Abstract
Flash pulmonary edema typically exhibits sudden onset and resolves rapidly. It generally is associated with bilateral renal artery stenosis or unilateral stenosis in conjunction with a single functional kidney. We describe a patient who presented with flash pulmonary edema treated by percutaneous therapy with stent implantation. Our case is unique in that the flash pulmonary edema occurred in the setting of unilateral renal artery stenosis with bilateral functioning kidneys.
The clinical presentation of renal artery stenosis is varied. A common and well-recognized presentation is worsening pre-existing hypertension or declining renal function during antihypertensive therapy, particularly when angiotensin converting enzyme inhibitors or angiotensin receptor blockers are prescribed.1) An uncommon clinical presentation of renal artery stenosis is flash pulmonary edema, which is an episode of abrupt onset pulmonary edema that resolves rapidly. Flash pulmonary edema develops in patients with bilateral renal artery stenosis or unilateral renal artery stenosis with a solitary functioning kidney. Here we report a case of flash pulmonary edema due to unilateral renal artery stenosis with bilateral functioning kidneys.
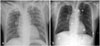
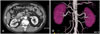
A 64-year-old man visited the emergency department with acute shortness of breath. It was his first episode, and it came on abruptly; twenty minutes earlier, he was asymptomatic and sleeping comfortably at home. His medical history included hypertension for more than five years, but he had not received treatment for it. He was a heavy smoker (45 pack years). Physical examination revealed arterial hypertension (260/140 mmHg). He had widespread wheezes and rales on auscultation, and the chest radiograph demonstrated bilateral interstitial shadowing (Fig. 1A). Additional investigations were performed. The serum creatinine level was in the normal range. The N-terminal pro-B-type natriuretic peptide (NT-proBNP) increased by 1,163 pg/mL. His electrocardiogram showed changes consistent with left ventricular hypertrophy and left atrial enlargement but no acute ischemic changes. Echocardiography demonstrated concentric left ventricular hypertrophy, left atrial enlargement, and diastolic dysfunction (grade 2) with an ejection fraction of 73%. He was hypoxic and was intubated and ventilated. After intubation, he improved rapidly without any special medications and was weaned from the mechanical ventilator within 1 hour. He was admitted to the intensive care unit for close observation. The pulmonary edema had subsided in the follow-up chest radiograph (Fig. 1B). These findings are characteristic of flash pulmonary edema. Since he had good left ventricular function we suspected a renovascular etiology for this pulmonary edema episode. CT angiography of the renal arteries revealed severe stenosis of the right renal artery ostium (Fig. 2). We performed a selective renal angiography, which revealed a 95% segmental ostial stenosis in the right renal artery (Fig. 3A), and a direct stent implantation (6.0×15 mm Genesis; maximum pressure of 12 atm) was performed (Fig. 3B). There was 10% residual stenosis and no detectable dissection. He remained stable for the next 48 hours without any complications. He was discharged, and out-patient follow-up was arranged. He has remained free of pulmonary edema and hypertension. Follow-up CT angiography revealed no restenosis two months after the stent placement (Fig. 3C).
Flash pulmonary edema typically exhibits sudden onset and resolves rapidly with acute pulmonary venous congestion.2) Renal artery stenosis can present in the acute state as flash pulmonary edema, but this is rare. A previous study, conducted between 1989 and 1998, followed 148 patients with renal artery stenosis, who were treated with stent insertion; only two patients (1%) presented with flash pulmonary edema.3)
Flash pulmonary edema usually is associated with bilateral renal artery stenosis or stenosis of a single surviving kidney,2) but no case had been reported involving unilateral stenosis in a patient with bilateral functioning kidneys prior to our case.
The mechanism by which renal artery stenosis causes pulmonary edema is not well understood, but the renin-angiotensin-aldosterone system (RAS) appears to be essential for the development of renovascular hypertension and flash pulmonary edema. Garovic et al.4), demonstrated that 1-kidney-1-clip models (analogous to bilateral renal artery disease or stenosis with a solitary functioning kidney) differs from 2-kidney-1-clip hypertension (analogous to unilateral stenosis with bilateral functioning kidneys): 1-kidney-1-clip hypertension is volume dependent,4) whereas 2-kidney-1-clip is angiotension-II dependent. In patients with bilateral renal artery stenosis or unilateral renal artery stenosis with a solitary functioning kidney, volume overload occurs, which can lead to increased left atrial pressure and pulmonary edema. In renal artery stenosis renin is released from the juxtaglomerular apparatus causing intravascular expansion via sodium and water retention. In unilateral renal artery stenosis with a normal contralateral kidney renin release can be suppressed in the normal kidney resulting in a natriuresis, which protects patients from pulmonary edema. However, with bilateral renal artery stenosis or unilateral renal artery stenosis with a single functioning kidney, a compensatory natriuresis cannot occur, resulting in fluid overload and, subsequently, pulmonary edema.4)
In the context of flash pulmonary edema pathophysiology our case is unique because flash pulmonary edema occurred with unilateral renal artery stenosis and bilateral functioning kidneys (analogous to the 2-kidney-1-clip model). In patients with hypertensive pulmonary edema and a normal ejection fraction it has been reported that the edema is due to diastolic dysfunction, otherwise known as diastolic heart failure.5) We speculate that the initial small increase in the left end-diastolic volume precipitated by activation of the renin-angiotensin-aldosterone system may be associated with a marked elevation in the diastolic pressure of patients with severe diastolic dysfunction (i.e., this case), which contributes to the development of pulmonary edema. Indeed echocardiography showed concentric left ventricular hypertrophy and diastolic dysfunction (grade 2) with normal systolic function. We propose that in a patient with severe diastolic dysfunction, even a unilateral renal artery stenosis with bilateral functioning kidneys can evoke flash pulmonary edema. Further investigations are needed to evaluate this hypothesis. Renal artery stenosis should be considered in hypertensive patients presenting with pulmonary edema and normal systolic function.
Screening tests for renal artery stenosis have improved considerably. Captopril renography was used almost exclusively in the past. Doppler ultrasonography is not a reliable technique because of its high failure rate. Magnetic resonance or CT angiography are possible alternatives, and both imaging modalitites provide additional imaging of the abdominal aorta and three-dimensional visualizations.5) CT angiography made an accurate diagnosis possible in our patient.
Three possible strategies can be used to treat RAS: medical management, surgical management, or percutaneous therapy.6-8) The recently published American Heart Association/American College of Cardiology (AHA/ACC) peripheral arterial disease guidelines includes class I and IIa indications for renal revascularization in several clinical subsets.9) Labile hypertension, progressive renal failure, and flash pulmonary edema may be strong indications for revascularization.10)11) Percutaneous renal artery stenting has replaced surgical revascularization for most patients who meet the criteria for intervention.12) In this case renal stenting was performed, and the patient has remained free of pulmonary edema and hypertension. However, it is of concern that hypertension is cured only rarely (<10%) in patients with atherosclerotic renovascular disease, and kidney function deteriorates rapidly in a subset of patients (20%) due to atheroembolic disease after renal angioplasty. Hence, it is prudent to select patients for renal stenting carefully.
Flash pulmonary edema is a rare manifestation of renal artery stenosis. Flash pulmonary edema occurred in a patient exhibiting unilateral renal artery stenosis with bilateral functioning kidneys, most likely due to diastolic dysfunction of the left ventricle. Revascularization with stent insertion was performed successfully.
Figures and Tables
Fig. 1
Chest radiograph demonstrates bilateral interstitial shadowing compatible with pulmonary edema (A) that subsided soon after admission (B).
Acknowledgments
We thank Ms. Gyeong-Ja Jeong and Ms. Youn-Jin Noh for their assistance in writing this manuscript.
References
1. Pun E, Dowling RJ, Mitchell PJ. Acute presentations of renal artery stenosis in three patients with a solitary functioning kidney. Australas Radiol. 2004. 48:523–527.
2. Sharifkazemi MB, Zamirian M, Astani A. Flash pulmonary edema heralding renal artery spasm. Cardiology. 2008. 109:66–67.
3. Perkovic V, Thomson KR, Mitchell PJ, et al. Treatment of renovascular disease with percutaneous stent insertion: long-term outcomes. Australas Radiol. 2001. 45:438–443.
4. Garovic VD, Textor SC. Renovascular hypertension and ischemic nephropathy. Circulation. 2005. 112:1362–1374.
5. Gandhi SK, Powers JC, Nomeir AM, et al. The pathogenesis of acute pulmonary edema associated with hypertension. N Engl J Med. 2001. 344:17–22.
6. Choi DH, Hong BK, Shim WH, Jang YS, Cho SY. Stenting in renal artery stenosis. Korean Circ J. 1997. 27:703–711.
7. Olin JW. Renal artery disease: diagnosis and management. Mt Sinai J Med. 2004. 71:73–85.
8. Oh GY, Lee GH, Jeon DS, et al. A case of renal hypertension with unilateral renal artery stenosis and contralateral hypoplastic kidney. Korean Circ J. 1998. 28:448–452.
9. White CJ. Catheter-based therapy for atherosclerotic renal artery stenosis. Prog Cardiovasc Dis. 2007. 50:136–150.
10. Choo DC, Fisher DZ. Renal artery stenosis: when to intervene? Cardiol Rev. 2003. 11:257–261.
11. Mansoor S, Shah A, Scoble JE. Flash pulmonary oedema: a diagnosis for both the cardiologist and the nephrologist? Nephrol Dial Transplant. 2001. 16:1311–1313.
12. Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): executive summary a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease) endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. J Am Coll Cardiol. 2006. 47:1239–1312.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download