Introduction
After the drug eluting stent (DES) was invented, the incidence of in-stent restenosis (ISR) was significantly reduced, while stent thrombosis (ST) remained a serious complication of intracoronary stent implantation. Unlike restenosis, ST is rare, but, once developed, almost one-third to one-half of all occurrences result in death.1) ST can develop immediately or late (over one year after the stent implantation).2) Although the mechanism is not fully understood, incomplete neointimal coverage over stent struts is thought to play a role in ST.3)
Case
A 70-year-old woman visited the emergency room with typical chest pain. She had undergone mastectomy for left breast cancer 30 years earlier and had hypertension and diabetes mellitus for 10 years. The electrocardiogram (ECG) showed ST segment elevation of 1 mm and Q waves in the II, III, and aVF leads. Chest radiography and 2-D echocardiography showed mild pulmonary congestion and a regional wall motion abnormality in the inferior wall. Serum troponin I and creatine kinase-MB (CK-MB) levels were 0.69 ng/mL and 60.1 ng/mL, respectively.
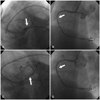
Aspirin (200 mg) and clopidogrel (300 mg) were administered before emergency coronary angiography, and low molecular weight heparin was administered subcutaneously. Critical stenosis at the proximal segment of the right coronary artery (RCA) was noted with Thrombolysis in Myocardial Infarction (TIMI) 3 flow, and severe stenosis in the proximal segment of the left anterior descending coronary artery (LAD) was observed (Fig. 1A and B).
An Endeavor stent (Medtronic Europe SA, 2.75×30 mm) was implanted in the infarct-related RCA after pre-dilatation (2.0×30 mm, 10 atm over 10 seconds) without acute complication. As the patient was hemodynamically stable and chest pain was resolved, subsequent intervention for the LAD stenosis was chosen. Another Endeavor stent (2.75×14 mm) was implanted after pre-dilatation (2.5×20 mm, 9 atm over 10 seconds) in the proximal segment of the LAD. During the procedure, the patient's vital signs were stable and the chest pain disappeared (Fig. 1C and D). She was transferred to the general ward after careful observation in the intensive coronary care unit. Aspirin (100 mg) and clopidogrel (75 mg) were administered daily after stent implantation.
On the sixth day after stent implantation, sudden ventricular tachycardia followed by ventricular fibrillation developed along with chest pain and dyspnea. The patient received advanced cardiac life support, the administration of low molecular weight heparin was resumed, and emergency coronary angiography was performed under the tentative diagnosis of subacute ST (Fig. 2A and B).
Coronary angiography showed total occlusion of the previously implanted stents at both the proximal LAD and RCA segments despite the appropriate dual anti-platelet treatment.
Before revascularization, a temporary pacemaker and an intra-aortic balloon pulsation (IABP) catheter were inserted. The LAD was re-canalized with simple balloon dilatation and the RCA was subsequently re-canalized. Successful revascularization was achieved and blood flow resumed to TIMI 3 in both arteries. After she was transferred to the intensive coronary care unit, vital signs were stabilized and the IABP was removed the following day. The dose of aspirin and clopidogrel was not increased but cilostazol (100 mg bid) was added after ST. Because acute renal failure developed and the respiratory support with mechanical ventilation was prolonged, her discharge was delayed for two months but she was without further ischemic events.
Discussion
Sirolimus and paclitaxel have been the most widely used coating agents on DESs, and the new zotarolimuseluting stent (ZES) was developed with favorable safety and efficacy for inhibiting neointimal hyperplasia compared to bare metal stents in early trials.4)5)
Since commercial availability of the new DESs, a few cases of ZES thrombosis have been reported.6)7) Moreover, simultaneous subacute multi-vessel ST of ZES stents despite the administration of a substantial number of anti-platelet agents is very rare.8)9)
According to a randomized, controlled study with sirolimus eluting stents, the predictors for ST are advanced age, premature anti-platelet discontinuation, clopidogrel resistance, insulin-dependent diabetes, acute coronary syndrome, low ejection fraction, moderate or heavy calcification, multivessel disease, post procedural TIMI <3, and a totally occluded lesion as the first manifestation.10) The patient in this report was an elderly person with type 2 diabetes mellitus, presenting with acute coronary syndrome.
We pre-dilated stenotic lesions and carefully measured reference diameters of the arteries before the selection of appropriate stents. Post-dilatation with a stent balloon was performed to avoid under-dilatation or malapposition. Therefore, we believe that simultaneous thrombosis of different arteries suggest a systemic, rather than a local cause. A potential cause of these fatal events was the incomplete coverage of anti-platelet agents for systemic thrombogenicity such as improper dosage or resistance to the anti-platelet agents. A previous report showed that up to 25% of patients with myocardial infarction associated with ST-segment elevation were resistant to clopidogrel.11) Unfortunately, we could not ascertain the resistance to aspirin or clopidogrel in our patient because the test was unavailable by the time of the adverse event and the patient was not compliant later on.
In summary, we experienced a case of very rare multivessel ST of a ZESs and expect this problem to be solved as more experience with ZESs accumulate.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download