Abstract
Background and Objectives
Pentraxin 3 (PTX3) was shown to be elevated in the acute phase of acute myocardial infarction (AMI) and to have prognostic significance in AMI patients. The aim of this study was to estimate whether the value of PTX3 could be used as a prognostic biomarker, with the global registry of acute coronary events (GRACE) risk assessment tool, in patients with acute coronary syndrome (ACS).
Subjects and Methods
Between July 2007 and June 2008, 137 patient subjects (mean age : 61±12 years, M : F=108 : 29) with ACS who underwent coronary intervention, but did not have a prior percutaneous coronary intervention (PCI) and/or follow-up coronary angiogram, were enrolled. We estimated the all-cause mortality or death/MI, in-hospital and to 6 months, using the GRACE risk scores and compared these estimates with serum PTX3 concentrations.
Results
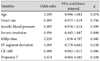
The serum PTX3 concentration showed a significant increase in ST segment elevation myocardial infarction (STEMI) greater than the unstable angina pectoris (UAP) group (2.4±2.1 ng/mL vs. 1.3±0.9 ng/mL, p= 0.017, respectively), but did not show a significant difference between non-ST segment elevation myocardial infarction (NSTEMI) and the UAP group (1.9±1.4 ng/mL vs. 1.3±0.9 ng/mL, p=0.083, respectively). The serum PTX3 concentration was closely related to death/MI in-hospital (r=0.242, p=0.015) and death/MI to 6 months (r=0.224, p=0.023), respectively. The serum PTX3 concentration was not related to all-cause mortality in-hospital (r=0.112, p=0.269) and to 6 months (r=0.132, p=0.191), respectively. Among the parameters determining the GRACE risk scores, the degree of Killip class in congestive heart failure (CHF) was independently associated with the supramedian PTX3 concentration [odds ratio: 2.229 (95% confidence interval: 1.038-4.787), p=0.040].
Inflammation plays a key role in the initiation, development and progression of atherosclerosis. The association of increased serum levels of acute-phase proteins with the progression of atherosclerosis and with the occurrence of atherosclerosis-related adverse events, such as coronary heart disease and myocardial infarction (MI), has been well documented in several epidemiological studies.1-6)
Currently, the pentraxin protein family is divided into two subfamilies based on size: the classical "short" pentraxin (25 kDa) and the "long" pentraxin (40-50 kDa). Pentraxin 3 (PTX3) is a "long" pentraxin that is highly expressed in the heart, whereas C-reactive protein (CRP) is a "short" pentraxin and is produced from the liver.7) In several recent studies,8)9) PTX3 appeared to be not only an early indicator of irreversible myocyte injury, but also a prognostic marker in patients with acute myocardial infarction (AMI).
The global registry of acute coronary events (GRACE) risk score,10)11) designed in 94 hospitals and 14 countries, has been used as a tool to predict death in-hospital12) and death after discharge13) in patients with acute coronary syndrome (ACS). The GRACE risk score is represented by the following three categories; ST segment elevation MI (STEMI), non-ST segment elevation MI (NSTEMI), and unstable angina pectoris (UAP). ACS represents a broad spectrum of ischemic myocardial events including UA, NSTEMI, and STEMI that are associated with high morbidity and mortality despite early diagnosis, medical intervention and management.14)
Our hypothesis is that PTX3 is a prognostic biomarker in patients with ACS. We estimated the all-cause mortality or death/MI, in-hospital and to 6 months, using the GRACE risk scores and compared these estimates to serum PTX3 concentrations. The aim of this study was to prove whether the value of PTX3 could be a prognostic marker, with the use of the GRACE risk assessment tool, in ACS patients.
Between July 2007 and June 2008, at the Uijeongbu St. Mary's Hospital, 137 patient subjects with ACS, with or without ST segment elevation, underwent percutaneous coronary intervention (PCI); those who had no prior PCI and/or follow-up coronary angiography were enrolled.
There were 108 male and 29 female patients enrolled, with a mean age of 61±12 years. Our institutional review committee approved this study. Patients were informed of the investigative nature of the study, and written informed consent was obtained before enrollment.
Patients with ACS were classified into the following standard subtypes: STEMI, NSTEMI and UAP. The GRACE diagnostic criteria of inclusion for AMI, according to the rationale and design of the GRACE investigators, was met if patients had a cardiac ischemic symptom and at least one of the following increases in cardiac enzymes: 1) creatine kinase MB fraction (CK-MB) >2 times upper limit of the hospital's normal range, and/or 2) positive Troponin T result.10) NSTEMI was defined as occurrence of acute MI with positive cardiac enzyme results, with or without accompanying electrocardiographic changes other than ST segment elevation. STEMI was defined as persistent ST segment elevation of ≥1 mm in 2 contiguous electrocardiographic leads or the presence of a new left bundle branch block with positive cardiac enzyme results.10) The diagnostic inclusion criteria for UAP, according to the rationale and design of the GRACE investigators, was met if patients had a cardiac ischemic symptom with serial enzymes and ST segment elevation negative for MI.10) Patients were excluded if they had 1) prior PCI and/or follow-up coronary angiogram, or 2) prior coronary artery bypass graft (CABG).
Each patient's individual GRACE risk score, including the parameters of age, heart rate, systolic blood pressure, serum creatinine level, Killip class, presence of cardiac arrest at admission, ST segment deviation, and elevated cardiac enzymes for all-cause mortality, in-hospital and to 6 months, was calculated using the published risk score calculator from the GRACE registry. Full details of the GRACE risk assessment tool have been previously published.10) We estimated the all-cause mortality or death/MI, in-hospital and to 6 months, using the GRACE risk scores and compared it with serum PTX3 concentrations.
A coronary angiogram was performed using the Judkins' method, following the puncture of the femoral artery or via a radial artery approach according to current guidelines from the American College of Cardiology/American Heart Association/Society for Cardiovascular Angiography and Intervention (ACC/AHA/SCAI) 2005 guideline update for PCI.15) Significant stenosis was defined as a diameter stenosis of 50% or greater. A standard antiplatelet therapy and other medications for ACS were provided according to current guidelines from the ACC/AHA16)17) and the European Society of Cardiology (ESC).18) In all patients, aspirin (300 mg/day) and clopidogrel (600 mg/day) were loaded before procedure. An intravenous bolus of 100 U/kg weight of unfractionated heparin was given, and then additional heparin boluses were given to maintain an activated clotting time of 250-300 seconds during the procedure.19)20)
During the procedure, blood was drawn into ethylenediaminetetraacetic acid vacuum containers. PTX3 was assayed with a noncommercial enzyme linked immuno sorbent assay (ELISA), based on the monoclonal antibody MNB10 and rabbit anti-serum. The ELISA assay did not cross-react with the short pentraxin CRP.
Continuous variables are expressed as mean±standard deviation (SD). Group comparisons for continuous variables of baseline clinical characteristics were performed using the analysis of variance test, and analysis for categorical data was performed using the χ2 test. Comparisons between the groups for serum PTX3 concentration were analyzed using an independent t-test, which was conducted using the SAS statistical software, version 9.1 (SAS Institute, Cary, NC, USA). In multivariate logistic regression analysis, the value for median serum PTX3 concentration was used as a cut-off point to determine an independent parameter for all-cause mortality in-hospital and to 6 months. Statistical significance was set at p<0.05.
A total of 137 consecutive patients with ACS (mean age, 61±12 years, M : F ratio 108 : 29), including 76 (55.5%) with STEMI, 38 (27.7%) with NSTEMI, and 23 (16.6%) with UAP, were studied. The baseline clinical and laboratory findings of the three groups were summarized in Table 1.
The serum PTX3 concentration was not correlated with CRP (r=0.199, p=0.058), CK-MB (r=0.022, p=0.830), ischemia modified albumin (r=-0.103, p=0.375), brain natriuretic peptide albumin (r=0.159, p=0.296) and pro-brain natriuretic peptide (r=0.260, p=0.074). The serum PTX3 concentration was significantly correlated with Troponin T (r=0.332, p=0.001) (Fig. 1).
The serum PTX3 concentration was significantly correlated to death/MI in-hospital (r=0.242, p=0.015) and death/MI to 6 months (r=0.227, p=0.023). The serum PTX3 concentration was not correlated to all-cause mortality in-hospital (r=0.112, p=0.269) and to 6 months (r=0.132, p=0.191) (Table 2).
The serum PTX3 concentration exhibited a significant increase in STEMI (2.4±2.1 ng/mL) as compared to the UAP group (1.3±0.9 ng/mL) with a p=0.017. But there was no significant difference between the NSTEMI and UAP groups (1.9±1.4 ng/mL vs. 1.3±0.9 ng/mL, p=0.083, respectively), as well as between the STEMI and NSTEMI groups (2.4±2.1 ng/mL vs. 1.9±1.4 ng/mL, p=0.185, respectively) (Fig. 2).
Among the parameters determining the GRACE risk scores, the degree of Killip class in congestive heart failure (CHF) was independently associated with the supramedian PTX3 concentration [odds ratio: 4.221 (95% confidence interval: 1.038-4.787), p=0.040] (Table 3).
The cut-off value of serum PTX3 concentration (0.88 ng/mL) shows a sensitivity (87.5%) and a specificity (69.1%) for predicting the probability of all-cause mortality in-hospital (>3%), as the highest tertile of GRACE risk assessment, and the cut-off value of serum PTX3 concentration (0.92 ng/mL) shows a sensitivity (78.2%) and a specificity (50.0%) for predicting the probability of death/MI in-hospital (>5%) (Fig. 3).
Although CRP has been used as a worldwide diagnostic biomarker in ischemic heart diseases, the increased serum CRP levels in the acute conditions such as ACS have been considered a nonspecific response to myocardial injury,21) and the actual role of CRP in the pathogenesis of heart damage is still debated.22)23) Peri et al.8) reported serum PTX3 as an early indicator of AMI in humans and with no correlation between serum concentrations of PTX3 and CRP.
The GRACE risk scoring system, a multinational registry involving all subsets of ACS including STEMI, NSTEMI and UAP, derived from clinical parameters at the time of hospitalization, was found to accurately predict mortality at 6 months.10) Parameters in this GRACE scoring system are age, history of CHF, history of MI, elevated resting heart rate, low systolic blood pressure on arrival, ST-segment depression, elevated initial serum creatinine, and elevated cardiac enzymes in-hospital.10) Recently, Latini et al.9) reported the acute-phase protein PTX3 as a predictor of 3-month mortality after adjustment for major risk factors and other acute-phase prognostic markers. In our results, the role of PTX3 as a prognostic biomarker was shown by an increased serum PTX3 that was closely related to death due to MI, in-hospital or to 6 months, in ACS patients, including STEMI, NSTEMI, and UAP groups.
Recently, several studies have mentioned that the plasma PTX3 level had increased in patients with heart failure and was independently associated with an increased risk for cardiac events.24)25) Suzuki et al.24) demonstrated that the concentration of plasma PTX3 levels was significantly higher in patients with heart failure than in control subjects and increased with advancing New York Heat Association (NYHA) functional class, especially in severe patients with heart failure and NYHA class III or IV. In this study, the serum PTX3 concentration was significantly correlated to Troponin T and the degree of Killip class, in CHF, among the parameters determining the GRACE risk scores, and the degree of Killip class was independently associated with an incremental change in the serum PTX3 level. To establish the role of PTX3 in the pathophysiology of CHF, further investigations are required in larger populations via multicenter trials.
Inflammatory mediators are intimately associated with the cascade of events leading to atherosclerotic plaque initiation, development, and rupture. A study by Inoue et al.26) compared 52 patients with stable angina pectoris (SAP) to 16 patients with UAP and reported that PTX3 was not associated with coronary risk factors including hypertension, diabetes mellitus and hyperlipidemia; the value of PTX3 was significantly higher in the UAP than in the SAP group. They suggested that the levels of plasma PTX3 had increased in patients with arterial inflammation, especially UAP, and that the detection of PTX3 was due to PTX3 having originated from the atherosclerotic plaque itself, thereby reflecting active atherosclerosis. Therefore, 'PTX3' will be useful for the prediction of UAP.
In contrast, Salio et al.27) reported, in a mouse model, that PTX3 plays a nonredundant, regulatory, cardioprotective role in AMI and suggested that modulation of the complement cascade contributes to the cardioprotective function of PTX3. Although our data found much evidence converging to support Inoue's report, we need to conduct further research in a larger population.
Kotooka et al.28) reported that PCI also induces a significant inflammatory reaction in the injured vessel wall and enhances plasma PTX3 concentration that leads to the development of neointimal thickening and restenosis after coronary stenting. However, to elucidate the mechanism of in-stent restenosis after PCI, more analysis of PTX3 is warranted.
There are several limitations in our present study. First, there is the limitation of "time gap" between the sampling of PTX3 during the procedure and the calculation of GRACE risk score at admission, including the difference of "door to balloon time" (STEMI : NSTEMI : UAP; 2.6±2.4 : 8.9±9.7 : 17.2±7.2, respectively, p=0.001). Second, despite several studies indicating PTX3 as a prognostic biomarker of ACS, a normal range for PTX3 levels has not been established. Last, our investigators suggest that the actual long-term outcomes in ACS patient subjects could be confirmed via future follow-up coronary angiography or telephone interview.
The Killip class that reflects CHF is an independent factor associated with an incremental change in the serum PTX3 level. Our investigators suggest that the serum PTX3 level provides important information for risk stratification of CHF diagnosis, among the parameters determining GRACE risk scores of ACS subjects, including subtypes STEMI, NSTEMI and UAP.
Figures and Tables
Fig. 1
The relationship between PTX3 and several biomarkers. PTX3: pentraxin 3, CRP: C-reactive protein, CK-MB: creatine kinase myoglobulin, IMA: ischemia modified albumin, BNP: brain natriuretic peptide, pro-BNP: pro-brain natriuretic peptide.

Fig. 2
The relationship between PTX3 and ACS, including STEMI, NSTEMI and UAP groups. PTX3: pentraxin 3, ACS: acute coronary syndrome, STEMI: ST segment elevation myocardial infarction, NSTEMI: non-ST segment elevation myocardial infarction, UAP: unstable angina pectoris.
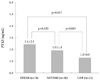
Fig. 3
ROC curve. The cut-off value of serum PTX3 concentration 0.88 ng/mL shows a sensitivity 87.5% and a specificity 69.1% for predicting the probability of all-cause mortality in-hospital (>3%), as the highest tertile of GRACE risk assessment in (A), and the cut-off value of serum PTX3 concentration 0.92 ng/mL shows a sensitivity 78.2% and a specificity 50.0% for predicting the probability of death/MI in-hospital (>5%) in (B). ROC: receiver operating characteristics, AUC: area under curve, CI: confidence interval, PTX3: pentraxin 3, GRACE: global registry of acute coronary events, MI: myocardial infarction.

Table 1
Baseline clinical and laboratory characteristics

STEMI: ST segment elevation myocardial infarction, NSTEMI: non-ST segment elevation myocardial infarction, UAP: unstable angina pectoris, BPM: beats per minute, bpm: breaths per minute, HDL-C: high density lipoprotein-cholesterol, LDL-C: low density lipoprotein-cholesterol, pentraxin 3: PTX3, ck-MB: creatine kinase myoglobulin, BNP: brain natriuretic peptide, pro-BNP: pro-brain natriuretic peptide, GRACE: global registry of acute coronary events, MI: myocardial infarction
Acknowledgments
This study was supported by a grant from the Seoul R & BD Program of the Republic of Korea (#10526).
References
1. Noh HJ, Kwon NH, Joo SB. Severity of coronary atherosclerosis: influence of metabolic syndrome risk factor clustering and hs-CRP. Korean Circ J. 2006. 36:802–808.
2. Doo YC, Park WJ, Park SH, et al. The optimal timing to measure C-reactive protein to predict cardiac events in patients with unstable angina. Korean Circ J. 2001. 31:290–296.
3. Kim TI, Chae SC, Yang DH, et al. Short-term prognostic value of CRP in the patients with acute coronary syndrome. Korean Circ J. 2000. 30:1387–1394.
4. Haverkate F, Thompson SG, Pyke SD, Gallimore JR, Pepys MB. Production of C-reactive protein and risk of coronary events in stable and unstable angina. European Concerted Action on Thrombosis and Disabilities Angina Pectoris Study Group. Lancet. 1997. 349:462–466.
5. Rossi E, Biasucci LM, Citterio F, et al. Risk of myocardial infarction and angina in patients with severe peripheral vascular disease: predictive role of C-reactive protein. Circulation. 2002. 105:800–803.
6. Rolph MS, Zimmer S, Bottazzi B, Garlanda C, Mantovani A, Hansson GK. Production of the long pentraxin PTX3 in advanced atherosclerotic plaques. Arterioscler Thromb Vasc Biol. 2002. 22:e10–e14.
7. Garlanda C, Bottazzi B, Bastone A, Mantovani A. Pentraxins at the crossroads between innate immunity, inflammation, matrix deposition, and female fertility. Annu Rev Immunol. 2005. 23:337–366.
8. Peri G, Introna M, Corradi D, et al. PTX3, a prototypical long pentraxin, is an early indicator of acute myocardial infarction in humans. Circulation. 2000. 102:636–641.
9. Latini R, Maggioni AP, Peri G, et al. Prognostic significance of the long pentraxin PTX3 in acute myocardial infarction. Circulation. 2004. 110:2349–2354.
10. GRACE Investigators. Rationale and design of the GRACE (global registry of acute coronary events) project: a multinational registry of patients hospitalized with acute coronary syndrome. Am Heart J. 2001. 141:190–199.
11. Eagle KA, Goodman SG, Avezum A, Budaj A, Sullivan CM, López-Sendón J. Practice variation and missed opportunities for reperfusion in ST-segment-elevation myocardial infarction: findings from the global registry of acute coronary events (GRACE). Lancet. 2002. 359:373–377.
12. Granger CB, Goldberg RJ, Dabbous O, et al. Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med. 2003. 163:2345–2353.
13. Eagle KA, Lim MJ, Dabbous OH, et al. A validated prediction model for all forms of acute coronary syndrome: estimating the risk of 6-month postdischarge death in an international registry. JAMA. 2004. 291:2727–2733.
14. Das R, Kilcullen N, Morrell C, Robinson MB, Barth JH, Hall AS. The British Cardiac Society Working Group definition of myocardial infarction: implications for practice. Heart. 2006. 92:21–26.
15. Smith SC Jr, Feldman TE, Hirshfeld JW Jr, et al. ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update the 2001 Guidelines for Percutaneous Coronary Intervention). J Am Coll Cardiol. 2006. 47:e1–e121.
16. Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-Elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J Am Coll Cardiol. 2007. 50:e1–e157.
17. Antman EM, Hand M, Armstrong PW, et al. 2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration With the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, Writing on Behalf of the 2004 Writing Committee. Circulation. 2008. 117:296–329.
18. Bassand JP, Hamm CW, Ardissino D, et al. Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes. Eur Heart J. 2007. 28:1598–1660.
19. King SB 3rd, Smith SC Jr, Hirshfeld JW Jr, et al. 2007 Focused Update of the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention: a report of the American College of Cardiology/ American Heart Association Task Force on Practice Guidelines: 2007 Writing Group to Review New Evidence and Update the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention, Writing on Behalf of the 2005 Writing Committee. Circulation. 2008. 117:261–295.
20. KingSB 3rd, Smith SC Jr, Hirshfeld JW Jr, et al. 2007 focused update of the ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice guidelines. J Am Coll Cardiol. 2008. 51:172–209.
21. de Beer FC, Hind CR, Fox KM, Allan RM, Maseri A, Pepys MB. Measurement of serum C-reactive protein concentration in myocardial ischaemia and infarction. Br Heart J. 1982. 47:239–243.
22. Verma S, Devaraj S, Jialal I. Is C-reactive protein an innocent bystander or proatherogenic culprit?: C-reactive protein promotes atherothrombosis. Circulation. 2006. 113:2135–2150.
23. Scirica BM, Morrow DA. Is C-reactive protein an innocent bystander or proatherogenic culprit?: the verdict is still out. Circulation. 2006. 113:2128–2134.
24. Suzuki S, Takeishi Y, Niizeki T, et al. Pentraxin 3, a new marker for vascular inflammation, predicts adverse clinical outcomes in patients with heart failure. Am Heart J. 2008. 155:75–81.
25. Kotooka N, Inoue T, Aoki S, Anan M, Komoda H, Node K. Prognostic value of pentraxin 3 in patients with chronic heart failure. Int J Cardiol. 2008. 130:19–22.
26. Inoue K, Sugiyama A, Reid PC, et al. Establishment of a high sensitivity plasma assay for human pentraxin3 as a marker for unstable angina pectoris. Arterioscler Thromb Vasc Biol. 2007. 27:161–167.
27. Salio M, Chimenti S, De Angelis N, et al. Cardioprotective function of the long pentraxin PTX3 in acute myocardial infarction. Circulation. 2008. 117:1055–1064.
28. Kotooka N, Inoue T, Fujimatsu D, et al. Pentraxin3 is a novel marker for stent-induced inflammation and neointimal thickening. Atherosclerosis. 2008. 197:368–374.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download