Abstract
Background and Objectives
Patients without previous history of cardiac disease can be regarded as low-risk when undergoing major non-cardiac surgery. The aim of this study was to examine whether preoperative B-type natriuretic peptide (BNP) level predicted postoperative cardiac events in these patients.
Subjects and Methods
Preoperative BNP level was measured in 163 patients whose risk was considered low according to the Revised Cardiac Risk Index. Postoperative cardiac events, including death during hospitalization, myocardial injury, arrhythmia, cerebrovascular accidents and congestive heart failure were assessed.
Perioperative mortality and morbidity associated with major non-cardiac surgery are strongly related to cardiac complications, such as myocardial infarction, stroke, unstable angina, pulmonary edema and serious arrhythmia. Many studies have identified clinical predictors of adverse cardiac events, including age, type of surgery, diabetes, congestive heart failure and previous history of angina or myocardial infarction.1-3) Poor left ventricular (LV) systolic dysfunction is also a known predictor of perioperative cardiac events.4)
If a cardiology consultation is requested for patients with known cardiac disease, intensive cardiac assessment may be performed according to the guidelines on perioperative cardiovascular evaluation.5) However, the evaluation steps or tools for risk stratification in patients with other risk factors, such as old age, diabetes and scheduled major non-cardiac surgery, which carries a 1-5% risk of cardiac events, have not been comprehensively studied. Moreover, symptoms of heart disease may be absent or blunted, especially in elderly or diabetic patients, and clinical evaluation alone may not be sufficient to stratify risks. Biomarkers readily available for testing, may assist with risk stratification and guide surgeons and patients in their evaluation surgical risks.
B-type natriuretic peptide (BNP) levels correlate with prognosis in patients with cardiac disease6-9) and may be useful in risk stratification of patients undergoing non-cardiac surgery.10-14) Left ventricular systolic dysfunction is correlated with elevated BNP levels, and is a known predictor of perioperative cardiac events.
The purpose of this study was to assess whether BNP levels predicted perioperative cardiac events in patients who had no previous history of cardiac diseases, such as congestive heart failure, angina, or myocardial infarction.
The study was a prospective, single-center, observational cohort study of consecutive patients undergoing major scheduled non-cardiac surgery. Major non-cardiac surgery was defined as major gastrointestinal surgery (laparotomy, thoracolaparotomy), major orthopedic surgery and other major open surgery (gynecologic and urologic surgery). The risk of cardiac events was calculated using the Lee's Cardiac Risk Index, which is a standardized, validated clinical scoring system based on the presence of 6 clinical variables: high-risk surgery, history of ischemic heart disease, congestive heart failure, cerebrovascular disease, insulin therapy for diabetes mellitus and preoperative serum creatinine >2mg/dL.15) Patients with a risk index score of 0 or 1 have complication rates of 0.4-0.9%. Such patients were regarded as low-risk. Exclusion criteria included previous history of congestive heart failure, angina, or myocardial infarction, LV ejection fraction less than 50% and creatinine level ≥2.0 mg/dL.
Preoperative data collection included a 12-lead electrocardiography (ECG) recording, echocardiography, clinical characteristics, medical and surgical history, preoperative medications and renal and hepatic functions. Preoperative blood samples were also obtained for plasma BNP levels. The mean time of venous sampling before surgery was 3±8 days. All patients underwent standard 2-dimensional and doppler echocardiographic examination with assessment of ventricular systolic and diastolic function.
The left atrial (LA) volume was calculated using the formula for an ellipsoid:
LA volume (mL)=Π/6 (D1×D2×D3)
where D1, D2, and D3 are the parasternal long axis, superoinferior, and medio-lateral measurements, respectively, of the LA at end-systole. The LA volume index was calculated as LA volume/body surface area. LV mass was calculated using guidelines recommended by the American Society of Echocardiography, and left ventricular mass index (LVMI) was calculated as LV msss/body surface area.
Postoperative data collection included a 12-lead ECG recording, chest radiograph, symptoms suggestive of myocardial ischemia or congestive heart failure after surgery and death during hospitalization.
The composite end-point was death, postoperative myocardial injury {cardiac troponin I (cTnI) >0.32 ng/mL-1, without preoperative cTnI elevation}, ECG evidence of acute myocardial ischemia or arrhythmia, cerebrovascular accident and congestive heart failure. ECG evidence of ischemia was defined as the development of new, postoperative T-wave inversion 2 mm and ST segment deviation 2 mm in at least two contiguous chest leads, or 1 mm in at least two contiguous limb leads. Arrhythmia was defined as a new, sustained, abnormal cardiac rhythm. Congestive heart failure was diagnosed by physical examination and chest radiograph.
Plasma BNP was measured using the Bayer ADVIA Centaur™ immunoassay (Bayer Healthcare LLC, Diagnostic Division, Leverkusen, Germany) before an operation.
Continuous data with a normal distribution are expressed as mean±standard deviation, and were compared using the Student's t-test. Categorical data are presented as percentage frequencies, and differences between proportions were compared using the chi-square test with Yates' correction. Receiver-operating characteristic (ROC) curve analysis was performed to calculate sensitivity, specificity and the area under the curve to select a cut-off value to predict perioperative cardiovascular events. Multivariate analysis was conducted to determine factors related to perioperative cardiovascular complications. The variables were selected according to significant univariate analysis, and odds ratios were given with 95% confidence intervals (CI). For continuous variables, the median value was used as a cut-off point to determine perioperative adverse events.
For all tests, a p less than 0.05 (2-tailed) was considered statistically significant. All analyses were performed using Statistical Package for the Social Sciences (SPSS) version 13.0 statistical software (SPSS, Inc., Chicago, IL, USA).
One hundred sixty-three patients met the inclusion criteria for the study. Table 1 describes the clinical characteristics of the study population. The mean patient age was 71 years old. The age of patients with cardiac events was significantly higher than that of patients without cardiac events (77±8 vs. 70±11, p=0.047).
Postoperative cardiac events occurred in 8 patients (4.9%): 5 congestive heart failures, 1 myocardial injury, 2 unstable anginas and 2 strokes. There was no cardiac death.
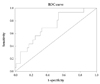
The mean preoperative BNP level was 61.5±77.2 pg/mL. Preoperative BNP levels were significantly higher among patients who experienced postoperative cardiac events (Table 1) (Fig. 1). Preoperative BNP predicted perioperative cardiovascular events with an area under the receiver operator characteristic curve of 0.76 (95% CI 0.63-0.89, p=0.014). The optimal cut-off point derived from this curve was 64.5 pg/mL. This had a sensitivity of 75% and a specificity of 75% (Fig. 2).
The mean LV ejection fraction was 61.5±6.7%. LA volume index was significantly higher in patients who experienced postoperative cardiac evenst than in patients who did not (33.3±23.0 vs. 22.1±7.1, p<0.0001) (Table 2).
From univariate analysis, the presence of atrial fibrillation and LA volume index were significant predictors of postoperative cardiac events. However, when preoperative BNP levels were included, the presence of atrial fibrillation and LA volume index were no longer statistically significant. BNP greater than 64.5 pg/mL did not reach statistical significance, but there was a trend for BNP to provide independent prognostic information (p=0.086).
Patients with no previous history of cardiac disease and normal LV systolic function can be regarded as low-risk for developing cardiac events during major non-cardiac surgery. In our study, however, a risk did exist (4.9%), although life-threatening cardiac events did not happen. Preoperative BNP levels were higher in patients who suffered postoperative cardiac events, which suggests that preoperative BNP level may provide prognostic information in patients no cardiac history.
Efforts to identify patients at increased cardiac risks when undergoing non-cardiac surgery have led to the development of a variety of scoring systems.1-3) In a multi-center study comparing several of these risk stratification indices, the areas under the ROC curves ranged from 0.60 to 0.64.16) Lee et al.15) indicated that an area under the ROC curve of 0.76 for the ability of the Revised Cardiac Risk Index to identify patients who experience a postoperative cardiac event. Nevertheless, our data suggest that BNP has a useful role in risk prediction in this setting. We recognize, however, that the CI around the area under the ROC curve value of 0.63 was wide (0.59-0.83), and larger studies are required to provide more precise estimates.
There are several reasons to support how BNP may predict cardiac events in this setting. BNP level is known to have predictive ability for cardiac events, such as heart failure, atrial fibrillation, stroke and coronary heart disease. Although a concentration of 100 pg/mL is widely accepted as the threshold to diagnose heart failure, excess risk exists at BNP levels well below this threshold.7)17) We hypothesize that some patients scheduled for major surgery may have subclinical diastolic heart failure or ischemic heart disease. As such, preoperative BNP levels may reflect their underlying cardiovascular status. In our study, the BNP level was lower than that reported in other studies, probably because all patients had an ejection fraction greater than 50%.10)12)
LA enlargement is traditionally considered a risk factor for atrial fibrillation, stroke and death in various clinical settings.18-21) Furthermore, it may be an early sign of hypertensive heart disease in patients with no other discernible cause of LA enlargement.22)23) Approximately 50% of our patients were hypertensive, so LA volume index may reflect their underlying hypertensive heart disease status. However, the clinical significance of this finding remains to be elucidated in future studies.
This was a small study with limited statistical power. The lack of blinding substantially confounded the results because clinicians used the results of BNP measurements to manage patients. As such, treatment bias was unavoidable. Surgical complications or incidences related to surgical procedures can influence the occurrence of serious cardiac events. However, these were not taken into consideration. Finally, our cohort was heterogeneous. For instance, it included patients undergoing major abdominal surgery and hip surgery. Nevertheless, the predictive value of BNP concentration must demonstrate sensitivity and specificity in such diverse clinical situations to prove its clinical usefulness.
Figures and Tables
Fig. 1
A comparison of preoperative BNP levels in patients who experienced a postoperative cardiac event (Y) with those who did not (N). Central lines represent medians, boxes represent 25th and 75th percentiles and whiskers represent ranges. BNP: B-type natriuretic peptide.

Fig. 2
Receiver operator characteristic curve for preoperative B-type natriuretic peptide levels predicting an early postoperative cardiac event. Area under the curve=0.76 (95% confidence interval=0.63-0.89, p=0.014). ROC: receiver-operating characteristic.
References
1. Goldman L, Caldera DL, Nussbaum SR, et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med. 1977. 297:845–850.
2. Detsky AS, Abrams HB, Forbath N, Scott JG, Hilliard JR. Cardiac assessment for patients undergoing noncardiac surgery: a multifactorial clinical risk index. Arch Intern Med. 1986. 146:2131–2134.
3. Goldman L. Multifactorial index of cardiac risk in noncardiac surgery: ten-year status report. J Cardiothorac Anesth. 1987. 1:237–244.
4. Halm EA, Browner WS, Tubau JF, Tateo IM, Mangano DT. Echocardiography for assessing cardiac risk in patients having noncardiac surgery: study of perioperative ischemia research group. Ann Intern Med. 1996. 125:433–441.
5. Eagle KA, Berger PB, Calkins H, et al. ACC/AHA guideline update for perioperative cardiovascular evaluation for noncardiac surgery: executive summary a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (committee to update the 1996 guidelines on perioperative cardiovascular evaluation for noncardiac surgery). Circulation. 2002. 105:1257–1267.
6. de Lemos JA, Morrow DA, Bentley JH, et al. The prognostic value of B-type natriuretic peptide in patients with acute coronary syndromes. N Engl J Med. 2001. 345:1014–1021.
7. Wang TJ, Larson MG, Levy D, et al. Plasma natriuretic peptide levels and the risk of cardiovascular events and death. N Engl J Med. 2004. 350:655–663.
8. Choe HM, Yoo BS, Ryu HY, et al. The early changing pattern of the B-type natriuretic peptide concentration and its significance as a prognostic marker after acute myocardial infarction. Korean Circ J. 2006. 36:526–534.
9. Chung IH, Yoo BS, Ryu HY, et al. The relationship between the early follow-up BNP level and congestive status or prognosis in acute heart failure. Korean Circ J. 2006. 36:200–207.
10. Dernellis J, Panaretou M. Assessment of cardiac risk before non-cardiac surgery: brain natriuretic peptide in 1590 patients. Heart. 2006. 92:1645–1650.
11. Feringa HH, Bax JJ, Elhendy A, et al. Association of plasma N-terminal pro-B-type natriuretic peptide with postoperative cardiac events in patients undergoing surgery for abdominal aortic aneurysm or leg bypass. Am J Cardiol. 2006. 98:111–115.
12. Cuthbertson BH, Amiri AR, Croal BL, et al. Utility of B-type natriuretic peptide in predicting perioperative cardiac events in patients undergoing major non-cardiac surgery. Br J Anaesth. 2007. 99:170–176.
13. Cuthbertson BH, Card G, Croal BL, McNeilly J, Hillis GS. The utility of B-type natriuretic peptide in predicting postoperative cardiac events and mortality in patients undergoing major emergency non-cardiac surgery. Anaesthesia. 2007. 62:875–881.
14. Gibson SC, Payne CJ, Byrne DS, Berry C, Dargie HJ, Kingsmore DB. B-type natriuretic peptide predicts cardiac morbidity and mortality after major surgery. Br J Surg. 2007. 94:903–909.
15. Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999. 100:1043–1049.
16. Gilbert K, Larocque BJ, Patrick LT. Prospective evaluation of cardiac risk indices for patients undergoing noncardiac surgery. Ann Intern Med. 2000. 133:356–359.
17. Daniels LB, Maisel AS. Natriuretic peptides. J Am Coll Cardiol. 2007. 50:2357–2368.
18. Vaziri SM, Larson MG, Benjamin EJ, Levy D. Echocardiographic predictors of nonrheumatic atrial fibrillation: the Framingham Heart Study. Circulation. 1994. 89:724–730.
19. Benjamin EJ, D'Agostino RB, Belanger AJ, Wolf PA, Levy D. Left atrial size and the risk of stroke and death: the Framingham Heart Study. Circulation. 1995. 92:835–841.
20. Laukkanen JA, Kurl S, Eranen J, Huttunen M, Salonen JT. Left atrium size and the risk of cardiovascular death in middle-aged men. Arch Intern Med. 2005. 165:1788–1793.
21. Bayes-Genis A, Vazquez R, Puig T, et al. Left atrial enlargement and NT-proBNP as predictors of sudden cardiac death in patients with heart failure. Eur J Heart Fail. 2007. 9:802–807.
22. Miller JT, O'Rourke RA, Crawford MH. Left atrial enlargement: an early sign of hypertensive heart disease. Am Heart J. 1988. 116:1048–1051.
23. Tsioufis C, Stougiannos P, Taxiarchou E, et al. The interplay between haemodynamic load, brain natriuretic peptide and left atrial size in the early stages of essential hypertension. J Hypertens. 2006. 24:965–972.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download