Abstract
Elective surgical repair has traditionally been considered to be the treatment of choice for the exclusion of isolated iliac artery aneurysms (IAAs). Recently, endovascular repair has evolved as an alternative to surgical repair, especially in patients at high surgical risk. However, in the absence of sufficient proximal necks, iliac artery aneurysms are not suitable for direct deployment of a tubular-shaped endograft. Here we report two cases of IAAs with short proximal necks that were excluded using an endovascular bifurcated stent-graft. The bifurcated stent-graft was successfully deployed with complete exclusion of the aneurysm. In neither case was there evidence of procedural failures. There were no signs of significant complications. We conclude that endovascular repair of IAAs with short proximal necks is feasible and efficient using an endovascular bifurcated stent-graft.
Isolated iliac artery aneurysms (IAAs) occurring in the absence of abdominal aortic aneurysm (AAA) are relatively uncommon. They represent only 2% of all intra-abdominal aneurysms.1) Although data on the natural history of IAAs are limited due to their rarity, expansive growth and subsequent rupture has been well documented in several cases.2) Some reports have suggested that isolated IAAs have a high risk of rupture, with an associated high mortality rate of up to 80%.2)3) To prevent the mortality associated with IAAs, patients with significant risk of rupture should be identified and considered for prophylactic repair. IAA diameter has been used most commonly as a surrogate for rupture risk, with repair recommended in patients with an IAA diameter >3-4 cm.4) Elective surgical repair has traditionally been considered to be the treatment of choice for IAAs. Recently, endovascular repair of isolated IAAs has emerged as an alternative to surgical repair, especially in patients at high surgical risk. However, endovascular repair using a tubular-shaped endograft is not efficient in the case of a short or absent proximal landing zone (<1.5 cm) or extension into the aortic bifurcation. For these patients, we recommend bifurcated stent grafting as described in the following two case reports.
A 54-year-old male patient was referred from the oncology division for management of an IAA discovered incidentally during a routine abdominal computed tomography (CT) scan performed for follow-up after chemotherapy. He had undergone radical nephrectomy for right renal cell carcinoma in 2001. After surgery he had been treated with chemotherapy several times. An abdominal CT scan showed a 39-mm, partially thrombosed aneurysm with a short proximal neck involving the entire length of the right common iliac artery (CIA) (Fig. 1A). The patient did not complain of any symptoms associated with an aneurysm. An initial examination revealed a blood pressure of 130/80 mmHg, a heart rate of 78 beats per minute, and a respiratory rate of 14 breaths per minute. Routine laboratory tests, including complete blood count, blood chemistry, liver function tests, serum electrolytes, and bleeding times, were all normal.
We decided to attempt endovascular repair using aorto-iliac bifurcated stent-grafts for the treatment of an iliac aneurysmal lesion, because the patient was reluctant to undergo surgical treatment. Furthermore, the patient had a previous open abdominal surgery because of renal cell carcinoma and was expected to be a difficult candidate for aorto-iliac surgery due to possible intra-abdominal adhesions. All procedures were performed in a fully-equipped cardiac catheterization room with constant patient monitoring. Bilateral femoral arterial access was obtained percutaneously under regional anesthesia. Heparin (5,000 units) was administered intraarterially prior to the procedure.
The patient underwent pre-procedural aortic angiography to evaluate the anatomic configuration of the aorto-iliac system (Fig. 1C). Embolization of the right internal iliac artery (IIA) was performed using Amplatzer vascular plugs before stent grafting to ensure aneurysm exclusion. AneuRx (Medtronic, Minneapolis, MN, USA) 4-piece bifurcated stentgrafts were implanted; a 26×35×151-mm trunk component was positioned at the infra-renal abdominal aorta into the left CIA, while a 16×85-mm left iliac limb, a 15×151-mm right iliac limb, and a 16×85-mm right iliac extension were deployed from the aorto-iliac bifurcation to each iliac artery. Deployed stent-grafts were subsequently dilated with a 33-mm Equalizer occlusion balloon catheter (Boston Scientific, Natick, MA, USA). The femoral access site was closed percutaneously using two Perclose AT devices (Abbott Vascular Devices, Redwood City, CA, USA) pre-applied at a 90° angle before the insertion of stent-grafts.
On completion of the procedure, a final angiogram revealed accurate positioning of the stent-grafts that achieved complete exclusion of the aneurysm (Fig. 1D). There was no evidence of graft migration, endoleaks, distal embolization, or access site complications. Follow-up CTs performed 3 days and 6 months after the interventional procedure showed the complete exclusion of the aneurysm and no endoleak (Fig. 1B).
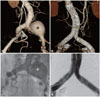
An 80-year-old male patient was referred from the urology department because of an incidental diagnosis of an IAA during an abdominal CT scan performed for evaluation of prostate cancer. CT angiography revealed a 50-mm huge left CIA aneurysm with a short (<1 cm) proximal neck (Fig. 2A). The patient had hypertension that had been treated with medication for 3 years. He did not present with any symptoms and his physical examination and routine laboratory values were all normal.
Because of his very old age and general condition, we decided to attempt endovascular repair using aorto-iliac bifurcated stent-grafts. Because of his very old age and general condition, we decided to attempt endovascular repair using aortoiliac bifurcated stent-grafts following the same procedure detailed in case (preprocedural angiographic image) (Fig. 2C). Following the same procedure detailed in case 1, Excluder (Gore, Flagstaff, AZ, USA) 3-piece bifurcated endografts were implanted; we then implanted a 23×12×180-mm aorta-to-right CIA limb, a 12×140-mm aorta-to-left CIA limb, and a 16×12×70-mm left iliac extension. Prior to implantation of a bifurcated stent-graft, IIA embolization using Nester coils (Cook Inc., Bloomington, IN, USA) was performed on the right side as well as on the left side because of a combined diffuse ectatic change in the right CIA.
The final angiogram showed aneurysm exclusion with no signs of endoleak and accurate positioning of the stentgrafts (Fig. 2D). No significant complications were reported. Follow-up CTs performed 3 days and 6 months after the procedure showed successful exclusion of the IAA without endoleaks (Fig. 2B).
Isolated IAAs are defined as aneurysms located only within the iliac artery system without involvement of the aorta. True isolated IAAs without aortic involvement are quite rare. Their prevalence in the general population is estimated at 0.03%, accounting for only 2% of all intra-abdominal aneurysms.1)2) One hundred seventy-seven patients underwent stent-graft implantation for aorto-iliac aneurysms in our hospital from August 2005 to July 2009. Among them, only 11 patients had an isolated IAA. The CIA is the most common site for IAAs, followed by the IIA. The external iliac artery (EIA) is seldom affected.2)5)
Most IAAs are asymptomatic. Consequently, most IAAs are usually discovered incidentally during CT scan or angiography performed for other purposes. However, some patients may present with specific symptoms due to rupture, local compression, thrombosis, or distal embolization.6) Aneurysm rupture is the most hazardous among the many complications. For aneurysms between 3 to 4 cm in diameter, the risk of rupture is 5% to 9% over 5 years.7) For aneurysms >4 cm in diameter, the risk of rupture is 10% to 70% over 5 years. Rupture mortality is 25% to 57%.2)8)
Conventional surgical repair is considered the classical treatment for IAAs >3 cm in diameter. Elective surgical repair of IAAs has even a higher mortality rate than that of AAAs, ranging from 5% to 11%, while for emergency ruptures the mortality rate increases to 40% to 50%.2)8)9)
In recent years, with the development of stent-grafts, endovascular repair of IAAs has emerged as an attractive alternative to open surgical repair. This has clearly been shown to decrease patient discomfort, operative morbidity, hospital stay, and recovery time.10)11) Endovascular repair of isolated IAAs is a minimally invasive, safe and feasible technique and provides good short-term patency, especially in patients at high surgical risk.12)13) Performed by using a combination of IIA embolization and stent-grafting, this technique reduces periprocedural morbidity and mortality.6)
Our first patient had renal cell carcinoma and a history of a previous open abdominal surgery and a second open surgery would not be easy due to intra-abdominal adhesions. Furthermore, the patient was reluctant to undergo surgery. Our second patient had prostate cancer and was considered to be at high surgical risk due to his very old age. Consequently, endovascular exclusion was chosen as an alternative option over open surgical repair in both cases. Recently, the frequency of AAAs or IAAs discovered incidentally during a screening CT scan performed for evaluation of malignancy has increased. Endovascular repair using stent-grafts might be a good alternative treatment, especially in patients with old age, a history of previous open surgery, or high surgical risk.
When IAAs have adequate proximal and distal aneurysm necks, the endoluminal exclusion of IAAs is both feasible and effective. The covered tube stent-graft is able to be simply deployed across the IAA for exclusion, preserving the IIA. The endovascular approach with this technique is not always feasible because there may be a short landing zone between the aneurysm and the aorto-iliac bifurcation.
To overcome the anatomical problem of a short proximal neck, we performed endovascular bifurcated aorto-iliac stent grafting. Bifurcated stent-grafts are required in the absence of an adequate proximal landing zone. Experience has accumulated in the management of combined AAA and common IAAs with bifurcated grafts,14)15) but less is known about the application of endografts in isolated IAAs. The benefits from decreased morbidity and mortality of endovascular exclusion of isolated IAAs using a bifurcated stent-graft outweigh the minor complications associated with this technique.
Percutaneous femoral arterial access was obtained in our cases. Surgical cut-down of one or both common femoral arteries has usually been performed for vascular access because aorto-iliac stent-grafts require use of large-bore sheaths. Surgical cut-down is invasive and increases the risk of complications. Recently, several non-surgical methods for femoral artery access and closure have been reported including the development of arterial closure devices.16) Percutaneous suture devices for closure decrease patient discomfort, time to ambulation, and hospital stay length.
In both of our cases, primary technical success with complete exclusion of the aneurysmal lesion was achieved. The aneurysm diameter did not increased in any subject, according to measurements made on follow-up CT. IAA ruptures were not observed during follow-up, nor was any serious complications. In conclusion, endovascular repair of isolated IAAs with short proximal necks using bifurcated endografts is an efficient, feasible and relatively safe treatment option.
Figures and Tables
Fig. 1
A 54-year-old man with renal cell carcinoma. A and C: preprocedural computed tomography and angiography show a 39-mm right common iliac artery aneurysm, which is partially thrombosed (arrows). B and D: postprocedural computed tomography and angiography show the complete exclusion of the aneurysm and accurate positioning of endografts.
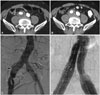
Fig. 2
An 80-year-old man with prostate cancer. A and C: preprocedural computed tomography reconstruction and angiography reveal a 50-mm huge left common iliac artery aneurysm with a short proximal neck (*). B and D: postprocedural computed tomography reconstruction and angiography reveal that bifurcated stent-grafts are patent and aneurysm exclusion is successful with no signs of endoleak or graft migration.
References
1. Brunkwall J, Hauksson H, Bengtsson H, Bergqvist D, Takolander R, Bergentz SE. Solitary aneurysms of the iliac arterial system: an estimate of their frequency of occurrence. J Vasc Surg. 1989. 10:381–384.
2. Richardson JW, Greenfield LJ. Natural history and management of iliac aneurysms. J Vasc Surg. 1988. 8:165–171.
3. Bolin T, Lund K, Skau T. Isolated aneurysms of the iliac artery: what are the chances of rupture? Eur J Vasc Surg. 1988. 2:213–215.
4. Kasirajan V, Hertzer NR, Beven EG, O'Hara PJ, Krajewski LP, Sullivan TM. Management of isolated common iliac aneurysms. Cardiovasc Surg. 1998. 6:171–177.
5. Cardon JM, Cardon A, Joueux A, Vidal V, Noblet D. Endovascular repair of iliac artery aneurysm with endoprosystem I: a multicentric French study. J Cardiovasc Surg. 1996. 37:3 Suppl 1. 45–50.
6. Boules TN, Selzer F, Stanziale SF, et al. Endovascular management of isolated iliac artery aneurysms. J Vasc Surg. 2006. 44:29–37.
7. Lowry SF, Kraft RO. Isolated aneurysm of the iliac artery. Arch Surg. 1978. 113:1289–1293.
8. McCready RA, Paizolero PC, Gilmore JC, Kazmier FJ, Cherry KJ Jr, Hollier LH. Isolated iliac artery aneurysm. Surgery. 1983. 93:688–693.
9. van Sambeek MR, van Urk H. Endovascular treatment of isolated iliac artery aneurysms. Eur J Vasc Endovasc Surg. 1998. 15:91–92.
10. Shim WH, Choi D, Yoon YS, Lee DY, Jang BC. Bifurcated stent-graft (vanguard) for the endovascular treatment of abdominal aortic aneurysm. Korean Circ J. 1999. 29:907–912.
11. Kim BK, Park S, Ko YG, et al. Immediate and mid-term outcomes of the endovascular stent-graft treatment of abdominal aortic aneurysm. Korean Circ J. 2005. 35:583–590.
12. Dorros G, Cohn JM, Jaff MR. Percutaneous endovascular stent-graft repair of iliac artery aneurysms. J Endovasc Surg. 1997. 4:370–375.
13. Marin ML, Veith FJ, Lyon RT, Cynamon J, Sanchez LA. Transfemoral endovascular repair of iliac artery aneurysms. Am J Surg. 1995. 170:179–182.
14. Ziegler P, Avgerinos ED, Umscheid T, Perdikides T, Erz K, Stelter WJ. Branched iliac bifurcation: 6 years experience with endovascular preservation of internal iliac artery flow. J Vasc Surg. 2007. 46:204–210.
15. Yano OJ, Morrissey N, Eisen L, et al. Intentional internal iliac artery occlusion to facilitate endovascular repair of aortoiliac aneurysms. J Vasc Surg. 2001. 34:204–211.
16. Shim CY, Park S, Ko YG, Choi D, Jang Y, Shim WH. Percutaneous closure of femoral artery access sites in endovascular stent-graft treatment of aortic disease. Int J Cardiol. 2008. 130:251–254.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download