Abstract
Sudden death (SD) in children is rarer than in adults. In the pediatric population, SD accounts for less than one tenth of deaths from all causes. SD in infants is a separate entity commonly termed "sudden infant death syndrome (SIDS)". Previous studies on SD in pediatric patients primarily focused on infants and showed that the incidence of SIDS was much lower in Asian countries than in Western ones. However, these differences diminished after educational campaigns such as the back to sleep act in the late 1980s to early 1990s. The incidence of SIDS from Western reports has decreased from 2.69 to around 0.5-0.24 per 1,000 live births. Beyond infancy, the annual incidence of SD ranges from 1.3 to 7.5 per 100,000. In 2009, two population-based studies, one from Taiwan and the other from the US, explored the epidemiological profile of SD in children. The child health care indexes of these two countries are similar, but the annual incidence of pediatric SD was 7.5 and 2.7 per 100,000 in the USA and Taiwan, respectively. The implications of ethic-related differences requires further confirmation. Around 40% of pediatric SD could be from cardiac causes, either diagnosed or undiagnosed. Risk stratification for cardiac SD and patient selection for implantable cardioverter-defibrillator (ICD) therapy are recommended. However, the adoption of ICD as primary prevention for SD in children is still a challenging issue. Early detection of undiagnosed cardiac risk may be facilitated by cardiac screening either in newborns or the school-age population to better manage the risk of SD. However, the efficacy of such screening remains still controversial.
Sudden death (SD) is rarer in pediatric populations than adults. Less than 10% of pediatric deaths are sudden, and the age-specific risk for SD is around 1:16,000 to 1:140,000.1-6) SD in infants is a distinct clinical entity and commonly grouped as "Sudden infant death syndrome (SIDS)". The rarity of the disease makes studies difficult, particularly in Asian populations, where the incidence is even lower.
In the West, the annual incidence of SD is 1.3-7.5 per 100,000 in the pediatric population beyond infancy,1-4)6) which are less than 10% of rates in adults.7-9) The annual incidence of SD in the general population is 1 in 1,000, a conservative estimate that does not account for unwitnessed events. Around 4% of SD in adults is unexplained, with no discernible abnormalities on histopathology and a negative toxicology screen. Termed "sudden arrhythmic death syndrome", some may be due to inherited cardiac arrhythmia syndrome from channelopathy.10) Similar SD may account for most SD in the pediatric population without structural cardiac diseases.
In an early study by Driscoll and Edwards,3) there were 12 SDs in the population aged 1-22 years from 1950 to 1982, giving an annual incidence of 1.3 per 100,000. Wren et al.1) reported an annual incidence of SD of 3.3 per 100,000 in the population aged 1-20 years in the Northern Health Region of England from 1985 to1994. In the study by Neuspiel and Kuller4) the annual incidence of SD was 4.6 per 100,000 in the population aged 1-20 years. In a recent report from Oregon (population 660,486), the pediatric SD constituted only 2.8% of all SD of the population, and the annual incidence of SD per 100,000 children (0-17 years) was 7.5 {95% confidence interval (CI) 5.1-10.5}, compared with 60/100,000 for all ages.6) In Asian populations, such data are still limited. Our study, based on the Taiwan National Health Insurance Database 2000-2006, revealed that in Taiwan (the average pediatric population 0-18 years was 5.44 million), the annual SD rate was 2.7 (95% CI: 2.6-2.9) per 100,000 in the population aged 1-18 years.5) In another study from Japan, in school age children, the annual incidence of SD was estimated as 6.4 per 100,000.11)
The incidence of SIDS is lower in Asian populations than in the West,12-21) but rates are declining in most Western countries.12-15)22) Educational campaigns in the late 1980s to early 1990s, such as the "back to sleep" act, have decreased the incidence of SIDS from 2.69 to around 0.5-0.24 per 1,000 live births.12-15)22) In Asian countries, most parents adopt a traditional "back to sleep" posture for infants, which could lead to low SIDS rates.
An international comparison of child health care indexes (newborn, infant, under-5, and 1-18 years population mortality), SIDS incidence, and SD in the pediatric population beyond infancy in 2005 were similar in most countries (Table 1). However, the infant, newborn, and under-five mortalities are relatively low for Japan, Norway, and Sweden, as was SIDS. SIDS rates best correlated to infant mortality (p=0.030), borderline to the newborn mortality (p=0.079), and not to postneonatal mortality (p= 0.119) or under-five mortality (p=0.238).
Limited data on SD incidence beyond infancy made an association between the incidence of SD and child health care indexes difficult to ascertain, with rates ranging from 1.3 to 7.5 per 100,000 person-years. Two studies in 2009 showed an annual SD incidence in non-infant pediatrics of 7.5 (2002-5) and 2.7 (2000-6), with all-cause rates of 32.7 (2004) and 33.2 (2000-6), in the United States and Taiwan, respectively.5)6) The proportion of SD to all-cause mortality was 22.9% for USA and 8.1% for Taiwan.5)6) Further work is needed to confirm these differences in the rates of SD to overall mortality.
We previously showed that the age-specific SD rate paralleled the all-cause mortality rate, with a nadir around early puberty (8-13 years).5) The proportionate SD mortality ratio ranged from 1.8% to 12.0% (8.9±2.2%), with the lowest rate in 11 to 12-year-olds. The proportionate SD mortality ratio in infants (6.2%) was not significantly higher than other age groups.
SD may occur in cardiac diseases such as 1) diagnosed cardiac diseases with risk of SD, such as repaired tetralogy of Fallot, transposition of the great arteries after atrial switch operation, Eisenmenger complex, Marfan syndrome, etc, 2) undiagnosed disease, mainly hypertrophic cardiomyopathy, primary cardiac arrhythmias {Wolff-Parkinson-White (WPW) syndrome, long QT syndrome (LQTS), catecholinergic polymorphic ventricular tachycardia, Brugada syndrome, short QT syndrome and arrhythmogenic right ventricular dysplasia}, and 3) acquired cardiac illness, such as myocarditis, commotio cordis, cocaine intoxication, etc.23-27) Around 40% of SD may be due to underlying cardiac diseases.27)
Patients with repaired congenital heart disease (CHD) have an SD risk during late follow-up. The risk of late SD increased incrementally 20 years after surgery for tetralogy of Fallot, aortic stenosis, and coarctation. In repaired CHD patients, the risk of nonsudden cardiac death was 1.6 per 1,000 patient-years, the risk of SD was 0.9 per 1,000 patient-years.28) The risk of SD was higher than non-sudden cardiac death for aortic stenosis and tetralogy of Fallot. Patients should undergo risk stratification for SD and consider elective implantable cardioverter-defibrillator (ICD) implantation after repaired tetralogy of Fallot.29-32) The role of electrophysiology studies to identify high risk patients has also been documented.30) Non-invasive screening parameters, such as QRS duration, QTc interval, and QTc and JTc dispersion from a 12-lead electrocardiogram are useful predictors of SD.31)
Among adults with CHD, including unrepaired CHD, the incidence of SD is 5.3 per 1,000 patient-years.33) The most common disease entities in SD were Eisenmenger complex, tetralogy of Fallot, and transposition of the great arteries. SD accounts for the highest proportion of death in coarctation of the aorta, Ebstein's anomaly, and transposition of great arteries. Most SD was found in the tetralogy of Fallot because of the patient population is relatively large. In a Japanese cohort of 253 patients from 15 institutions, 23 (9%) patients died at 29 (18-54) years of age and SD occurred in 6 (2.3%) patients, mainly in those with pulmonary vascular diseases.34) In another long-term follow up study of 167 patients who received total repair between 1965 and 1975 at a median age of 6 years, SD occurred in 7 (4%) patients.35) In Asians, we have demonstrated that the incidence of tetralogy of Fallot is higher than in Western countries.36) With advances in cardiac interventions, most of these patients may survive into adulthood. Long-term management of these patients, including the risk stratification and prevention for SD, will be a very important issue.
Hypertrophic cardiomyopathy is the most important cause of SD in young athletes. In a study of 99 children with hypertrophic cardiomyopathy, the reported annual incidence of SD and cardiac arrest was 2.7% between the age of 8 and 18 years.37) The risk factors included a family history of SD from hypertrophic cardiomyopathy, recurrent syncope, non-sustained ventricular tachycardia on an ambulatory electrocardiography (ECG), and extreme left ventricular hypertrophy.37)38) In a previous study from Finland, the risk of SD from previously unsuspected hypertrophic cardiomyopathy is low, with an age-specific risk in apparently normal children or adolescents of less than 1 in 1,000,000 per year.39)
Most patients with primary cardiac arrhythmias have undiagnosed cardiac diseases that account for unexplained SD. Some primary cardiac arrhythmias may be detected early by cardiac screening.40-44) For example; WPW syndrome and long-QT syndrome can be identified in schools during an electrocardiogram screening, but risk stratification for asymptomatic children with ECG abnormalities remains challenging.40)
SD in patients with WPW syndrome occurs after the development of atrial fibrillation that conducts though an accessory pathway with a very short refractory period and degenerates into ventricular fibrillation.45) SD in WPW patients ranges from 0.09% to 0.6% per patient year of follow-up.46)47) SD mainly occurs in adolescents and adults and rarely in childhood. Therefore, radiofrequency transcatheter ablation is recommended for symptomatic patients at the appropriate ages,47) and observation for asymptomatic patients.
The incidence of LQTS is 1:20,000 to 1:5,000.48)49) Using ECG-guided identification of disease-causing mutations, the prevalence of LQTS in apparently healthy live births was around 1:2,534 (95% CI, 1:1,583 to 1: 4,350).50) Most of the mutations were in KCNQ1 (LQT1), KCNH2 (LQT2), and SCN5A (LQT3) genes. The risk of SD in LQTS is associated with the gender, extent of QT prolongation, and underlying channelopathy. The latest report from the International LQTS Registry showed that LQTS boys experience a significantly higher rate of fatal or near-fatal cardiac events than girls during childhood.50) A QTc duration >500 ms and a history of prior syncope identify risk in boys, whereas a history of prior syncope is the only significant risk factor among girls. Beta-blocker therapy may decrease the risk of life-threatening cardiac events during childhood. Therefore, ICD implantation is only recommended for patients with recurrent syncope despite drug therapy, sustained ventricular arrhythmias, or averted SD.51) A strong family history of SD or compliance and intolerance issues may also prompt ICD implantation.51)
SD from life-threatening arrhythmias can potentially be prevented by ICD, on either a primary or secondary prevention basis.51)52) While ICD implantation is recommended for those with prior averted SD, ventricular arrhythmias, and syncope, ICD as primary SD prevention in high-risk children remains controversial. Risk stratification of cardiac disease and SD risk is often made according to electrophysiological data and hemodynamic abnormalities, but no parameter has satisfactory positive and negative predictive values for predicting SD. Therefore, ICD therapy is limited to secondary prevention of ventricular arrhythmias, syncope, and after SD.
Undiagnosed cardiac disease may be detected by screening with a detailed history, physical examination, and electrocardiogram. Disease-specific management and education may reduce SD probability, but the timing for invasive management, including electrophysiological studies, disease specific interventions, and ICD remains challenging. In children, the problem of inappropriate shock at follow-up adds further controversy to ICD implantation.
In conclusion, SD in children is rarer than adults and accounts for less than one tenth of all deaths in children. Ethnic differences in SIDS incidence have decreased after educational campaigns in the West. Two recent studies still indicate ethnic differences in SD incidence beyond infancy. Risk stratification for cardiac disease and early detection of undiagnosed disease may identify children with a high risk of SD. Subsequent disease-specific management may reduce the risk of SD. The role of ICD, particularly in the primary prevention of SD, remains a challenging issue in the pediatric population.
Figures and Tables
Table 1
International comparison of the mortality relevant to child health care indexes and the incidence of sudden death in infants (SIDS) and sudden death in 2005 and in pediatric population beyond infancy
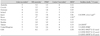
Data of infant and under-five mortality are obtained from Unicef website (http://www.unicef.org). *Per 1,000 live births, †Per 100,000 person-years, ‡2004. NB mortality: newborn mortality, PNM: postneonatal mortality
References
1. Wren C, O'Sullivan JJ, Wright C. Sudden death in children and adolescents. Heart. 2000. 83:410–413.
2. Molander N. Sudden natural death in later childhood and adolescence. Arch Dis Child. 1982. 57:572–576.
3. Driscoll DJ, Edwards WD. Sudden unexpected death in children and adolescents. J Am Coll Cardiol. 1985. 5:6 Suppl. 118B–121B.
4. Neuspiel DR, Kuller LH. Sudden and unexpected natural death in childhood and adolescence. JAMA. 1985. 254:1321–1325.
5. Wu MH, Wu MH, Chen HC, Wang JK, Huang SC, Huang SK. Population-based study of pediatric sudden death in Taiwan. J Pediatr. 2009. 155:870–874.e2.
6. Chugh SS, Reinier K, Balaji S, et al. Population-based analysis of sudden death in children: the Oregon sudden unexpected death study. Heart Rhythm. 2009. 6:1618–1622.
7. Priori SG, Aliot E, Blomstrom-Lundqvist C, et al. Task Force on Sudden Cardiac Death of the European Society of Cardiology. Eur Heart J. 2001. 22:1374–1450.
8. Zheng ZJ, Croft JB, Giles WH, Mensah GA. Sudden cardiac death in the United States, 1989 to 1998. Circulation. 2001. 104:2158–2163.
9. Straus SM, Bleumink GS, Dieleman JP, van der Lei J, Stricker BH, Sturkenboom MC. The incidence of sudden cardiac death in the general population. J Clin Epidemiol. 2004. 57:98–102.
10. Behr ER, Casey A, Sheppard M, et al. Sudden arrhythmic death syndrome: a national survey of sudden unexplained cardiac death. Heart. 2007. 93:601–605.
11. Niimura I, Maki T. Sudden cardiac death in childhood. Jpn Circ J. 1989. 53:1571–1580.
12. Adams EJ, Chavez GF, Steen D, Shah R, Ivasu S, Krous HF. Changes in the epidemiologic profile of sudden infant death syndrome as rates decline among California infants: 1990-1995. Pediatrics. 1998. 102:1445–1451.
13. Daltveit AK, Øyen N, Skjærven R, Irgens LM. The epidemic of SIDS in Norway 1967-93: changing effects of risk factors. Arch Dis Child. 1997. 77:23–27.
14. Arnestad M, Andersen M, Vege A, Rognum TO. Changes in the epidemiological pattern of sudden infant death syndrome in southeast Norway, 1984-1998: implications for future prevention and research. Arch Dis Child. 2001. 85:108–115.
15. Moon RY, Horne RS, Hauck FR. Sudden infant death syndrome. Lancet. 2007. 370:1578–1587.
16. Sawaguchi T, Nelson EA, Fujita T, Sawaguchi A, Knight B. Is the incidence of SIDS increasing in Asia? Int J Legal Med. 1998. 111:278–280.
17. Lee CL, Chang TL. The trend of sudden infant death syndrome in Taiwan from 1984 to 1993. Zhonghua Min Guo Xiao Er Ke Yi Xue Hui Za Zhi. 1995. 36:431–433.
18. Sawaguchi T, Namiki M. Recent trend of the incidence of sudden infant death syndrome in Japan. Early Hum Dev. 2003. 75:Suppl. S175–S179.
19. Ha M, Yoon SJ, Lee HY, Goh UY, Kim CH, Lee YS. Estimation of the incidence of sudden infant death syndrome in Korea: using the capture-recapture method. Paediatr Perinat Epidemiol. 2004. 18:138–142.
20. Lee NN, Chan YF, Davies DP, Lau E, Yip DC. Sudden infant death syndrome in Hong Kong: confirmation of low incidence. BMJ. 1989. 298:721.
21. Knöbel HH, Yang WS, Chen CJ. Sudden infant death syndrome among Chinese. Lancet. 1994. 344:820.
22. Hauck FR, Tanabe KO. International trends in sudden infant death syndrome: stabilization of rates requires further action. Pediatrics. 2008. 122:660–666.
23. Morentin B, Aguilera B, Garamendi PM, Suarez-Mier MP. Sudden unexpected non-violent death between 1 and 19 years in north Spain. Arch Dis Child. 2000. 82:456–461.
24. Maron BJ, Shirani J, Poliac LC, Matenge R, Roberts WC, Mueller FO. Sudden death in young competitive athletes: clinical, demographic, and pathological profiles. JAMA. 1996. 276:199–204.
25. Keeling JW, Knowles SA. Sudden death in childhood and adolescence. J Pathol. 1989. 159:221–224.
26. Liberthson RR. Sudden death from cardiac causes in children and young adults. N Engl J Med. 1996. 334:1039–1044.
27. Wren C. Sudden death in children and adolescents. Heart. 2002. 88:426–431.
28. Silka MJ, Hardy BG, Menashe VD, Morris CD. A population-based prospective evaluation of risk of sudden cardiac death after operation for common congenital heart defects. J Am Coll Cardiol. 1998. 32:245–251.
29. Khairy P, Harris L, Landzberg MJ, et al. Implantable cardioverter-defibrillators in tetralogy of Fallot. Circulation. 2008. 117:363–370.
30. Khairy P, Landzberg MJ, Gatzoulis MA, et al. Value of programmed ventricular stimulation after tetralogy of Fallot repair: a multicenter study. Circulation. 2004. 109:1994–2000.
31. Kugler JD. Predicting sudden death in patients who have undergone tetralogy of Fallot repair: is it really as simple as measuring ECG intervals? J Cardiovasc Electrophysiol. 1998. 9:103–106.
32. Silka MJ, Kron J, Dunnigan A, Dick M 2nd. The Pediatric Electrophysiology Society. Sudden cardiac death and the use of implantable cardioverter-defibrillators in pediatric patients. Circulation. 1993. 87:800–807.
33. Harrison DA, Connelly M, Harris L, Luk C, Webb GD, McLaughlin PR. Sudden cardiac death in the adult congenital heart disease. Can J Cardiol. 1996. 12:1161–1163.
34. Sakazaki H, Niwa K, Echigo S, Akagi T, Nakazawa M. Predictive factors for long-term prognosis in adults with cyanotic congenital heart disease: Japanese multi-center study. Int J Cardiol. 2007. 120:72–78.
35. Hamada H, Terai M, Jibiki T, Nakamura T, Gatzoulis MA, Niwa K. Influence of early repair of tetralogy of Fallot without an outflow patch on late arrhythmias and sudden death: a 27-year follow-up study following a uniform surgical approach. Cardiol Young. 2002. 12:345–351.
36. Wu MH, Chen HC, Lu CW, Wang JK, Huang SC, Huang SK. Prevalence of congenital heart disease at live birth in Taiwan. J Pediatr. 2010. [Epub ahead of print].
37. Yetman AT, Hamilton RM, Benson LN, McCrindle BW. Long-term outcome and prognostic determinants in children with hypertrophic cardiomyopathy. J Am Coll Cardiol. 1998. 32:1943–1950.
38. Elliot P, Poloniecki J, Dickie S, et al. Sudden death in hypertrophic cardiomyopathy: identification of high risk patients. J Am Coll Cardiol. 2000. 36:2212–2218.
39. Arola A, Jokinen E, Ruuskanen O, et al. Epidemiology of idiopathic cardiomyopathies in children and adolescents: a nationwide study in Finland. Am J Epidemiol. 1997. 146:385–393.
40. Chiu SN, Wang JK, Wu MH, et al. Cardiac conduction disturbance detected in a pediatric population. J Pediatr. 2008. 152:85–89.
41. Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980-2006. Circulation. 2009. 119:1085–1092.
42. Vetter VL. The role of ECG screening in the evaluation of risk of sudden cardiac arrest in the young. Pacing Clin Electrophysiol. 2009. 32:Suppl 2. S6–S14.
43. Myerburg RJ, Vetter VL. Electrocardiograms should be included in preparticipation screening of athletes. Circulation. 2007. 116:2616–2626.
44. Chaitman BR. An electrocardiogram should not be included in routine preparticipation screening of young athletes. Circulation. 2007. 116:2610–2614.
45. Montoya PT, Brugada P, Smeets J, et al. Ventricular fibrillation in the Wolff-Parkinson-White syndrome. Eur Heart J. 1991. 12:144–150.
46. Munger TM, Packer DL, Hammill SC, et al. A population study of the natural history of Wolff-Parkinson-White syndrome in Olmsted County, Minnesota, 1953-1989. Circulation. 1993. 87:866–873.
47. Friedman RA, Walsh EP, Silka MJ, et al. NASPE Expert Consensus Conference: radiofrequency catheter ablation in children with and without congenital heart disease. Report of the writing committee. North American Society of Pacing and Electrophysiology. Pacing Clin Electrophysiol. 2002. 25:1000–1017.
48. Goldenberg I, Moss AJ. Long QT syndrome. J Am Coll Cardiol. 2008. 51:2291–2300.
49. Schwartz PJ, Stramba-Badiale M, Crotti L, et al. Prevalence of the congenital Long-QT syndrome. Circulation. 2009. 120:1761–1767.
50. Goldenberg I, Moss AJ, Peterson DR, et al. Risk factors for aborted cardiac arrest and sudden cardiac death in children with the congenital long-QT syndrome. Circulation. 2008. 117:2184–2191.
51. Epstein AE, DiMarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities. J Am Coll Cardiol. 2008. 51:e1–e62.
52. Berul CI, Van Hare GF, Kertesz NJ, et al. Results of a multicenter retrospective implantable Cardioverter-defibrillator registry of pediatric and congenital heart disease patients. J Am Coll Cardiol. 2008. 51:1685–1691.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download