Abstract
Background and Objectives
Plaque composition rather than degree of luminal narrowing may be predictive of future coronary events in high risk patients. The purpose of this study was to compare degree of plaque burden and composition with multislice computed tomography (MSCT) angiography between diabetic and non-diabetic patients.
Subjects and Methods
A total of 452 consecutive MSCT angiography examinations were performed between July 2007 and June 2009. Of these, the patients who underwent invasive coronary angiography were evaluated for the presence and type of atherosclerotic plaque and severity of luminal narrowing.
Results
Ninety two (46 in the diabetic group and 46 in the non-diabetic group) patients underwent both MSCT angiography and invasive coronary angiography. Among them, 30 patients (65.2%) in the diabetic group and 26 patients (56.5%) in the non-diabetic group had significant coronary narrowing on MSCT angiography. Sixteen patients (34.8%) in the diabetic group and 15 patients (32.6%) in non-diabetic group underwent coronary angioplasty and stenting. Forty-two patients (93.3%) in the diabetic group and 39 patients (88.6%) in the non-diabetic group had multiple types of coronary plaque (p=0.485). MSCT angiography was similar to conventional coronary angiography in its ability to predict significant coronary artery disease in that the area under the curve was 0.88 (95% confidence interval, 0.81 to 0.95). Diabetic patients had more mixed plaque compared with non-diabetic patients.
Patients with diabetes have a significant risk for atherosclerotic vascular disease, and aggressive management of risk factors is recommended in these patients, irrespective of symptoms or known coronary artery disease (CAD). Therefore, the role of coronary imaging in diabetic patients is not only to prove the presence of coronary narrowing but to detect those patients with a higher risk in whom further testing may be warranted in order to identify those with significant inducible myocardial ischemia.
Multislice computed tomography (MSCT) angiography can accurately visualize the coronary arteries and permits detection of significant coronary artery stenosis when compared with conventional coronary angiography.1-3) Previous reports on detection and characterization coronary atherosclerotic plaque has revealed that MSCT angiography enables the measurement of the degree of stenosis and well correlated with measurement by intravascular ultrasound (IVUS)4)5) and conventional coronary angiography.6)
Although IVUS is the gold standard for characterizing morphology plaque or degree of stenosis in patients undergoing coronary angiography, noninvasive detection and characterization of coronary plaque would be an attractive alternative modality. Noninvasive evaluation of coronary atherosclerotic plaques would improve risk stratification of both symptomatic and asymptomatic patients and also of high risk diabetic patients.7) The purpose of this study was to compare the coronary plaque burden and composition in diabetic and non-diabetic patients with angina pectoris undergoing both MSCT angiography with conventional coronary angiography and evaluate any differences that might explain the poorer clinical outcomes in diabetic patients with CAD.
A total 452 consecutive MSCT angiography examinations were performed between July 2007 and June 2009. The study group consisted of the patients who underwent both MSCT angiography and conventional coronary angiography. Referral for coronary angiography was based on the presence of symptoms, abnormal or inconclusive previous treadmill exercise electrocardiography (ECG), and/or nuclear testing. Patients in sinus rhythm without contraindications to MSCT angiography were included. Exclusion criteria were (supra-) ventricular arrhythmia, renal insufficiency, known allergy to contrast media and pregnancy. An institutional review board approved the study and all participants provided written informed consent.
MSCT angiography data were acquired with a 64 multi-detector CT scanner (Toshiba Medical Systems, Japan). According to a previously published protocol,8) images were acquired with 16×0.75 mm slice collimation, a gantry rotation time of 420 ms, table feed of 2.8 mm/rotation, tube energy of 120 kV, and an effective tube current of 500 mAs. Eighty milliliters of contrast agent (Iodhexodol 320 g/cm3, Visipaque, GE-Healthcare Amersham, Piscataway, NJ, USA) were injected intravenously at a rate of 4 mL/s, followed by a 30 mL saline chaser. All patients with a heart rate > 65 beats/min received 5 mg metoprolol intravenously before the MSCT scan.
Overlapping trans-axial images were reconstructed using a medium sharp convolution kernel (B35f) with an image matrix of 512×512 pixels, slice thickness of 1 mm, and an increment of 0.5 mm using an ECG-gated half-scan algorithm with a resulting temporal resolution of 210 ms in the center of rotation. Image reconstruction was retrospectively gated to the ECG. The position of the reconstruction window within the cardiac cycle was individually optimized to minimize motion artifacts.
Data were evaluated on a remote workstation using dedicated software (Vitrea, Vital Images, USA). For each patient, the entire coronary arterial tree was inspected for the presence of coronary plaques. Observers graded image quality of coronary segments as interpretable or not interpretable. Only patients with interpretable image quality in all coronary segments with lesions >50% were included in the analysis. To evaluate lesions, original axial images, multi-planar reconstructions perpendicular to the vessel centerline and cross-sectional reconstructions (1-mm thickness) were rendered at the site of maximal lumen narrowing and at reference sites proximal and distal to the lesion. Segments with motion artifacts or poor contrast-to-noise ratio were excluded from the analysis and patients in whom all of the following segments (the left main, the proximal and middle segment of the left anterior descending artery and the right coronary artery and the proximal segment of the circumflex artery) could be assessed were included. Interpretable lesions identified on MSCT angiography subsequently were visually classified as non-calcified, mixed plaques, or calcified plaques. Examples of each type of lesion are provided in Fig. 1.
Coronary plaques were defined as structures >1 mm2 within the coronary artery whose density differed from that of the contrast-enhanced vessel lumen. Plaques were divided into calcified {density >130 Hounsfield Unit (HU) in native scans}, non-calcified, or mixed lesions (Fig. 1). Non-calcified lesions were identified on the basis of their lower density compared with the contrast-enhanced vessel lumen (density <130 HU) as described by Schroder et al.9) Mixed lesions were defined as a plaque area consisting of >50% of non-calcified plaque tissue.
To test differences in demographics and risk factors between diabetic and non-diabetic patients, we performed an unpaired t test (for continuous variables) or a chi-square test (for categorical variables). For assessment of the independent relationship of different plaques subtypes with diabetes mellitus, logistic regression analysis (plaque subtype as the dependent variable) was used. All statistical analyses were performed using Statistical Package for the Social Sciences (SPSS) software (version 15.0, SPSS Inc, Chicago, IL, USA). A p<0.05 was considered to indicate statistical significance.
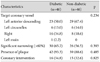
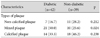
Of the 452 patients, 92 (46 in the diabetic group and 46 in the non-diabetic group) patients underwent both MSCT angiography and invasive coronary angiography. Demographic and clinical characteristics of the patients are summarized in Table 1. No significant differences in risk factors were present between the two groups. Patients with diabetes were more likely to be hypertensive compared with those without diabetes. Smoking history, hypercholesterolemia, previous history of percutaneous coronary intervention and coronary artery bypass graft surgery were not different between the two groups. Twenty-two (47.8%) patients in the diabetic group and 17 (37.0%) in the non-diabetic group had multi-vessel disease (p=0.291).
Fig. 2 shows a receiver-operating-characteristic curve describing the diagnostic performance of MSCT angiography to identify coronary stenosis of 60% or more in the culprit vessel. The area under the curve (AUC) was 0.88 {95% confidence interval (CI), 0.81 to 0.95}. The sensitivity and specificity for the quantitative analysis were 95% (95% CI, 92 to 96) and 71% (95% CI, 69 to 72), respectively, with positive and negative predictive value of 75% (95% CI, 71 to 78) and 97% (95% CI, 95 to 98).
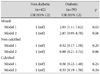
The characteristics of coronary stenosis according to diabetes status are presented in Table 2. The right coronary artery tended to be more frequently involved in diabetic patients, whereas left anterior descending artery involvement was more prevalent in non-diabetic patients. There was no statistically significant difference in the prevalence of significant coronary narrowing (>60%) between the two groups (65.2 vs. 56.5%, p=0.393). Atherosclerotic plaque was present in 42 (93.3%) diabetic patients and 39 (88.6%) non-diabetics, a difference which was not statistically significant. Coronary intervention was done in 16 (34.8%) diabetic patients and 15 (32.6%) non-diabetics. The remaining patients were treated conservatively with optimal medical treatment.
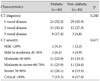
Coronary CT angiographic characteristics of the study population are shown in Table 3. More than half the patients in both groups had single vessel disease. Triple vessel disease was found in 8 (17.4%) patients with diabetes and 3 (6.8%) in patients without diabetes. Also, the severity of luminal narrowing of target vessels was not significantly different between the two groups (p=0.677). When assessed according to types of coronary plaque, patients with diabetes had a higher prevalence of mixed plaques compared with non-diabetic patients (50% vs. 25.6%, p=0.024), whereas the other kinds of plaque did not show such differences (non-calcified plaques: 16.7% vs. 28.2%, p=0.212, calcified plaques: 33.3% vs. 46.2%, p=0.238) (Table 4). Fig. 3 shows the composition of different kinds of plaque according to the presence of diabetes mellitus.
The results of multivariate logistic regression analysis are shown in Table 5. After adjustment for age and sex, diabetics were shown to be more likely to have mixed plaques {odds ratio (OR): 2.91, 95% CI 1.11-0.62, p=0.03}; whereas, after adjustment for age, sex, history of hypertension, smoking, and hypercholesterolemia, patients with diabetes showed a trend toward more mixed plaque but the difference was not statistically significant (OR: 2.87, 95% CI 0.95-8.70, p=0.062).
A major finding of this study was that MSCT angiography can accurately identify burden of atherosclerotic plaque and differences in its composition and that plaque features were closely related to the presence of diabetes (Fig. 3). The extent of coronary plaques was similar in diabetic and non-diabetic patients when assessed by MSCT angiography. The proportion of mixed plaques seen using MSCT angiography was larger in patients with diabetes when compared with patients without diabetes.
A similar finding was reported recently by Ibebuogu et al.10) showing that diabetic patients had a higher proportion of coronary segments with mixed plaques compared with non-diabetic patients (1.67±2.01 vs. 1.23±1.61, p=0.05) using MSCT angiography. In our study, a similar extent of coronary atherosclerotic narrowing was observed in diabetic patients on MSCT angiography and although statistically not significant, the presence of plaques was higher in diabetic patients. This finding is in line with a previous study11) exploring invasive coronary plaque characterization on gray-scale IVUS in 654 patients, of which 128 had diabetes. They reported a significantly larger plaque burden in diabetic patients. Increased plaque extent on MSCT angiography, as well as gray-scale IVUS, might explain a higher event rate in diabetic patients compared with non-diabetics.
Previous studies using MSCT angiography have suggested that coronary calcium content is associated with total plaque burden and therefore increases severity of luminal narrowing. Therefore, a high calcium score level was regarded as a surrogate marker for increased cardiovascular risk and events.12)13) However, it is unclear how well the presence and amount of calcium can predict coronary events in various patient populations with different cardiovascular risk factors, such as diabetes. In our study, diabetic patients had an increased number of mixed plaques compared with patients without diabetes. Differences in plaque composition may in part explain the increased risk of CAD and mortality in diabetic patients.14) Indeed, previous studies support the hypothesis that plaque composition, as well as stenosis severity, is predictive of future coronary events. As shown in Mann and Davies's study,15) lipid core size and minimal cap thickness have been known as major determinants of plaque vulnerability, while absolute plaque size and degree of coronary narrowing were not. So, vulnerable plaques may occur across the full spectrum of coronary disease, suggesting that relatively mild coronary lesions may contribute to coronary events.16)17)
IVUS is the gold standard for plaque detection and characterization and for the assessment of plaque progression in follow-up studies.18) It has the advantage of a higher spatial resolution but is invasive and limited due to its low penetration depth.19) Although current MSCT angiography technology is not as good when compared to IVUS in terms of spatial resolution, it allows non-invasive evaluation of the vessel wall.20) Additionally, a major advantage of non-invasive imaging modality is that it is less time consuming for both the patient and the operator. MSCT angiography also has fewer acute risks, such as coronary spasm related to IVUS catheterization, acute vessel closure, dissection and distal embolization.21)
A recent study using virtual histology IVUS demonstrated that mixed plaques were more highly associated with high risk features when compared with calcified or non-calcified plaques.22) Also, thin-cap fibroatheromas (TCFA) were more frequently present in mixed plaques and the increased amount of necrotic core was shown to be a feature of increased risk to plaque rupture.23) Nevertheless, the proportion of TCFAs was identical in diabetic and non-diabetic patients. Another study demonstrated that TCFA lesions were known to be more prevalent in patients with acute coronary syndromes than in patients with stable CAD.24) The higher proportion of mixed plaques in diabetic patients in our study can be regarded as having high risk lesions because vulnerable plaque presented with TCFA; less extensive calcification and high proportion of necrotic core tissue are frequently observed in mixed plaques on MSCT angiography. As previously mentioned, Pundziute et al.25) demonstrated that mixed plaques on MSCT angiography were related more with adverse cardiovascular events on one-year follow-up. Among the predictors of coronary cardiac events in that study, the number of segments with mixed plaques were one of the significant independent predictors (hazard ratio 1.6, 95% CI 1.2-2.0, p=0.0003). Therefore, the predominance of mixed plaques in symptomatic diabetic patients with CAD might explain the higher incidence of coronary events, including unstable acute coronary syndrome, and thus hospital admission.
On the contrary, in a recent study, 49% of plaques in diabetic patients were classified as completely calcified.26) This finding could be explained by a higher risk profile of the patients in the study when compared with the population of in the previous study. Further studies are necessary to better understand the mechanisms that lead to plaque instability and cardiovascular events in diabetic patients. Although earlier studies have shown that diabetics are more likely to have multi-vessel disease compared with non-diabetics,27) in our selected symptomatic patients, using a 60% stenosis cut-off did not show a significant difference between the two groups (47.8%, 37.0%, p=0.291).
There were several limitations in this study which should be considered. This study was a retrospective and non-randomized study. Also, there might be many confounding factors that could not be properly accounted for in the analysis and there were no available validated algorithms that allow quantification of plaque stenosis, volume, or composition. Because most patients who underwent MSCT angiography were asymptomatic and didn't have any obstructive findings on their examination, we selected only patients who had a high likelihood of CAD by performing both MSCT angiography and conventional angiography. As a consequence, many patients were excluded and selection bias may have affected the results. Thus, we should interpret the results very carefully and not extend them to most asymptomatic diabetic patients.
Another limitation of this study is the lack of IVUS as a gold standard for plaque characterization, although previous studies demonstrated a strong correlation between MSCT and IVUS examinations for assessing plaque characteristics, as well as for the measurement of the plaque volumes.22)28) Also, the prognostic value of MSCT angiography in diabetic and non-diabetic patients was not determined. Finally, the study population was small. Further studies should address whether certain plaque characteristics in diabetic patients may indeed be related to adverse outcomes.
In conclusion, MSCT angiography may be useful for the identification of CAD in diabetic and non-diabetic patients. There were significant differences in coronary atherosclerotic plaque burden and composition between diabetic and non-diabetic patients, with a higher proportion of mixed plaques, a more vulnerable form of atherosclerotic plaque, in diabetics. Furthermore, MSCT angiography may give accurate information about plaque characteristics according to different coronary risk factors, thereby identifying high risk features warranting a more intensive anti-atherosclerotic treatment.
Figures and Tables
Fig. 1
Example of different plaque types as visually assigned on the multislice computed tomography angiography. A: non-calcified plaque. B: mixed plaque. C: calcified plaque.

Fig. 2
Diagnostic performance of MSCT angiography. Receiver-operating-characteristic curve describing the diagnostic performance of MSCT angiography to identify coronary stenosis of 60% or more in culprit vessel. The area under the curve was 0.88 (95% confidence interval, 0.81 to 0.95). MSCT: multislice computed tomography.
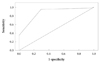
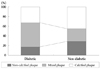
Fig. 3
Bar graph demonstrating the relative distribution of the different lesion types in diabetic and non-diabetic patients (p=0.035).
References
1. Achenbach S, Ulzheimer S, Baum U, et al. Noninvasive coronary angiography by retrospectively ECG-gated multi-slice spiral CT. Circulation. 2000. 102:2823–2828.
2. Hoffmann U, Moselewski F, Cury RC, et al. Predictive value of 16-slice multi-detector spiral computed tomography to detect significant obstructive coronary artery disease in patients at high risk for coronary artery disease: patient-versus segment-based analysis. Circulation. 2004. 110:2638–2643.
3. Oh HJ, Kwon K, Park SH, et al. CT coronary angiography using multidetector computed tomography in coronary artery disease : a comparative study to quantitative coronary angiography. Korean Circ J. 2004. 34:1167–1173.
4. Achenbach S, Moselewski F, Ropers D, et al. Detection of calcified and non-calcified coronary atherosclerotic plaque by contrast-enhanced, submillimeter multi-detector spiral computed tomography: a segment based comparison with intravascular ultrasound. Circulation. 2004. 109:14–17.
5. Kim SY, Kim KS, Lee YS, et al. Assessment of non-calcified coronary plaques using 64-slice computed tomography: comparison with intravascular ultrasound. Korean Circ J. 2009. 39:95–99.
6. Cury RC, Pomerantsev EV, Ferencik M, et al. Comparison of the degree of coronary stenoses by multi-detector computed tomography versus by quantitative coronary angiography. Am J Cardiol. 2005. 96:784–787.
7. Naghavi M, Libby P, Falk E, et al. From vulnerable plaque to vulnerable patient: a call for new definitions and risk assessment strategies: part I. Circulation. 2003. 108:1664–1672.
8. Hoffmann U, Moselewski F, Nieman K, et al. Noninvasive assessment of plaque morphology and composition in culprit and stable lesions in acute coronary syndrome and stable lesions in stable angina by multi-detector computed tomography. J Am Coll Cardiol. 2006. 47:1655–1662.
9. Schroeder S, Kopp AF, Baumbach A, et al. Noninvasive detection and evaluation of atherosclerotic coronary plaques with multi-slice computed tomography. J Am Coll Cardiol. 2001. 37:1430–1435.
10. Ibebuogu UN, Nasir K, Gopal A, et al. Comparison of atherosclerotic plaque burden and composition between diabetic and non diabetic patients by non invasive CT angiography. Int J Cardiovasc Imaging. 2009. 25:717–723.
11. Nicholls SJ, Tuzcu EM, Crowe T, et al. Relationship between cardiovascular risk factors and atherosclerotic disease burden measured by intravascular ultrasound. J Am Coll Cardiol. 2006. 47:1967–1975.
12. Wayhs R, Zelinger A, Raggi P. High coronary artery calcium scores pose an extremely elevated risk for hard events. J Am Coll Cardiol. 2002. 39:225–230.
13. Kim D, Choi SY, Choi EK, et al. Distribution of coronary artery calcification in an asymptomatic Korean population: association with risk factors of cardiovascular disease and metabolic syndrome. Korean Circ J. 2008. 38:29–35.
14. Herlitz J, Karlson BW, Lindqvist J, Sjolin M. Rate and mode of death during five years of follow-up among patients with acute chest pain with and without a history of diabetes mellitus. Diabet Med. 1998. 15:308–314.
15. Mann JM, Davies MJ. Vulnerable plaque: relation of characteristics to degree of stenosis in human coronary arteries. Circulation. 1996. 94:928–931.
16. Giroud D, Li JM, Urban P, Meier B, Rutishauer W. Relation of the site of acute myocardial infarction to the most severe coronary arterial stenosis at prior angiography. Am J Cardiol. 1992. 69:729–732.
17. Davies MJ, Thomas AC. Plaque fissuring: the cause of acute myocardial infarction, sudden ischaemic death, and crescendo angina. Br Heart J. 1985. 53:363–373.
18. Kopp AF. Angio-CT: heart and coronary arteries. Eur J Radiol. 2003. 45:Suppl 1. S32–S36.
19. Escolar E, Weigold G, Fuisz A, Weissman NJ. New imaging techniques for diagnosing coronary artery disease. CMAJ. 2006. 174:487–495.
20. Carrascosa PM, Capunay CM, Garcia-Merletti P, Carrascosa J, Garcia MF. Characterization of coronary atherosclerotic plaques by multi-detector computed tomography. Am J Cardiol. 2006. 97:598–602.
21. Hausmann D, Erbel R, Alibelli-Chemarin MJ, et al. The safety of intracoronary ultrasound: a multicenter survey of 2207 examinations. Circulation. 1995. 91:623–630.
22. Pundziute G, Schuijf JD, Jukema JW, et al. Head-to-head comparison of coronary plaque evaluation between multislice computed tomography and intravascular ultrasound radiofrequency data analysis. JACC Cardiovasc Interv. 2008. 1:176–182.
23. Kolodgie FD, Virmani R, Burke AP, et al. Pathologic assessment of the vulnerable human coronary plaque. Heart. 2004. 90:1385–1391.
24. Rodriguez-Granillo GA, Garcia-Garcia HM, McFadden EP, et al. In vivo intravascular ultrasound-derived thin-cap fibroatheroma detection using ultrasound radiofrequency data analysis. J Am Coll Cardiol. 2005. 46:2038–2042.
25. Pundziute G, Schuijf JD, Jukema JW, et al. Prognostic value of multislice computed tomography coronary angiography in patients with known or suspected coronary artery disease. J Am Coll Cardiol. 2007. 49:62–70.
26. Pundziute G, Schuijf JD, Jukema JW, et al. Noninvasive assessment of plaque characteristics with multi-slice computed tomography coronary angiography in symptomatic diabetic patients. Diabetes Care. 2007. 30:1113–1119.
27. Hambly RI, Sherman L, Mehta J, et al. Reappraisal of the role of the diabetic state in coronary artery disease. Chest. 1976. 70:251–257.
28. Springer I, Dewey M. Comparison of multislice computed tomography with intravascular ultrasound for detection and characterization of coronary artery plaques: a systematic review. Eur J Radiol. 2009. 71:275–282.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download