Abstract
Background and Objectives
To determine the level of knowledge of stroke and heart attack (HA) symptoms and risk factors of cardiovascular disease (CVD) in rural elderly people who are at risk for CVD.
Subjects and Methods
A total of 444 adults over the age of 60 living in a rural province of Korea with at least one CVD risk factor participated in this survey.
Results
A total of 72.5% of the participants had hypertension and 28.4% had diabetes, whereas approximately 40% exhibited over two CVD risk factors. The mean knowledge scores for HA symptoms (4.3/9) were lower than scores for stroke symptoms (5.8/9), and the mean knowledge score for risk factors was 7.3/11. Stepwise multiple regression analyses showed that old age, low level of education, and low income level were the determining factors for low knowledge levels of stroke and HA symptoms as well as CVD risk factors. A low perceived risk of stroke or HAs also predicted a low knowledge of CVD risk factors.
Cerebro-cardiovascular diseases (CVD) such as stroke and ischemic heart disease are the second leading cause of death in Korea. In 2008, death rates from stroke and ischemic heart disease among Koreans were 56.5 and 25.7 per 100,000 people, respectively.1) The incidence rate of stroke in Korea is twice as high as that in Western countries.2) The rising incidence of CVD might be related to an increase in the aging population. The older population ≥65 years of age is 9.9% in Korea, which may increase to 14.3% over the next 10 years.1) For people above the age of 65, stroke and ischemic heart disease have been identified as the 3rd and 4th major reasons for hospitalization, respectively.3) Approximately half of the patients enrolled in the Korean Acute Myocardial Infarction Registry and Korean Stroke Registry were over the age of 65.4)5) Old patients with acute myocardial infarction (AMI) and stroke had a markedly high incidence of in-hospital mortality and an increased length of hospital stay, resulting in higher medical expenses.5-7)
The proportion of older people at risk of developing chronic diseases living in rural areas has significantly increased, consequently increasing the financial burden of health care expenditure on families and communities in Korea.11) The current survey was conducted in Jeonnam, a province with the largest proportion of elderly people in Korea: 14.9% of the total population is above the age of 65, with a high proportion of elderly women who live alone.1) Disparities in seeking health services due to education and income levels are leading to emerging social and health issues in Korea, especially for the elderly population in rural areas.8) Elderly people living in rural areas are amongst the most vulnerable populations for developing CVD.
Early recognition of symptoms and prompt medical care are essential for providing appropriate treatment to prevent adverse clinical outcomes in patients with stroke or AMI.9) However, the Korean registry studies showed that only 20.5% of patients with acute ischemic stroke were admitted within 3 hours after symptom onset5) and 40.1% of AMI patients were admitted to hospital 6 hours after the acute event.4) In particular, older adults with stroke or heart attack (HA) symptoms were admitted significantly later to the hospital than younger patients.9) This might be associated with poor recognition of symptoms and risk factors of stroke and HA as well as of required actions. In addition, ischemic stroke and HA have the same lifestyle risk factors, and public awareness of these risk factors is essential. Therefore it is important to identify the level of awareness about stroke and HA symptoms and risk factors in rural elderly people, in an effort to help them prevent and detect CVD.
This study was a descriptive survey to identify the level of knowledge of stroke and HA symptoms, as well as CVD risk factors among rural elderly people.
Elderly people or patients who visited 3 public health care centers and 2 medical centers located in Jeonnam province were included as subjects of this study. People above the age of 60 who had at least one CVD risk factor and were able to communicate verbally were selected. Written permissions from the directors of the community health care and medical centers were obtained for the study. After agreement of a survey method at the meeting, data were collected by 5 trained research assistants, who were senior nursing students. Four hundred and fifty-one individuals participated in the survey, of which 444 provided complete datasets and were selected for further analysis. Data were collected from January to March, 2009.
Informed written consent was obtained from all the study participants. The participants were interviewed individually and the questionnaires were assisted if required. The questionnaire consisted of items pertaining to warning symptoms of stroke and HA as well as CVD risk factors identified by the American Heart Association.10) The structured questionnaire contained 18 items, including 9 stroke and 9 HA warning symptoms, as well as 11 items for CVD risk factors. The questionnaire included terms that have been disclosed as public information by Korean medical and nursing textbooks, and were validated by two nursing professors. One point was given for each correct answer and a zero was given for each incorrect answer; the individual scores were added to obtain a total score. Dichotomous data in the Kuder-Richardson 20 (KR-20) formula were used to calculate the internal consistency of stroke and HA symptoms, and CVD risk factors, and the alphas were 0.80 and 0.85, respectively. In addition, the subjects were also asked what they would do if they thought someone was having a stroke or HA, and their ability to perceive the possible occurrence of a stroke or a HA was assessed.
Data were analyzed using Statistical Package for the Social Sciences version 14.0 (Chicago, IL, USA). Demographic characteristics of the subjects and response rates to symptoms and risk factors were calculated. Chi-square, t-test, and analysis of variance were used to examine the relationship between the demographic variables and knowledge scores of symptoms and CVD risk factors. The total knowledge scores of symptoms regarding stroke and HA, and the knowledge score of CVD risk factors were normally distributed, respectively. There was no presence of multicollinearity between predictor variables in the multiple regression models. Stepwise multiple regression analyses were used to determine the predicting factors for low levels of knowledge of symptoms and CVD risk factors.
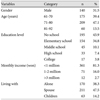
The average age of participants in this study was 72.3 (±7.3) years. A majority of the participants (68.5%) were women. A total of 38.3% of the participants lived alone and 25.5% never received regular health checkups. A total of 72.5% of participants had hypertension and 28.4% had diabetes for average lengths of 7.2±5.9 and 9.1±7.8 years, respectively. Among those who had hypertension or diabetes, 18.7% reported that they no longer visited the doctor nor took any medication. A total of 18% of the participants had a family history of stroke or ischemic heart disease and 39.6% had 2 or more risk factors for CVD. In response to the question on the possibility of stroke and/or HA occurrence, 32.4% reported a possibility of stroke and 31.1% reported a possibility of a HA. In response to the question on the actions that they would take if stroke or HA symptoms occurred, 54.1% reported that they would call emergency services, and 24.3% responded that they would go to the doctor's office and call their family members (Table 1 and 2).
In response to structured questionnaire items on the symptoms of stroke and HA, the participants, on average, accurately identified 5.8 out of the 9 stroke symptoms and 4.3 out of the 9 HA symptoms. The average knowledge score of participants about CVD risk factors was 7.3 out of 11; 78.4% of the participants accurately identified hypertension as a risk factor, and more than 60% of the participants recognized overall CVD risk factors. However, only 47.1% recognized diabetes as a risk factor for CVD. Less than 60% of the participants recognized sudden loss of vision in one or both eyes and nausea or vomiting, as stroke and HA symptoms. Chest pain or discomfort (75.2%) and shortness of breath (70.3%) were the most widely recognized symptoms of a HA. However, less than 50% of the participants were accurately able to identify other HA symptoms (Table 3 and 4).
The results of bivariate analyses are shown in Table 5. There were significant differences between gender, age, education level, monthly income, and knowledge of stroke/HA symptoms and CVD risk factors. The level of knowledge about CVD risk factors was significantly lower in the participants who had no perceptions on the possibility of having a stroke or HA than those who had not (p<0.01). However, there were no significant differences in the levels of knowledge on symptoms and CVD risk factors according to clinical characteristics such as the presence of hypertension or diabetes, the lengths of period of those risk factors, and the number of CVD risk factors. Multiple stepwise regression analyses were conducted to determine the variables that can predict the lower level of knowledge of stroke/ HA symptoms and CVD risk factors. The analyses included all significant variables confirmed by bivariate analyses. Lower education, older age, and lower monthly income were found to be independent predictors of the low knowledge of stroke and HA symptoms. In addition, a low perceived risk of stroke or HA was a predictor of the knowledge of CVD risk factors (Table 6).
The participants identified 7.3 of the 11 CVD risk factors: Hypertension was the most frequently identified risk factor (78.4%), followed by stress (73.0%), whereas diabetes was the least frequently identified risk factor (47.1%). These findings are consistent with earlier reports in Korea which showed that subjects lacked awareness of diabetes as a CVD risk factor.11)12) People who are aware of the risk of stroke and HA may be more likely to engage in preventive practices. Therefore, community-based public education, with particular emphasis on the management of diabetes is needed, in order to prevent stroke or HA among elderly people suffering from diabetes.
More than 70% of the participants identified sudden dizziness, pain on one side of the body, and trouble speaking, as stroke symptoms. This finding was also consistent with a previous report.13) The least identified stroke symptoms were sudden loss of vision in one or both eyes and nausea followed by vomiting. This finding was in agreement with previous studies that showed vision impairment to be the least identified warning symptom.14) More than 60% of the participants of this study did not identify back pain, neck/jaw pain, cold sweat, and nausea as HA symptoms. These findings were also consistent with a previous study of Korean immigrants,15) as well as an additional study of Korean subjects.16) Considering average accurate response rates, the participants of this study reported a limited knowledge about most HA symptoms (4.3/9) except chest pain and shortness of breath, as compared to stroke symptoms (5.8/9). Previous studies have reported that atypical symptoms such as gastrointestinal or respiratory symptoms without chest pain, were the most significant factors for predicting a lower use of thrombolytic therapy, and were associated with in-hospital complications.17)18) Furthermore, patients with an atypical presentation were more likely to be older, female, and have hypertension and/or diabetes.17-19) Thus, public campaigns targeting elderly people and those with diabetes are necessary to improve their awareness of all possible symptoms including the atypical symptoms.
Multiple regression analyses showed that lower levels of education and monthly income, and older age significantly predicted the lower levels of knowledge of stroke and HA symptoms and CVD risk factors. These findings are supported by previous studies.11)20) Similar findings have also been reported in a review of fifteen international studies which showed that elderly people and those with lower levels of education tended to have less knowledge of risk factors and warning signs of stroke as compared to younger age groups and those with higher levels of education.21) A low level of education and old age were also shown to affect HA symptom recognition.22) In this study, 78.6% of the participants attended only elementary school and 81.3% had a monthly income of under one million won. The low levels of education and socioeconomic status were the defining demographics of our elderly population. The knowledge disparity among elderly people needs to be addressed in programs aimed at helping them recognize and take prompt treatment-seeking action through simple guidelines, when early warning symptoms appear.
Participants who had never considered the possibility of having a HA had significantly lower levels of knowledge of CVD risk factors, and this finding was consistent with a previous study.23) Approximately 69% of participants with one or multiple CVD risk factors did not perceive themselves to be at risk of a stroke or HA in this study. The decision to seek treatment is made based on whether the patients believe their physical symptoms to be serious and life threatening.9) Public education can be an effective way to improve awareness of the risk factors for stroke and HA. A previous study reported that a 4 month educational intervention program for elderly adults with a mean age of 75 years was effective in improving awareness about stroke and HA symptoms.24) Therefore, public health education for the elderly at risk of CVD should focus on improving awareness of having a stroke or HA to increase the knowledge of symptoms and risk factors of CVD, and to facilitate preventive actions.
The limitation of this study was that the study subjects were recruited from only one rural province with a high proportion of elderly women and from the clients of community health care centers. Hence, these findings cannot be generalized for all elderly people living in rural areas in other provinces or for home residents.
Knowledge of HA symptoms among rural elderly people in Korea was lower than that of stroke symptoms. Lower education level, older age, and a lower monthly income were predicting factors for a lower knowledge of stroke/HA symptoms and CVD risk factors. In addition, a low perceived risk of HA independently predicted a low knowledge of CVD risk factors. Educational interventions are needed to increase the recognition of early warning symptoms and risk factors for CVD among rural elderly clients visiting community health care or medical centers, particularly those with low levels of education and income.
Figures and Tables
References
1. Cause of death statistics, 2005 to 2008. Korea Statistical Information Service. 2009. Accessed on June 20. Daejeon: Korea Statistical Office;Available from: http://kosis.kr/wnsearch/totalSearch.jsp.
2. Rah JH. Stroke epidemiology 2007 update. Korean J Stroke. 2008. 10:1–4.
3. National health insurance statistical year book 2008. Korea National Health Insurance Corporation. 2009. Accessed on June 20. Seoul: Korea National Health Insurance Corporation;Available from: http://www.nhic.or.kr/portal/site/main/menuitem.
4. Sim DS, Kim JH, Jeong MH. Differences in clinical outcomes between patients with ST-elevation versus non-ST-elevation acute myocardial infarction in Korea. Korean Circ J. 2009. 39:297–303.
5. Yu KH, Bae HJ, Kwon SU, et al. Analysis of 10,811 cases with acute ischemic stroke from Korean Stroke Registry: Hospital-based Multicenter Prospective Registration Study. J Korean Neurol Assoc. 2006. 24:535–543.
6. Assali AR, Moustapha A, Sdringola S, et al. The dilemma of success: percutaneous coronary interventions in patients > or =75 years of age-successful but associated with higher vascular complications and cardiac mortality. Catheter Cardiovasc Interv. 2003. 59:195–199.
7. Schuler J, Meier B, Behrens S, Thimme W. Present treatment of acute myocardial infarction in patients over 75 years: data from the Berlin Myocardial Infarction Registry. Clin Res Cardiol. 2006. 95:360–367.
8. Ku IH. Income Disparity and Poverty in Korea: The Aggravation of Income Distribution and the Task of Social Security Policy. 2006. Seoul: Seoul National University.
9. Moser DK, Kimble LP, Alberts MJ, et al. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on cardiovascular nursing and stroke council. Circulation. 2006. 114:168–182.
10. Rosamond W, Flegal K, Furie K, et al. Heart disease and stroke statistics-2008 update: a report of American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008. 117:e25–e146.
11. Han NY, Ko EA, Hwang SY. Knowledge of stroke symptoms and risk factors among older adults. J Korean Acad Adult Nurs. 2009. 21:314–323.
12. Kim JS, Yoon SS. Perspective of stroke in persons living in Seoul: a survey of 1000 subjects. Stroke. 1997. 28:1165–1169.
13. Blades LL, Oser CS, Dietrich DW, et al. Rural community knowledge of stroke warning signs and risk factors. Prev Chronic Dis. 2005. 2:A14.
14. Hwang SY, Zerwic JJ. Knowledge of stroke symptoms and risk factors among Korean immigrants in the United States. Res Nurs Health. 2006. 29:337–344.
15. Hwang SY, Ryan CJ, Zerwic JJ. Korean immigrants' knowledge of heart attack symptoms and risk factors. J Immigr Minor Health. 2008. 10:67–72.
16. Kim cJ, Huh HK, Lee JK. A study on knowledge about myocardial infarction in Korean population. J Korean Acad Adult Nurs. 1999. 11:288–297.
17. Canto JG, Shlipak MG, Rogers WJ, et al. Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. JAMA. 2000. 283:3223–3229.
18. Brieger D, Eagle KA, Goodman SG, et al. Acute coronary syndromes without chest pain, an underdiagnosed and undertreated high-risk group: insights from the Global Registry of Acute Coronary Events. Chest. 2004. 126:461–469.
19. Seok JH, Kwun JY, Lee JL, et al. The characteristics of clinical presentation and in-hospital outcome of acute myocardial infarction patients older than 65 years of age. Korean Circ J. 1997. 27:386–393.
20. Lutfiyya MN, Lipsky MS, Bales RW, Cha I, McGrath C. Disparities in knowledge of heart attack and stroke symptoms among adult men: an analysis of behavioral risk factor surveillance survey data. J Natl Med Assoc. 2008. 100:1116–1124.
21. Nicol MB, Thrift AG. Knowledge of risk factors and warning signs of stroke. Vasc Health Risk Manag. 2005. 1:137–147.
22. Greenlund KJ, Keenan NL, Giles WH, et al. Public recognition of major signs and symptoms of heart attack: seventeen states and the US Virgin Islands, 2001. Am Heart J. 2004. 147:1010–1016.
23. Harwell TS, Blades LL, Oser CS, et al. Perceived risk for developing stroke among older adults. Prev Med. 2005. 41:791–794.
24. Bell M, Lommel T, Fischer JG, Lee JS, Reddy S, Johnson MA. Improved recognition of heart attack and stroke symptoms after a community-based intervention for older adults, Georgia, 2006-2007. Prev Chronic Dis. 2009. 6:A41.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download