Abstract
Background and Objectives
Patent ductus arteriosus (PDA) is associated with increased morbidity and mortality in premature infants. Therefore, an early diagnosis and treatment of a hemodynamically significant PDA are very important. A widened pulse pressure is considered to be a well known clinical sign of a PDA in older infants and children; however, whether this is also applicable in the case of preterm infants remains to be confirmed. The aims of this study were to investigate the change in blood pressure (BP) before and after medical treatment of a PDA with indomethacin and to evaluate if the change in the pulse pressure in preterm infants with a medically treated PDA could be used as a reliable clinical predictor of a hemodynamically significant PDA.
Subjects and Methods
Between January 2005 and June 2009, a retrospective analysis was performed in preterm infants with a hemodynamically significant PDA (PDA group, n=72) and preterm infants without a PDA (control group, n=72) at the Chonnam National University Hospital Neonatal Intensive Care Unit. The PDA was closed by treatment with indomethacin. The BP was compared between the two groups over the seven days after the first dose of indomethacin.
Results
In preterm infants with a hemodynamically significant PDA, the mean systolic (55.1±6.0 mmHg) and diastolic BPs (31.4±6.2 mmHg) were lower than those in the controls (mean systolic BP 58.0±6.4 mmHg, mean diastolic BP 34.7±6.0 mmHg) before indomethacin treatment. When the ductus arteriosus was successfully closed by indomethacin treatment, there was a gradual increase in both the systolic and diastolic BPs without any change in the pulse pressure.
Conclusion
The results of this study show that a widened pulse pressure is not a useful clinical sign of a hemodynamically significant PDA in preterm infants. However, low systolic and diastolic BPs may be useful clinical signs of a hemodynamically significant PDA in preterm infants. If the systolic and diastolic BP is low, a PDA should be considered and echocardiography should be performed for early diagnosis and treatment.
The ductus arteriosus normally undergoes spontaneous closure within 24 to 48 hours after birth, in full-term infants. However, in 20% to 60% of the cases of premature infants, the ductus commonly remains open for many days after birth.1)2) Significant left-to-right shunting across a patent ductus arteriosus (PDA) in premature infants is associated with heart failure, intraventricular hemorrhage, necrotizing enterocolitis, and kidney injury as well as chronic lung disease, which leads to an increased morbidity and mortality.3-7) Therefore, diagnosis and treatment of a hemodynamically significant PDA in a timely manner is very important.
A PDA causes a decrease in the diastolic pressure resulting in a widened pulse pressure.8-10) Although this has been confirmed in older infants and children, it has not been confirmed in small preterm infants, who are often critically ill and have left-to-right shunting as a result of the PDA.4)11)
The effect of PDA closure on the pulse pressure and blood pressure (BP) in preterm infants has not been well documented. Some patients with a large PDA have been reported to have widened pulse pressures due to disproportionate reduction in the diastolic BP as compared to the systolic BP.12)13) However, others have reported that a hemodynamically significant PDA in very preterm infants is associated with reduction in both the systolic and diastolic BPs and that the pulse pressure is not significantly affected.9)11)14)
The goals of this retrospective study were to investigate the change in BP before and after medical treatment of a PDA with indomethacin; and to determine if the change in the pulse pressure could be used as a reliable clinical predictor of a hemodynamically significant PDA in preterm infants.
The records of all neonates less than 37 weeks gestational age (GA) and with a PDA treated with indomethacin were reviewed. There were a total of 3,546 neonates admitted to the Neonatal Intensive Care Units of the Chonnam National University Hospital from January 2005 to July 2009. There were 1,812 preterm infants and 343 of them had a PDA. Seventy-two infants, who had a hemodynamically significant PDA within 72 hours after birth, had undergone treatment with indomethacin and the ductus arteriosus subsequently closed after the treatment, were included in the study. The closure of PDA was confirmed by echocardiography and if the PDA remained open, these patients were excluded from this study. Each infant with a PDA was matched with an infant without a PDA. The matching criteria were: a similar GA (±1 week), birth weight (±100 g), ventilatory support, and severity of the respiratory distress syndrome. The following clinical data were recorded: GA, birth weight, gender, the day of diagnosis of the PDA, and the day on which indomethacin therapy was started. Neonates with severe combined diseases that could influence the BP were excluded from this study. The severe diseases such as major congenital malformations, congenital anomalies of the heart; except for a patent foramen ovale, renal or gastrointestinal abnormalities, persistent pulmonary hypertension, urinary output less than 1 mL/body weight per hour during the preceding 12 hours, recent bleeding within the last 48 hours, a periventricular or intraventricular hemorrhage more than grade 3, a platelet count less than 50,000/mm3, sepsis, and a surgical closure of the PDA, were excluded from this study.
BP was measured either directly using an indwelling umbilical arterial catheter (UAC) or a radial arterial type of monitoring with General Electric DASH 3000 monitor (General Electric Systems, Milwaukee, USA), General Electric DASH 4000 monitor (General Electric Systems, Milwaukee, USA), Intellivue MP70 (Philips Medical Systems, Suresnes, France) or indirectly using the oscillometric monitoring with General Electric DASH 3000 monitor (General Electric Systems, Milwaukee, USA), General Electric DASH 4000 monitor (General Electric Systems, Milwaukee, USA), Agilent M1205A monitor (Agilent technologies Co., Boeglingen, Germany), Critikon Neonatal Cuff (General Electric Systems, Juarez, Mexico).15) If direct measurement was available, the BP was recorded using it and if not, oscillometric measurement was exclusively used. If the UAC or radial artery catheter had been removed before the infant was 1 week old, oscillometric measurements were used. The pulse pressure was computed as the systolic BP minus the diastolic BP. From the recorded BP taken at every 3 hours, the daily mean systolic, diastolic, and pulse pressure measurements for each infant were calculated from 24 hours before the first dose of indomethacin upto seven days after the first dose of indomethacin. The BP in the control group was recorded in the same manner. If one of the patients in the PDA group received indomethacin on the fourth day after birth, the BP of a control with a similar GA (±1 week) and BW (±100 g), from the day before the initiation of indomethacin upto seven days after indomethacin treatment, from the the third day to the eighth day, were included in the analysis. BP support was provided whenever the mean arterial pressure (in torrs) was lower than the GA (in weeks), as suggested by Lee et al.16) The protocol in our institution is to give fluid boluses (NaCl 0.9%) of 10 mL/kg intravenously in cases with hypotension, followed by inotropes if the fluid boluses failed to correct the hypotension. For the purpose of this study, infants which received fluid boluses or inotropes during the first 48 hours of life, were not excluded from the study.
The diagnosis of PDA and the decision to treat were made on the basis of clinical criteria with echocardiographic (Acuson 128XP/10 color flow ultrasound system, Simens Medical Solutions, Malvern, Pennsylvania, USA; Agilent SONOS 5500, Philips Medical Systems, Andover, Massachusetts, USA; iE33 ultrasound system, Philips Medical Systems, Andover, Massachusetts, USA) confirmatory findings. The definition of a hemodynamically significant PDA was based on the previously established criteria and was defined by the presence of at least two of the following three parameters: a left atrium/aorta ratio of more than 1.4 : 1, a left ventricle/aorta ratio of more than 2.1 : 1, and the narrowest ductal diameter of more than 1.5 mm.17)
Each infant received three doses of i.v. indomethacin (Lyometacen; Chiesi Farmaceutici, Parma, Italy), 0.2 mg/kg at 12 hours intervals followed by two doses of 0.1 mg/kg each after 24 and 48 hours. Surgical ligation of the ductus was performed, when the ductus did not close after two or three courses of indomethacin treatment or when a pharmacological treatment was contraindicated (n=16). Before administering the next dose of indomethacin, echocardiography was performed and if the PDA had closed, no additional indomethacin was given.
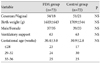
The results were analyzed in two different subgroups according to the birth weight: less than 1,500 g (n=67) and more than 1,500 g (n=77) and in two different subgroups according to the GA: less than 30 weeks (n=58) and more than 30 weeks (n=86). In each of the two subgroups, the mean GA and BW did not differ significantly between the PDA group and the control group (Table 1 and 2).
Results were expressed as the mean±standard deviation and statistically significant differences were set at p<0.05. Statistical Package for the Social Sciences for Windows (version 18.0) was used for analyzing the data. The differences in systolic BP, diastolic BP and pulse pressure were evaluated by an independent samples t-test and paired t-test.
Retrospective data were collected on the premature infants which met the inclusion criteria. Seventy-two preterm infants with a hemodynamically significant PDA and the same number of controls were analyzed. The mean GA, birth weight, mode of delivery, and sex were comparable between the PDA group and the control group (Table 3).
The mean systolic (55.1±6.0 mmHg) and diastolic BPs (31.4±6.2 mmHg) were significantly lower in the PDA group than in the control group (systolic BP of 58.0±6.0 mmHg, diastolic BP of 34.7±6.0 mmHg) before indomethacin treatment (p=0.006, p=0.002 respectively) (Fig. 1).
The mean systolic and diastolic BPs increased significantly and steadily in the PDA group during the seven days after indomethacin treatment was started. In the control group, the mean systolic BP increased steadily and the diastolic BP increased by the third day of BP measurement. There were significant differences in the systolic and diastolic BPs between the two groups. The systolic BPs between the PDA group and the control group respectively were as follows: On the first day 54.0±5.1 vs. 59.8±6.2 mmHg (p<0.001); on the second day: 57.5±5.6 vs. 62.2±5.8 mmHg (p=0.005), on the third day: 58.8±5.5 vs. 61.0±4.6 mmHg (p=0.014). The diastolic BPs between the PDA group and the control group respectively were as follows: on the first day: 30.9±4.7 vs. 36.3±4.7 mmHg (p<0.001); on the second day: 33.8±6.0 vs. 38.3±5.2 mmHg (p=0.001); on the third day: 35.6±5.9 vs. 37.7±5.7 mmHg (p=0.009). The infants with a PDA had lower mean systolic and diastolic BPs than the controls from the day before indomethacin treatment was started upto the third day after indomethacin treatment. The pulse pressures increased slightly after four days of indomethacin treatment in the two study groups, but were not significantly different at any given time between the PDA group and the control group (Fig. 1).
During the study period, the average mean systolic and diastolic BPs increased in the infants with a birth weight more than 1,500 g. The diastolic BPs were lower in the PDA group than in the control group but the differences were small and were not statistically significant. There were no significant differences in the pulse pressures between the two groups (Fig. 2). The systolic and diastolic BPs increased during the study period as compared to the BP on the day of the diagnosis in the infants with a birth weight more than 1,500 g; however, there was no statistically significant difference between the two groups (Fig. 2).
The mean systolic BP increased daily in the infants with a birth weight less than 1,500 g. However, the diastolic BP increased from the day before indomethacin treatment was started upto two days after indomethacin treatment in the infants with a birth weight less than 1,500 g. Systolic and diastolic BPs were significantly lower in the PDA group than in the control group during the same period. There were no significant differences in the pulse pressures between the two groups (Fig. 3).
The systolic and diastolic BPs increased during the study period in the infants with a GA of more than 30 weeks as compared to the BP on the day of diagnosis. However, there were no statistically significant differences between the two study groups. The diastolic BP was lower in the PDA group than in the control group; however, the difference was not statistically significant. In addition, there were no significant differences in the pulse pressures between the two groups (Fig. 4).
The mean systolic and diastolic BPs in the PDA group increased daily from the day before indomethacin treatment up-to two days after indomethacin treatment and were significantly lower as compared to the control group from the day before indomethacin treatment upto two days after indomethacin treatment. However, there were no significant differences in the pulse pressures between the two groups (Fig. 5).
The classical physical signs of a PDA are a heart murmur, tachycardia, and wide pulse pressures presenting as bounding pulses, a hyperactive precordium, and hepatomegaly. Chest radiographs show pulmonary plethora, cardiomegaly and a wide angle between the left and right main bronchi due to left atrial dilatation. However, several studies on these clinical signs have shown a sensitivity that ranges from 37%18) to 72%19) with little added to the clinical findings on radiography.20) Clearly, echocardiography is the most accurate method for establishing the diagnosis and assessing the closure of a PDA; however, practically it is difficult for many neonatal units to have immediate access to echocardiography. In the NICU, BP is evaluated regularly in all the preterm infants. This study was performed to evaluate the change in BP before and after the treatment of a PDA and to determine whether the pulse pressure BP is a useful clinical factor in the prediction and treatment of a PDA.
The results of this study show that in cases where medical treatment is successful, there is a gradual increase in the systolic and diastolic BPs after indomethacin treatment. A proportionate increase in both the systolic and diastolic BPs was seen, which means that there was no change in the pulse pressure. Therefore, if the systolic and diastolic BPs gradually increased after indomethacin treatment, PDA closure can be expected. Infants with a PDA had a significantly lower mean systolic and diastolic BP as compared to the control infants. There were no significant differences in the pulse pressures between the two groups and both the systolic and diastolic BPs promptly returned to control values four days after treatment with indomethacin.
Prior studies have shown similar results. Ratner et al.14) reported that the systolic and diastolic BPs decreased at the time of diagnosis of the PDA; also there were no significant differences in the pulse pressure. They suggested that the diastolic BPs were a more sensitive indicator of significant ductal shunting. However, the sample size in their study was small, including only 17 infants with a PDA and in these cases the PDA was surgically repaired.
Evans and Moor Craft4) reported that a hemodynamically significant PDA in very preterm infants during the first week of life was associated with a reduction in both the systolic and diastolic BPs and the pulse pressure was not different from that in the infants without a PDA. The most dramatic reductions in BP were among the infants less than 1,000 g; in the infants between 1,000-1,500 g, the BP was not significantly different between the infants with and without a hemodynamically significant PDA. However, in this study the change in the BP after treatment was not analyzed.
In other studies, Evans Iyer11) found an increase in BP following PDA closure with inconsistent changes in the pulse pressure. Where medical treatment is successful, there is a gradual and significant increase in all BP parameters over three days after the first dose of indomethacin, with inconsistent changes in the pulse pressure. They investigated the BP only in the PDA group and did not compare their findings to the infants without a PDA. It is well known that the BP gradually increases after birth in preterm infants.21) It was difficult to determine in their study whether the increase in BP after medical treatment was due to normal physiological changes or due to changes caused by the closure of the PDA. Therefore, to overcome this limitation, the BP in the PDA group was compared to a control group matched for GA and BW. The results showed a significant difference in the systolic and diastolic BPs between the two study groups before and after treatment of the PDA.
Lubetzky et al.9) found that PDA closure was associated with a non-significant change in the pulse pressure. However, they studied preterm infants that were diagnosed with a PDA within the first 24 hours of life and reported the BP only two times, i.e., pre and post treatment.
This study included 72 neonates with a PDA, medically treated with indomethacin and 72 neonatal controls without a PDA. For the low birth weight infants less than 1,500 g or with a GA of less than 30 weeks, increase in the systolic and diastolic BPs were more significant when the PDA was hemodynamically significant.
In this study, infants with conditions that might have some influence on the BP such as intraventricular hemorrhage, necrotizing enterocolitis, and sepsis as well as those that received surfactant infusion or ventilatory support were excluded. Further studies including these factors, and evaluation of the usefulness of other clinical signs such as a heart murmur, pulse rate, and chest radiography, are needed.
In conclusion, a widened pulse pressure is not a useful clinical sign of a hemodynamically significant PDA in preterm infants. However, low systolic and diastolic BPs may be useful clinical signs of a hemodynamically significant PDA in preterm infants. If systolic and diastolic BPs are low, a PDA should be considered and early assessment with echocardiography should be performed for establishing the diagnosis and initiating the treatment of a PDA. The systolic and diastolic BPs gradually increased after treatment, and this was associated with PDA closure.
Figures and Tables
Fig. 1
Mean systolic blood pressure (top), mean diastolic blood pressure (middle) and pulse pressure (bottom) in the PDA group and the control group. The closed squares indicate the PDA group and the open squares indicate the control group. Error bars indicate the standard deviation. *p<0.05. PDA: patent ductus arteriosus.

Fig. 2
Mean systolic blood pressure (top), mean diastolic blood pressure (middle) and pulse pressure (bottom) in the infants with a birth weight more than 1,500 g. PDA: patent ductus arteriosus.
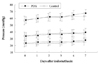
Fig. 3
Mean systolic blood pressure (top), mean diastolic blood pressure (middle) and pulse pressure (bottom) in the infants with a birth weight less than 1,500 g. PDA: patent ductus arteriosus. *p<0.05.

Fig. 4
Mean systolic blood pressure (top), mean diastolic blood pressure (middle) and pulse pressure (bottom) in the infants with a gestational age more than 30 weeks. PDA: patent ductus arteriosus.
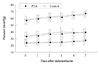
Fig. 5
Mean systolic blood pressure (top), mean diastolic blood pressure (middle) and pulse pressure (bottom) in the infants with a gestational age less than 30 weeks. PDA: patent ductus arteriosus. *p<0.05.

References
1. Wyllie J. Treatment of patent ductus arteriosus. Semin Neonatol. 2003. 8:425–432.
2. Knight DB. The treatment of patent ductus arteriosus in preterm infants. A review and overview of randomized trials. Semin Neonatol. 2001. 6:63–73.
3. Rakza T, Magnenant E, Klosowski S, Tourneux P, Bachiri A, Storme L. Early hemodynamic consequences of patent ductus arteriosus in preterm infants with intra-uterine growth restriction. J Pediatr. 2007. 151:624–628.
4. Evans N, Moor Craft J. Effect of patency of the ductus arteriosus on blood pressure in very preterm infants. Arch Dis Child. 1992. 67:1169–1173.
5. Kluckow M, Evans N. Ductal shunting, high pulmonary blood flow, and pulmonary hemorrhage. J Pediatr. 2000. 137:68–72.
6. Kim HS, Lee K. A study on patent ductus arteriosus in premature infants. Korean Circ J. 1985. 15:483–496.
7. Shimada S, Kasai T, Konishi M, Fujiwara T. Effects of patent ductus arteriosus on left ventricular output and organ blood flows in preterm infants with respiratory distress syndrome treated with surfactant. J Pediatr. 1994. 125:270–277.
8. Bernstein D. Behrman RE, Kliegman RM, Jenson HB, editors. A cyanotic congenital heart diseases: the left-to right shunt lesions. Nelson Textbook of Pediatrics. 2007. 18th ed. Philadelphia: W.B. Saunders Company;1891–1893.
9. Lubetzky R, Mendel D, Mimouni FB, et al. Indomethacin induced early patent ductus arteriosus closure cannot be predicted by a decrease in pulse pressure. Am J Perinatol. 2004. 21:257–261.
10. Hoffman TM, Welty SE. Emmanouilides GC, Riemenschneider TA, editors. Patent ductus arteriosus. Moss and Adams' Heart Disease in Infants, Children, and Adolescents. 2008. 7th ed. Philadelphia: Williams & Wilkins;440–441.
11. Evans N, Iyer P. Change in blood pressure after treatment of patent ductus arteriosus with indomethacin. Arch Dis Child. 1993. 68:584–587.
12. Perlman JM, Hill A, Volpe JJ. The effect of patent ductus arteriosus on flow velocity in the anterior cerebral arteries: ductal steal in the premature newborn infant. J Pediatr. 1981. 99:767–771.
13. Rudolph AM, Scarpelli EM, Golinto RJ, Gootman NL. Hemodynamic basis for clinical manifestations of patent ductus arteriosus. Am Heart J. 1964. 68:447–458.
14. Ratner I, Perelmuter B, Toews W, Whitfield J. Association of low systolic and diastolic blood pressure with significant patent ductus arteriosus in very low birth weight infants. Crit Care Med. 1985. 13:497–500.
15. Choi SK. Problems in measuring blood pressure. Korean Circ J. 1997. 27:485–487.
16. Lee J, Rajadurai VS, Tan KW. Blood pressure standards for low birth weight infants during the first day of life. Arch Dis Child Fetal Neonatal Ed. 1999. 81:F168–F170.
17. Skinner J. Diagnosis of patent ductus arteriosus. Semin Neonatol. 2001. 6:49–61.
18. Hirsimaki H, Kero P, Wanne O. Doppler ultrasound and clinical evaluation in detection and grading of patent ductus arteriosus in neonates. Crit Care Med. 1990. 18:490–493.
19. Valdes-Cruz LM, Dudell GG. Specificity and accuracy of echocardiographic diagnosis and clinical criteria for diagnosis of patent ductus arteriosus in fluid-restricted infants. J Pediatr. 1981. 98:298–305.
20. Davis P, Turner-Gomes S, Cunningham K, Way C, Roberts R, Schmidt B. Precision and accuracy of clinical and radiological signs in premature infants at risk of patent ductus arteriosus. Arch Pediatr Adolesc Med. 1995. 149:1136–1141.
21. Hegyi T, Anwar M, Carbone MT, et al. Blood pressure ranges in premature infants: part II. the first week of life. Pediatrics. 1996. 97:336–342.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download