal Membrane Oxygenation) support in critically ill adult patients. Heart Lung Circ. 2008. 17:Suppl 4. S41–S47.
5. Vogel RA, Tommaso CL, Gundry SR. Initial experience with coronary angioplasty and aortic valvuloplasty using elective semipercutaneous cardiopulmonary support. Am J Cardiol. 1988. 62:811–813.
6. Shawl FA, Domanski MJ, Punja S, Hernandez TJ. Percutaneous cardiopulmonary bypass support in high-risk patients undergoing percutaneous transluminal coronary angioplasty. Am J Cardiol. 1989. 64:1258–1263.
7. Teirstein P, Vogel R, Dorros G, et al. Prophylactic versus standby cardiopulmonary support for high risk percutaneous transluminal coronary angioplasty. J Am Coll Cardiol. 1993. 21:590–596.
8. Sivananthan MU, Rees MR, Browne TF, et al. Coronary angioplasty in high risk patients with percutaneous cardiopulmonary support. Eur Heart J. 1994. 15:1057–1062.
9. Vogel RA. Cardiopulmonary bypass support of high risk coronary angioplasty patients: registry results. J Interv Cardiol. 1995. 8:193–197.
10. Suarez de Lezo J, Pan M, Medina A, et al. Percutaneous cardiopulmonary support in critical patients needing coronary interventions with stents. Catheter Cardiovasc Interv. 2002. 57:467–475.
11. Vainer J, van Ommen V, Maessen J, Geskes G, Lamerichs L, Waltenberger J. Elective high-risk percutaneous coronary interventions supported by extracorporeal life support. Am J Cardiol. 2007. 99:771–773.
12. Shawl FA, Quyyumi AA, Bajaj S, Hoff SB, Dougherty KG. Percutaneous cardiopulmonary bypass-supported coronary angioplasty in patients with unstable angina pectoris or myocardial infarction and a left ventricular ejection fraction ≤25%. Am J Cardiol. 1996. 77:14–19.
13. Shawl FA, Domanski MJ, Punja S, Hernandez TJ. Emergency cardiopulmonary bypass support in cardiogenic shock from acute myocardial infarction. Am J Cardiol. 1989. 64:967–970.
14. Matsuwaka R, Sakakibara T, Shintani H, et al. Emergency cardiopulmonary bypass support in patients with severe cardiogenic shock after acute myocardial infarction. Heart Vessels. 1996. 11:27–29.
15. Obo H, Kozawa S, Asada T, et al. Emergency percutaneous cardiopulmonary bypass support for acute myocardial infarction. Surg Today. 1998. 28:797–801.
16. Ha JW, Cho SY, Shim WH, et al. Cardiopulmonary support for high risk percutaneous transluminal coronary angioplasty. Korean Circ J. 1995. 25:85–91.
17. Rhee I, Gwon HC, Choi J, et al. Percutaneous cardiopulmonary support for emergency in-hospital cardiac arrest or cardiogenic shock. Korean Circ J. 2006. 36:11–16.
18. Schreiber TL, Kodall UR, O'Neil WW, Gangadharan V, Purchrowicz-Ochocki SB, Grines CL. Comparison of acute results of prophylactic intraaortic balloon pumping with cardiopulmonary support for percutaneous transluminal coronary angioplasty (PCTA). Cathet Cardiovasc Diagn. 1998. 45:115–119.
19. Aguirre FV, Kern MJ, Bach R, et al. Intraaortic balloon pump support during high-risk coronary angioplasty. Cardiology. 1994. 84:175–186.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download