Abstract
Background and Objectives
There are limited data examining triggering activities and circadian distribution at the onset of acute aortic dissection (AAD) in the context of diagnostic and anatomical classification. The aim of this study was to further investigate this relationship between triggering activities and circadian distribution at the onset of AAD according to diagnostic and anatomic classification.
Subjects and Methods
A total of 166 patients with AAD admitted to Kyungpook National University Hospital between July 2001 and June 2009 were included. To assess the influence of diagnostic and anatomical classification, we categorized the patients into intramural hematoma (IMH) group (n=67)/non-IMH group (n=99) and Stanford type A (AAD-A, n=94)/type B (AAD-B, n=72). To evaluate circadian distribution, the day was divided into four 6-hour periods: night (00-06 hours), morning (06-12 hours), afternoon (12-18 hours), and evening (18-00 hours).
Results
Most (72%) AAD episodes were related to physical (53%) and mental activities (19%), with about one-third occurring during the afternoon, and only 12% occurring at night. No differences in triggering activities or circadian distribution were observed among the groups. Waking hours including morning, afternoon, and evening correlated with triggering activities (p=0.003). These relationships were observed for the non-IMH (p=0.008) and AAD-B (p=0.003) cases. The remaining categories had similar relationships, but did not reach statistical significance.
Physical and mental activities are considered as trigger factors for several cardiovascular diseases including acute myocardial infarction (AMI) and myocardial ischemia.1-3) In addition, there is considerable evidence indicating that numerous cardiovascular disorders including AMI,4-6) sudden death,7) and subarachnoidal hemorrhage8) are not randomly distributed over time but rather demonstrate chronobiological patterns of occurrence. Most acute aortic dissection (AAD) episodes are related to physical and mental activities,9) and the onset of AAD episodes peaks in the morning10) or during the day.9) Furthermore, triggering activities significantly contribute to a circadian distribution of the onset of AAD.9) However, limited data exist that examine about the relationship between activities that trigger AAD and their circadian distribution according to anatomical location.
Although intramural hematoma (IMH) is a variant or a precursor of AAD, and does not involve an intimal tear and continuous direct flow communication, the same treatment strategies have been applied for patients with IMH and AAD.11)12) Although in some cases IMH may rapidly regress, it may also proceed to dissection or aortic rupture.11) Patients with IMH show different clinical features and have a much better prognosis with medical treatment compared to those with classic AAD.12-14) In the context of limited available data, we hypothesized that there would be differences in triggering activities and their circadian distribution between patients with IMH and classic AAD. In the present study we investigated triggering activities and the circadian distribution of the onset of AAD. Our aim was to elucidate the relationship between both parameters in an analysis of subgroups sorted according to AAD anatomical location and the presence or absence of IMH.
Because traumatic or iatrogenic dissections are not influenced by chronobiologic patterns, these patients were excluded from the analysis. One hundred eighty-seven consecutive AAD patients who were admitted to Kyungpook National University Hospital between July 2001 and June 2009 were included in the present study. Twenty-one patients whose triggering activities or onset time of AAD were uncertain were excluded from further analysis. In total, 166 patients with AAD were included in this study. The data were retrospectively collected from hospital medical records. The diagnosis of AAD was based on clinical symptoms/signs including severe chest pain, back pain, abdominal pain, neurological signs, typical findings on computed tomography (CT), and transesophageal echocardiography. Cases of IMH were included in the present study. IMH was defined as a hemorrhage contained within the medial layer of the aortic wall with crescentic or circular thickening ≥7 mm, without intimal flap or intimal tear.15-18) To assess the influence of anatomical location, we divided the patients into Stanford type A dissection (AAD-A) defined as AAD involving the ascending aorta, and type B dissection (AAD-B) defined as AAD occurring distal to the left subclavian artery.19) To evaluate the seasonal distribution of onset of AAD, the year was divided into four seasons: spring (March-May), summer (June-August), autumn (September-November), and winter (December-February). To evaluate the circadian distribution of onset of AAD, the day was divided into four 6-hour periods: night (00-06 hours), morning (06-12 hours), afternoon (12-18 hours), and evening (18-00 hours). The protocol was reviewed and approved by the institutional review board. Written informed consent was obtained for all patients enrolled in the study.
The data were analyzed using the Statistical Package for the Social Sciences (SPSS) software (version 15.0; SPSS, Inc., Chicago, IL, USA). Data are presented as mean±standard deviation for continuous variables and number (percentage) for categorical variables. The Student's t-test was used for comparison of continuous variables, and Chi-square analyses were used for comparison of categorical variables. The distribution of triggering activities at the onset of AAD within four 6-hour periods was tested for uniformity in the overall population and in the various patients' subgroups by the Chi-square test for goodness of fit. A Chi-square value large enough to reject the hypothesis implied nonuniformity. A 2-sided p<0.05 was considered statistically significant.
The baseline characteristics of patients with AAD are listed in Table 1. The mean age of study patients was 59±14 years. No significant difference was found in gender proportions. Chest pain (51%) was the most common symptom, while hypertension (68%) was the most common risk factor for AAD. Most cases of AAD (95%) were detected by CT. Surgery was performed on 93 patients (56%). Eleven patients (7%) expired during hospitalization.
Triggering activities at the onset of AAD are shown in Tables 2 and 3. Most AAD cases (n=120, 72%) were related to physical (n=88, 53%) and mental (n=32, 19%) activities. The chronobiological distribution of the onset of AAD is reported in Table 2 and Fig. 1. In terms of seasonal distribution, AAD occurred most frequently in winter (33%) followed by spring (26%), autumn (22%), and summer (19%). In terms of monthly distribution, AAD occurred most frequently in December and January (11%, respectively), and least frequently in August (4%), followed by September (5%). There was homogeneity in the weekly distribution. In terms of the circadian distribution, AAD occurred most frequently at 12-14 hours (13%) followed by 18-20 hours (11%), 14-16 hours (11%), 16-18 hours (10%), 20-22 hours (10%), and 06-08 hours (10%). Therefore, about one-third of AAD episodes occurred during the afternoon, with the least (12%) occurring at night.
The relationship between triggering activities and the circadian distribution of the onset of AAD is reported in Fig. 2. Triggering activities were related to circadian distribution (p=0.003) (Fig. 2A). At night, AAD occurred frequently in patients with no triggering activities, whereas during the waking hours, AAD occurred frequently in patients with physical or mental activity. Baseline characteristics according to Stanford classification are listed in Table 1. Compared with the AAD-B group, the AAD-A group involved more women (p=0.004), chest pain (p<0.001) and surgery (p<0.001), and less frequently involved back pain (p<0.001) and abdominal pain (p=0.042). However, there was no significant difference in in-hospital mortality between the two groups (p=0.352).
Differences in triggering activities and the chronobiological distribution of the onset of AAD between patients with AAD-A and AAD-B are shown in Table 2. No significant difference was observed between the two groups in triggering factors. Compared with the AAD-B group, onset in the AAD-A group occurred more frequently during the autumn/winter (p=0.008). However, there was no significant difference in circadian distribution between the two groups (p=0.248).
The relationship between triggering activities and the circadian distribution of the onset of AAD according to Stanford classification is reported in Fig. 2. Although there was a relationship between triggering activities and the circadian distribution of the onset of AAD for the AAD-B group (p=0.003) (Fig. 2C), the relationship in the AAD-A group (p=0.197) did not reach statistical significance (Fig. 2B).
Baseline characteristics according to the presence or absence of IMH are listed in Table 1. Compared with the non-IMH group, the IMH group was older (p<0.001) with significantly more women (p<0.001), history of hypertension (p=0.001), and a significantly lower frequency of surgery (p=0.007). However, there was no significant difference in in-hospital mortality between the two groups (p=0.202).
Differences in triggering activities and chronobiological distribution at the onset of AAD according to the presence or absence of IMH are shown in Table 2. No significant difference in triggering factors was observed between the two groups. Furthermore, there was no significant difference in circadian distribution (p=0.100) or seasonal distribution (p=0.236) between the two groups.
The relationship between triggering activities and the circadian distribution of the onset of AAD according to the presence or absence of IMH is reported in Fig. 2. The relationship between triggering activities and the circadian distribution of the onset of AAD also held for the non-IMH group (p=0.008) (Fig. 2D). There was a trend towards a relationship between triggering activities and the circadian distribution of the onset of AAD in the IMH group (p=0.102), but it did not reach statistical significance (Fig. 2E).
The results of this study demonstrate that there is a significant relationship between triggering activities and the circadian distribution of AAD, and that this relationship also holds for AAD-B and non-IMH cases.
This study reveals that most AAD episodes (72%) are related to physical (53%) and mental (19%) activities. Previously, Matsuo reported that 65% of AAD episodes were triggered by mild effort or exercise.20) However, he did not categorize triggering activities in detail. Kojima et al.9) also showed that the onset of AAD was related to physical (74%) or mental activities (13%) in most patients (87%), with an increase in blood pressure (BP) being the most important factor. Many physical and mental activities are known to increase BP.21) In addition, the highly elevated BP peaks associated with physical and mental activity are known to trigger intimal tear or vasa vasorum rupture within the aortic media, which subsequently leads to AAD.22) Differences in patient populations may explain why AAD tends to occur more frequently with mental activity compared to previous studies.
There is considerable evidence suggesting that several major adverse cardiovascular events are not randomly distributed over time, but rather demonstrate chronobiological (circadian, weekly, and seasonal/monthly) patterns in their occurrence.10) Many studies have suggested that there is a chronobiological distribution to AAD onset.9)23)24) In terms of seasonal distribution, this study shows that AAD occurs most frequently in winter, followed by spring, summer, and autumn. A recent study also found that the onset of AAD showed marked seasonal variation with a peak in winter and a trough in summer.23) Another study demonstrated seasonal changes in hemodynamic measurements, suggesting that a cold climate causes sympathetically mediated vasoconstriction, leading to an elevation in BP.24) This may be a possible explanation for the observation in this study. In terms of monthly distribution, we found that AAD occurs most frequently in December, January, and March, and least frequently in September. This result is similar to that of another recent study23) and is likely related to the seasonal explanation suggested above. There is no difference in weekly distribution in this study. Recently a small peak for onset of AAD on Monday was found, but there was no significant overall variation.23) We have no clear explanation for the difference in weekly onset distribution for AAD and other serious cardiovascular disorders including AMI and sudden cardiac death with a peak on Monday. It may reflect differences in the external triggering factors among various diseases. In terms of circadian distribution, this study shows that the onset of most AAD is during the waking hours including morning, afternoon, and evening. Kojima et al.9) found that the onset of AAD also occured significantly more often during waking hours with most episodes occurring during the daytime (63% of episodes occurred between 06-18 hours) peaking at late morning (10-12 hours). A recent study showed that there was significant circadian variation in the occurrence of AAD, with a primary morning peak (08-11 hours) and a secondary evening peak (17-19 hours).23) As mentioned earlier, an increase in BP is considered one of the most important risk factors for AAD.9)21) BP rapidly increases after 07 hours and reaches a peak at mid-morning (around 10 hours), later peaking again in the evening (16-19 hours) in hypertensive and normotensive subjects.23) The circadian variation of BP may be a possible explanation for the daily distribution of AAD onset.
Compared with the AAD-B group, the AAD-A group experienced chest pain more frequently, and back and abdominal pain less frequently. It is reasonable that AAD-A involving the anterior portion of the aorta is more frequently associated with chest pain, while AAD-B, which involves the posterior and inferior portion of aorta, would be more frequently associated with back and abdominal pain. Interestingly, the present study finds that AAD-A is more frequent in female. A recent study showed that there was female bias in the occurrence of AAD-A, but the difference was not statistically significanct.25) These biases could be explained by older age and a tendency towards a history of high BP among females, as hypertension plays the most important role in the pathogenesis of AAD, and increases with age. However, there are no significant differences between the two groups regarding triggering factors in this study. Kojima et al.9) also demonstrated that triggering activities did not differ between the AAD-A and AAD-B groups. Moreover, this study found no difference in circadian distribution between the two groups. There are limited studies investigating a possible correlation between the anatomical location of AAD and its chronobiological distribution, and the fact that we found no significant difference may explain lack of published studies.
There was little data available examining triggering activities and the chronobiological distribution of the onset of AAD according to the presence or absence of IMH. In this study, no significant difference was observed between the two groups in triggering activities or the circadian distribution of the onset of AAD, although patients with IMH were older, more frequently female, and had a history of hypertension. However, one of the most important factors for the occurrence of AAD is an increase of BP, not a history of hypertension.9)21) Therefore, it is possible that there were no significant differences in essential mechanisms of AAD occurrence, such as BP increase, in the presence or absence of IMH.
The present study demonstrates that the occurrence of triggering activities was related to circadian distribution. AAD occurred less frequently in patients with triggering activities at night, whereas it occurred more frequently in patients with physical or mental activities during waking hours including morning, afternoon, and evening. Kojima et al.9) showed that daytime events were significantly more related to physical or mental activities than nighttime events (95% vs. 70%, p<0.001). It is well known that BP exhibits circadian variation.9)21)23) In a previous study, higher physical and mental activity levels also showed a pattern similar to that of elevation of BP.3) The circadian variation of BP together with increased physical and mental activity may be a possible explanation for the daily pattern of onset of AAD. There have been limited studies about the relationship between the circadian distribution and triggers of AAD onset in the context of anatomical location and the presence or absence of IMH. To the best of our knowledge, this study is the first one to reveal that the relationship between circadian distribution and triggering activities holds for AAD-B and non-IMH cases, whereas there is no significant relationship between the two parameters in AAD-A and IMH cases. We suppose that AAD-A and IMH could be influenced by another mechanism, which underlies the relationship between the two parameters. Therefore, further studies on the relationship between the two parameters according to anatomical location and the presence or absence of IMH are needed to confirm our results.
There are some potential limitations to the present study. First, there may be some selection bias because we collected data retrospectively from hospital medical records. Second, we did not assess the activity level of each patient, although physical activity seems to be an important triggering factor for AAD. Third, the timing of onset of AAD might be different from the real time of occurrence because we collected data retrospectively, as previously mentioned. However, this disparity would not influence the relationship between triggering activities and circadian distribution because of its lack of significant importance in the study design. Finally, we could not measure BP at the time of the occurrence of AAD. We therefore could not investigate an accurate relationship between BP and triggering activities or circadian distribution.
Most AAD is caused by triggering activities. Triggering activities are related to the circadian distribution of the onset of AAD. The circadian distribution of the onset of AAD does not differ according to anatomical classification or the presence or absence of IMH. This relationship also holds for non-IMH patients and those with AAD-B.
Figures and Tables
Fig. 1
The chronobiological distribution of onset of acute aortic dissection (AAD). A: AAD occurred most frequently in winter (33%) followed by spring (26%), autumn (22%), and summer (19%). B: AAD occurred most frequently in December and January (11%), and least frequently in August (4%), closely followed by September (5%). C: There was homogeneity in weekly distribution. D: AAD occurred most frequently at 12-14 hours (13%) followed by 18-20 hours (11%), 14-16 hours (11%), 16-18 hours (10%), 20-22 hours (10%), and 06-08 hours (10%). About one-third of AAD episodes occurred during the afternoon (bars with dark horizontal line) while the fewest (12%) occurred at night (bars with shallow left-downward line).

Fig. 2
The relationship between triggering activities and the circadian distribution of onset of acute aortic dissection (AAD). Presence of triggering activities was related to circadian distribution (p=0.003) (A). There was a trend towards triggering activities and the circadian distribution of the onset of AAD in the Stanford type A group (p=0.197), but the difference did not reach statistical significance (B). The relationship between triggering activities and the circadian distribution of AAD onset held in the Stanford type B group (p=0.003) (C). The relationship between triggering activities and the circadian distribution of the onset of AAD held for the non-intramural hematoma group (p=0.008) (D). There was a trend towards a relationship between triggering activities and circadian distribution of the onset of AAD in the intramural hematoma group (p=0.102), but the difference did not reach statistical significance (E). The distribution of triggering activities of the onset of AAD within four 6-hour periods was tested for uniformity in the overall population, and in the patient's subgroups by the Chi-square test for goodness of fit. A Chi-square value large enough to reject the hypothesis implied nonuniformity.

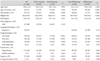
Table 1
Baseline characteristics of patients with acute aortic dissection according to Stanford classification and the presence or absence of intramural hematoma
Acknowledgments
The authors are deeply indebted to Roberto Patarca, MD, PhD for his useful suggestions during the preparation of this manuscript.
References
1. Mittleman MA, Maclure M, Tofler GH, Serwood JB, Goldberg RJ, Muller JE. Triggering of acute myocardial infarction by heavy physical exertion. Protection against triggering by regular exertion. N Engl J Med. 1993. 329:1677–1683.
2. Willich SN, Lewis M, Löwel H, Arntz HR, Schubert F, Schröder R. Physical exertion as a trigger of acute myocardial infarction. N Engl J Med. 1993. 329:1684–1690.
3. Krantz DS, Kop WJ, Gabbay FH, et al. Circadian variation of ambulatory myocardial ischemia: triggering by daily activities and evidence for an endogenous circadian component. Circulation. 1996. 93:1364–1371.
4. Kono T, Morita H, Nishina T, et al. Circadian variations of onset of acute myocardial infarction and efficacy of thrombolytic therapy. J Am Coll Cardiol. 1996. 27:774–778.
5. Marchant B, Ranjadayalan K, Stevenson R, Wilkinson P, Timmis AD. Circadian and seasonal factors in the pathogenesis of acute myocardial infarction: the influence of environmental temperature. Br Heart J. 1993. 69:385–387.
6. Gnecchi-Ruscone T, Piccaluga E, Guzzetti S, Contini M, Montano N, Nicolis E. Morning and Monday: critical periods for the onset of acute myocardial infarction. The GISSI 2 Study experience. Eur Heart J. 1994. 15:882–887.
7. Willich SN, Levy D, Rocco MB, Tofler GH, Stone PH, Muller JE. Circadian variation in the incidence of sudden cardiac death in the Framingham Heart Study population. Am J Cardiol. 1987. 60:801–806.
8. Gallerani M, Portaluppi F, Maida G, et al. Circadian and circannual rhythmicity in the occurrence of subarachnoid hemorrhage. Stroke. 1996. 27:1793–1797.
9. Kojima S, Sumiyoshi M, Nakata Y, Daida H. Triggers and circadian distribution of the onset of acute aortic dissection. Circ J. 2002. 66:232–235.
10. Mehta RH, Manfredini R, Hassan F, et al. Chronobiological patterns of acute aortic dissection. Circulation. 2002. 106:1110–1115.
11. Kim JK, Park SW, Jeong JO, et al. Clinical features and prognosis of acute aortic intramural hemorrhage compared with those of acute aortic dissection: a single center experience. Jpn Heart J. 2001. 42:91–100.
12. Hwang GS, Kim YH, Lee HS, et al. Clinical comparison of aortic intramural hemorrhage with aortic dissection involving the ascending aorta. Korean Circ J. 2000. 30:440–447.
13. Song JK, Kim HS, Song JM, et al. Multicenter longitudinal follow-up clinical study comparing the natural course of medically-treated patients with aortic dissection and aortic intramural hematoma. Korean Circ J. 2001. 31:592–601.
14. Lee IS, Kang DH, Song JK, et al. Clinical and echocardiographic outcome of aortic intramural hemorrhage compared with acute aortic dissection. Korean Circ J. 1998. 28:749–756.
15. Mohr-Kahaly S, Erbel R, Kearney P, Puth M, Meyer J. Aortic intramural hemorrhage visualized by transesophageal echocardiography: findings and prognostic implications. J Am Coll Cardiol. 1994. 23:658–664.
16. Nienaber CA, von Kodolitsch Y, Petersen B, et al. Intramural hemorrhage of the thoracic aorta: diagnostic and therapeutic implications. Circulation. 1995. 92:1465–1472.
17. Harris KM, Braverman AC, Gutierrez FR, Barzilai B, Dávila-Román VG. Transesophageal echocardiographic and clinical features of aortic intramural hematoma. J Thorac Cardiovasc Surg. 1997. 114:619–626.
18. Sueyoshi E, Matsuoka Y, Sakamoto I, Uetani M, Hayashi K, Narimatsu M. Fate of intramural hematoma of the aorta: CT evaluation. J Comput Assist Tomogr. 1997. 21:931–938.
19. Daily PO, Trueblood HW, Stinson EB, Wuerflein RD, Shumway NE. Management of acute aortic dissections. Ann Thorac Surg. 1970. 10:237–247.
20. Matsuo H. The thrombosed type of aortic dissection: its clinical features and diagnosis. Int J Angiol. 1998. 7:329–334.
21. Turjanmaa V, Tuomisto M, Fredrikson M, Kalli S, Uusitalo A. Blood pressure and heart rate variability and reactivity as related to daily activities in normotensive men measured with 24-h intra-arterial recording. J Hypertens. 1991. 9:665–673.
22. Fogelholm RR, Turjanmaa VM, Nuutila MT, Murros KE, Sarna S. Diurnal blood pressure variations and onset of subarachnoid haemorrhage: a population-based study. J Hypertens. 1995. 13:495–498.
23. Sumiyoshi M, Kojima S, Arima M, et al. Circadian, weekly, and seasonal variation at the onset of acute aortic dissection. Am J Cardiol. 2002. 89:619–623.
24. Izzo JL Jr, Larrabee PS, Sander E, Lillis LM. Hemodynamics of seasonal adaptation. Am J Hypertens. 1990. 3:405–407.
25. Nienaber CA, Fattori R, Mehta RH, et al. Gender-related differences in acute aortic dissection. Circulation. 2004. 109:3014–3021.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download