Abstract
Background and Objectives
Although coronary artery obstruction, aortic insufficiency (AI), and pulmonary stenosis (PS) have been reported after arterial switch operation (ASO), limited long-term studies on ASO exist. Our study aimed to examine long-term outcomes after ASO for simple complete transposition of the great arteries (TGA).
Subjects and Methods
All 108 patients with simple complete TGA who underwent ASO at Seoul National University Children's Hospital between 1987 and 2004 were enrolled. We retrospectively reviewed the patients' medical records and the results of various functional and imaging studies.
Results
Among 108 cases of ASO for simple TGA, 96 have been followed-up through the present time (mean follow-up duration was 11.7±8.6 years: range= 4 to 23 years). The 20-year rates of freedom from significant AI, PS, and coronary obstruction were 78.6%, 67.8%, and 95.8%, respectively. AI showed a tendency to progress as follow-up time increased in 21.4% of the population studied (p=0.014); however, AS, PS, and PI showed no such progression. Late coronary artery occlusion was not associated with the initial coronary arterial pattern. Re-operations were done for 13 patients (13.5%) at an average of 8±4.3 years after ASO. The survival rate was 96%, while the re-operation-free was 90% at 10 years and 83% at 20 years. Most patients showed normal physical growth with good activity {98%; New York Heart Association (NYHA) class 1 activity} and normal development (96%).
Since the first successful arterial switch operation (ASO) in 1975 by Jatene et al.,1) ASO has become the treatment of choice for surgical correction of complete transposition of the great arteries (TGA). Compared with atrial switch procedures (Mustard or Senning operation), the ASO has some advantages, including preservation of the left ventricle as the systemic pumping chamber, maintenance of sinus node function, and employment of the mitral valve as the systemic atrioventricular valve.2)3) Recent results have been satisfactory, although it has been reported that various complications may occur, mainly coronary artery obstruction, aortic insufficiency (AI), and supravalvar pulmonary stenosis (PS).3) Although the earliest surviving ASO patients in South Korea are now entering their third decade of life, longterm follow-up studies (up to 20 years) are rare. The purpose of this study was to examine long-term outcomes after ASO for simple complete TGA.
We retrospectively reviewed all the patients with simple complete TGA who underwent ASO at Seoul National University Children's Hospital between January 1987 and December 2004. One-hundred eight patients were enrolled in this study. We included patients with atrial septal defect (ASD), ventricular septal defect (VSD), patent ductus arteriosus, and mild PS, but excluded patients with other complex anomalies such as coarctation of the aorta, interrupted aortic arch, pulmonary atresia, functional single ventricle, and mitral valve disease. The mean follow-up duration after ASO was 11.3±4.9 years (range: 4 to 23 years). Survival status was determined according to medical records or by contacting the patient's parents by telephone. We reviewed medical records and recent results of electrocardiograms (ECG), echocardiography, cardiac catheterization, myocardial single photon emission computed tomography (SPECT), and multi-slice computed tomography (MSCT).
Statistical Package for Social Science (SPSS) 16.0 for Windows (SPSS Inc., Chicago, IL, USA) was used for data analysis. The Kaplan-Meier estimator and log-rank test were used to calculate survival and re-operation-free rates. Pearson's chi-square test and linear-by-linear association method were applied to assess time trends for AI, aortic stenosis (AS), pulmonary insufficiency (PI), and PS. Cox's proportional hazards model and Fisher's exact test were employed to analyze risk factors associated with AI after ASO. For all analyses, a p of less than 0.05 was considered significant.
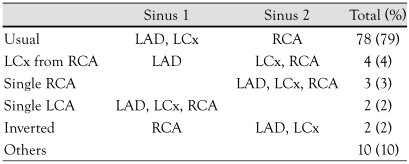
Of the 108 patients, 96 (88.9%) are still alive and have been followed-up through the time of this report. Another 8 patients (7.4%) were lost to follow-up, and 4 patients (3.7%) died in the hospital within 4 months of ASO because of cardiogenic shock due to coronary insufficiency or septic shock. The mean age at the time of this study was 11.7±8.6 years (range: 4-23 years). The majority of patients, 86 of 108, were males; 22 were females. Sixty-five (60.2%) patients did not have VSD. Balloon atrial septostomy (BAS) was performed on 65 patients (60.2%), with a median age of 4 days (range: 1-113 days). The median interval between BAS and ASO was 4 days (range: 1 day to 16 months). A total of 104 patients underwent one-stage ASO at a median age of 10.5 days (range: 2 days to 5 years); another 3 patients underwent staged ASO with palliative pulmonary artery banding (PAB) and a right modified Blalock-Taussig shunt, and 1 patient underwent a conversion ASO from a previous Senning operation. We were able to identify coronary artery patterns in 99 patients, and those data are summarized in Table 1. The usual coronary artery pattern was the most common (78 patients; 79%), followed by the left circumflex artery from the right coronary artery (4 patients; 4%).
We assessed valve complications by Doppler echocardiography and categorized them as none, trivial, mild, moderate, or severe. AI tends to progress with post-operative time (p=0.014) (Fig. 1A). However, AS, PI, and PS did not increase significantly during the follow-up period (Figs. 1B and 2). AI was progressive in 18 patients (21.4%); none or trivial to mild (time interval: 64±40 months) in 12 patients (14.3%); none or trivial to moderate (time interval: 16.5 years) in 1 patient (1.2%); mild to moderate (time interval: 57±32 months) in 4 patients (4.8%); and mild to severe (time interval: 13.3 years) in 1 patient (1.2%). Aortic valve replacement or aortic valvuloplasty was performed in 3 patients. Known risk factors for AI progression-prior PAB, presence of VSD, more advanced age at the time of ASO (1 month or more after birth), and size discrepancy between the aorta and the pulmonary artery-were not statistically significant in the present study. The 20-year rates of freedom from significant AI and PS were 78.6% and 67.8%, respectively (Fig. 3). PS was identified at the level of the main pulmonary artery (3 patients), at the more distal branches (1 patient), or at the pulmonic valve (2 patients). The 20-year rate of freedom from both significant PI and significant AS was 100%.
We performed cardiac catheterizations 65 times in 53 patients and found that 4 patients had coronary artery complications. Forty-nine patients showed intact coronary arteries. Three patients showed complete occlusion of the left coronary artery ostium (at 18, 78, and 97 months after ASO). Of the 3 cases of coronary obstruction, 1 case was detected by coronary angiography 1 year after ASO, another 8 years after ASO, and the last 6 years after ASO. The first case showed a high take-off pattern of left coronary artery. The ostium was completely occluded, and distal perfusion was observed through retrograde filling from the right coronary artery. Myocardial single photon emission computed tomography (SPECT) showed reversible perfusion defects in the apex and the anterior wall. The patient complained of intermittent chest discomfort during exercise. Fourteen years after the initial ASO, the patient underwent coronary angioplasty and subsequently was symptomfree. The second case showed severe narrowing of the left coronary artery via coronary angiography 1 year after ASO but was asymptomatic at that time. Eight years later, the patient complained of recurrent chest pain that became more severe and more frequent. Coronary angiography revealed complete occlusion of the left coronary ostium and intercoronary collateral perfusion from the right coronary artery. Left coronary ostial angioplasty was performed immediately. After the operation, the patient still had a persistent perfusion defect revealed by myocardial SPECT and complained of intermittent chest pain during exercise. However, a follow-up coronary angiography revealed a patent left coronary artery. In the third case, echocardiography showed an interventricular septal wall motion abnormality 1 year after ASO. This abnormality was progressive and was ultimately accompanied by severe ventricular systolic dysfunction. Coronary angiography performed 6 years after ASO showed complete occlusion of the left anterior descending artery ostium and retrograde flow from the left circumflex coronary artery to the distal left anterior descending artery. Because the patient was asymptomatic at that time, the patient remained on follow-up without revascularization and has been categorized as New York Heart Association (NYHA) class 1. Myocardial SPECT recently showed a reversible mild perfusion decrease in the apex and apical anteroseptal wall. Another patient with a hypoplastic left anterior descending coronary artery showed neither a perfusion defect nor chest pain.
Among 9 patients with chest pain or decreased systolic function, MSCT revealed intact coronary arteries in all patients. We also performed myocardial SPECT in 32 patients; 24 patients (75%) showed no perfusion defects, 7 (22%) showed reversible perfusion defects, and 1 (3%) showed a persistent perfusion defect. There was no significant correlation between the original coronary artery patterns and late coronary complications or death (p=0.131). Neither ECG during exercise nor 24-hour ECG revealed any significant arrhythmia, except premature ventricular or atrial complexes in 19 of 36 patients (52.8%) who underwent testing.
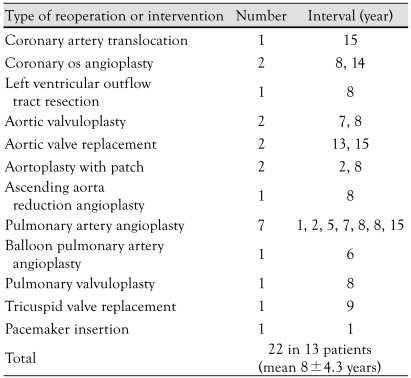
As shown in Table 2, a total of 22 re-operations or interventions were performed in 13 patients (13.5%), an average of 8±4.3 years after ASO. Ostial angioplasty of the left coronary artery was performed in 2 patients with complete occlusion of the left coronary artery ostia 8 and 14 years after ASO. Aortic valve replacement was performed in 2 patients with severe AI at 13 and 15 years, respectively, after ASO. As PS was the most frequent cause of re-operations or intervention, surgical or balloon pulmonary angioplasty was performed in 9 patients at an average of 6.6±3.9 years after ASO. One of the 9 required two re-operations for residual PS. The survival rate at 11.3±4.9 years post-ASO was 96%, and the re-operation-free rate was 96%, 90%, 87%, and 83% after 5, 10, 15, and 20 years of follow-up, respectively (Fig. 4).
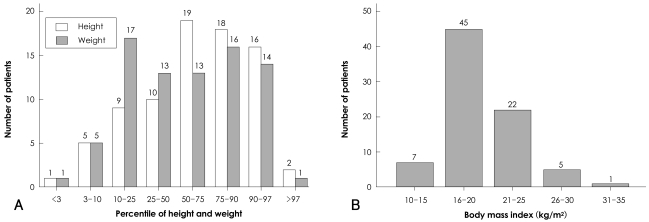
In this study group, 5 patients had neurological complications. One patient had quadriparesis due to preoperative hypoxia. Among the remaining 4 patients, whose neurological abnormalities were attributed to postoperative hypoxia, the manifestations were as follows: quadriparesis, spastic diplegia, left hemiplegia, and right finger movement impairment. In all, 86 patients (98%) belonged to NYHA functional class 1, and only 3 patients (2%) were placed in class 3 or 4. Most patients (98.8%) showed normal physical growth as in the general healthy population (Fig. 5), except one patient, diagnosed with failure to thrive, who had cerebral palsy and developmental delay due to postoperative hypoxic ischemic encephalopathy.
In this study, we observed that ASO provides satisfactory long-term results with an excellent survival rate, small rate of re-operation, negligible significant arrhythmia, and good physical growth and development. Despite these positive results, there remain some concerns with regard to coronary artery, AI, PS, and other complications.
AI is the most frequent valve complication in this study. 44% of enrolled patients showed some degree of AI, and 14% of patients had more than moderate AI. Several mechanisms were proposed to explain this. Operative procedures include transection of both great arteries above the sinotubular junction and transfer of the coronary arteries into the neo-aortic sinus. These procedures can result in a complex suture line, which not only changes the geometry of the neo-aortic sinus, but also causes distortion with somatic growth and a decrease in neo-aortic distensibility. Moreover, because the pulmonary valve is not designed to perform as the normal aortic valve, the excessive burden placed on the pulmonary valve in the systemic position can affect neoaortic valvar function, possibly leading to valvar incompetence over time. As in other studies, our study showed that the incidence and degree of AI progress over time. The development of AI is known to be related to more advanced age at the time of ASO, previous pulmonary artery banding, use of trap-door coronary reimplantation rather than the punch technique, size discrepancies between the aorta and the pulmonary artery, AI at discharge, and rapid development of aortic root dilatation.3-5) We evaluated the relationship between AI progression and risk factors, such as prior PAB, presence of VSD, older age at the time of ASO (1 month or more after birth), and aorta-pulmonary artery size discrepancy. In contrast to previous findings, however, we identified no risk factors for AI progression in the present study, which may be due to the small number of patients with significant AI.
PS was the most common cause of reoperation or intervention after ASO, as in previous studies.6-11) The mechanism of PS is not well known, but the long course of the pulmonary artery can be stretched with somatic growth due to frequent use of the LeCompte maneuver in TGA with the vessels located in an anterior-posterior relationship, and that may be one of the causes of PS. Stenosis at any level of the pulmonary artery is possible, but in our observations, it occurred mainly in the supravalvar area, in the branches or the main pulmonary artery. Previous studies have reported that significant PS was found in 10-30% patients.8)10)11) In recent work described by Jatene et al.,9) severe supravalvar PS (a mean gradient of >60 mmHg) was reported in 7.4% of his cases, and all patients underwent reoperation. We observed significant PS in 7.1% of patients who underwent reoperation or intervention.
In contrast, AS is rarely observed in long-term follow-up after ASO, which may be due to the lack of traction between the neo-aorta and the pulmonary trunk. Likewise, PI was seldom observed, which may be due to the lower shear force and tensile stress in the pulmonary circulatory system.
One of the most common and serious morbidities in long-term follow-up after ASO involves coronary artery complications such as coronary artery obstruction or stenosis. Earlier reports showed a prevalence varying from 2% to 11%.11-15) A recent retrospective study encompassing 1,198 patients by Legendre et al.16) showed frequent coronary artery complications, with a prevalence of 6.8%. In this study, coronary artery obstruction was observed in 3 patients (3.6%). The relatively lower prevalence of coronary complications in our study compared with previous studies is likely because we included only simple complete TGA and assessed the prevalence of coronary complications except for 2 cases of early mortality due to coronary insufficiency. Possible mechanisms for coronary artery obstruction include stretching of the coronary artery with somatic growth, fibrocellular intimal thickening, extrinsic compression, and anatomical kinking or torsion.17) A recent meta-analysis of 9 independent series,18) including a total of 1,942 patients, revealed that single coronary patterns and intramural coronary arteries were associated with significant mortality. However, neither intramural nor single coronary patterns were found in any patients with coronary obstructions that required revascularization, which may be due to the small number of patients included in this study.
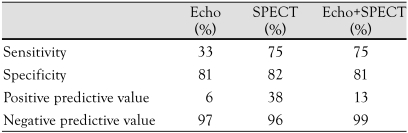
Coronary artery obstruction was an important cause of both early and late death in previous studies.3)12)19-21) However, accurate diagnosis of coronary lesions is challenging. Typical clinical signs of coronary dysfunction, such as chest pain or syncope, were not observed in most patients, as seen in other studies.17)19)20) Indeed, earlier studies revealed that severe coronary lesions, including stenosis, compression, and occlusion, occurred in 3-7.8% of symptom-free patients.17)22) With advancements in resolution and new techniques, echocardiography has become a valuable tool in detecting stenosis of the proximal and distal coronary arteries, as well as functional assessment through measurement of the coronary flow reserve. However, epicardial coronary artery evaluation is limited, and because of the poor window for anatomic assessments of coronary arteries in many cases, echocardiography plays only an additive role for coronary angiography.23) Myocardial SPECT is a widely used noninvasive method, although it is less sensitive than conventional angiography in detecting significant coronary lesions, because retrograde perfusion from collateral circulation may protect the myocardium.16) The sensitivity and specificity of echocardiography and myocardial SPECT for predicting coronary artery lesions were analyzed in this study, and we found that the sensitivity of myocardial SPECT was higher than that of echocardiography, reaching 75% (Table 3). Of 8 patients with perfusion defects shown by myocardial SPECT, 4 underwent coronary angiography. Three patients showed complete ostial occlusion of the left coronary artery, with a normal or false-positive result in 1 patient. Bengel et al.24) reported that coronary flow reserve measured by stress echocardiography or positron emission tomography was diminished in the absence of ischemic symptoms in children late after ASO.25) One possible reason for the discrepancies between the results of myocardial SPECT and coronary angiography in our data may be the decrease in coronary flow reserve. MSCT has recently been introduced as an innovative noninvasive technique for detecting coronary lesions. Because MSCT began in earnest at our institute in 2002, data were limited in this study. MSCT has the advantage of providing a better understanding of mechanisms behind coronary artery obstruction than conventional angiography, because it gives three-dimensional information about the abnormal course of the coronary artery between the great arteries. A recent study on MSCT showed that the technique accurately detected ostial and proximal segments of transferred coronary artery stenosis when compared to conventional angiography.26) However, MSCT has some limitations for the reliable assessment of coronary arteries. Image quality can be poor, especially when tachycardia or severe coronary calcification is present.27) Administration of additional beta-blockers prior to MSCT may improve image quality, but it is impossible to apply to all patients, especially those who have had decreased systolic function. Nonetheless, a recently developed 64-slice CT considerably overcame these limitations, but not completely. Another innovative method, intracoronary ultrasound, provides cross-sectional, transmural tomographic images of the coronary arteries and reflects vessel wall histology.28) This technique has been shown to be superior to conventional angiography in evaluating intimal wall thickening. Coronary angiography and intracoronary ultrasound are together the most sensitive and accurate methods for detecting various forms of coronary lesions, although they are invasive.
Though universal long-term follow-up guidelines are not available for ASO patients, coronary evaluation should be performed at regular intervals, utilizing both noninvasive and invasive methods, because only systematic evaluation can detect coronary lesions in their early stages and prevent sudden cardiac death due to coronary obstruction.
Recent evidence suggests that obesity is quite prevalent in patients with TGA.29) In this study group, 6 patients (7.5%) had an observed body mass index (BMI) of more than 25 and were classified as obese, and the prevalence of obesity was similar to that of the general pediatric population. Especially careful attention must be paid to these obese patients with vulnerable coronary arteries because of the potential for early atherosclerosis and abnormal coronary vascular reserve. The distribution of the NYHA class in the late follow-up period did not differ from that in another study, and most patients (98%) showed NYHA class 1 activity.11) Symptoms or wall motion abnormalities that suggest myocardial ischemia were inconsistent with NYHA functional class. Of 17 patients with an ejection fraction of less than 55% based on echocardiography, 16 (94.1%) belonged to NYHA class 1 and only 1 patient (5.9%) belonged to class 3. Therefore, we might conclude that NYHA classification is not sufficiently sensitive to identify patients with significant systolic dysfunction. All patients without preoperative or postoperative hypoxic damage achieved normal development. Preoperative hypoxia could be prevented through prenatal identification of patients with TGA. The high-risk coronary artery patterns that cause postoperative hypoxia due to immediate coronary obstruction are as follows: high take-off, para-commissural origin, tangential origin, intramural, and single coronary artery.18)30) Careful attention during surgery is required when treating such high-risk patients, especially when the coronary artery is transferred to minimize hypoxic damage and improve functional and neuro-developmental outcomes.
We acknowledge the following limitations of the present study: First, coronary artery evaluations, such as angiography, myocardial SPECT, and MSCT, were not performed in all patients, so we could not completely identify all the coronary artery complications. Second, we determined the re-operation-free rate and survival rate using only data from patients currently involved in follow-up. Therefore, the actual re-operation-free rate and survival rate may be less than the present study reports. Our results require further validation with more children undergoing ASO through a multi-institutional prospective study.
Based on the favorable long-term outcomes revealed in this study, ASO should be considered the treatment of choice for children with complete TGA, as previously reported. However, because some late complications, such as coronary artery obstruction and significant AI and PS, have been found after successful ASO, meticulous lifelong follow-up is mandatory in this patient group, and further studies will be required to ascertain long-term complications.
References
1. Jatene AD, Fontes VF, Paulista PP, et al. Successful anatomic correction of transposition of the great vessels: a preliminary report. Arq Bras Cardiol. 1975; 28:461–464. PMID: 1200893.
2. Kim YW. Follow-up study after atrial switch operation for complete transposition of the great arteries. Korean Circ J. 1998; 28:683–690.
3. Losay J, Touchot A, Serraf A, et al. Late outcome after arterial switch operation for transposition of the great arteries. Circulation. 2001; 104(12 Suppl 1):I121–I126. PMID: 11568042.
4. Losay J, Touchot A, Capderou A, et al. Aortic valve regurgitation after arterial switch operation for transposition of the great arteries: incidence, risk factors, and outcome. J Am Coll Cardiol. 2006; 47:2057–2062. PMID: 16697325.
5. Yoon MJ. Aortic insufficiency after arterial switch operation in transposition of the great arteries. Korean Circ J. 1998; 28:331–338.
6. Haas F, Wottke M, Poppert H, Meisner H. Long-term survival and functional follow-up in patients after the arterial switch operation. Ann Thorac Surg. 1999; 68:1692–1697. PMID: 10585044.
7. Hutter PA, Kreb DL, Mantel SF, Hitchcock JF, Meijboom EJ, Bennink GB. Twenty-five years' experience with the arterial switch operation. J Thorac Cardiovasc Surg. 2002; 124:790–797. PMID: 12324738.
8. Jatene FB, Bosisio IB, Jatene MB, Souza LC, Barbero-Marcial M, Jatene AD. Late results (50 to 182 months) of the Jatene operation. Eur J Cardiothorac Surg. 1992; 6:575–577. discussion 578. PMID: 1449810.
9. Jatene MB, Jatene IB, Oliveira PM, et al. Prevalence and surgical approach of supravalvular pulmonary stenosis after Jatene operation for transposition of great arteries. Arq Bras Cardiol. 2008; 91:17–24. PMID: 18660940.
10. Wernovsky G, Hougen TJ, Walsh EP, et al. Midterm results after the arterial switch operation for transposition of the great arteries with intact ventricular septum: clinical, hemodynamic, echocardiographic, and electrophysiologic data. Circulation. 1988; 77:1333–1344. PMID: 3370773.
11. Yamaguchi M, Hosokawa Y, Imai Y, et al. Early and midterm results of the arterial switch operation for transposition of the great arteries in Japan. J Thorac Cardiovasc Surg. 1990; 100:261–269. PMID: 2385123.
12. Brown JW, Park HJ, Turrentine MW. Arterial switch operation: factors impacting survival in the current era. Ann Thorac Surg. 2001; 71:1978–1984. PMID: 11426778.
13. Mayer JE Jr, Sanders SP, Jonas RA, Castaneda AR, Wernovsky G. Coronary artery pattern and outcome of arterial switch operation for transposition of the great arteries. Circulation. 1990; 82(5 Suppl):IV139–IV145. PMID: 2225398.
14. Pretre R, Tamisier D, Bonhoeffer P, et al. Results of the arterial switch operation in neonates with transposed great arteries. Lancet. 2001; 357:1826–1830. PMID: 11410190.
15. von Bernuth G. 25 years after the first arterial switch procedure: mid-term results. Thorac Cardiovasc Surg. 2000; 48:228–232. PMID: 11005598.
16. Legendre A, Losay J, Touchot-Kone A, et al. Coronary events after arterial switch operation for transposition of the great arteries. Circulation. 2003; 108(Suppl 1):II186–II190. PMID: 12970230.
17. Bonnet D, Bonhoeffer P, Piechaud JF, et al. Long-term fate of the coronary arteries after the arterial switch operation in newborns with transposition of the great arteries. Heart. 1996; 76:274–279. PMID: 8868989.
18. Pasquali SK, Hasselblad V, Li JS, Kong DF, Sanders SP. Coronary artery pattern and outcome of arterial switch operation for transposition of the great arteries: a meta-analysis. Circulation. 2002; 106:2575–2580. PMID: 12427654.
19. Bonhoeffer P, Bonnet D, Piechaud JF, et al. Coronary artery obstruction after the arterial switch operation for transposition of the great arteries in newborns. J Am Coll Cardiol. 1997; 29:202–206. PMID: 8996315.
20. Tanel RE, Wernovsky G, Landzberg MJ, Perry SB, Burke RP. Coronary artery abnormalities detected at cardiac catheterization following the arterial switch operation for transposition of the great arteries. Am J Cardiol. 1995; 76:153–157. PMID: 7611150.
21. Tsuda E, Imakita M, Yagihara T, et al. Late death after arterial switch operation for transposition of the great arteries. Am Heart J. 1992; 124:1551–1557. PMID: 1462913.
22. Kern MJ, Donohue TJ, Aguirre FV, et al. Clinical outcome of deferring angioplasty in patients with normal translesional pressure-flow velocity measurements. J Am Coll Cardiol. 1995; 25:178–187. PMID: 7798498.
23. Youn HJ. Demonstration of pathologic coronary flow dynamics using transthoracic Doppler echocardiography: its potential role in clinical decision-making. Korean Circ J. 2005; 35:269–281.
24. Bengel FM, Hauser M, Duvernoy CS, et al. Myocardial blood flow and coronary flow reserve late after anatomical correction of transposition of the great arteries. J Am Coll Cardiol. 1998; 32:1955–1961. PMID: 9857878.
25. Hauser M, Bengel FM, Kuhn A, et al. Myocardial blood flow and flow reserve after coronary reimplantation in patients after arterial switch and ross operation. Circulation. 2001; 103:1875–1880. PMID: 11294806.
26. Ou P, Mousseaux E, Azarine A, et al. Detection of coronary complications after the arterial switch operation for transposition of the great arteries: first experience with multislice computed tomography in children. J Thorac Cardiovasc Surg. 2006; 131:639–643. PMID: 16515917.
27. Ropers D, Baum U, Pohle K, et al. Detection of coronary artery stenoses with thin-slice multi-detector row spiral computed tomography and multiplanar reconstruction. Circulation. 2003; 107:664–666. PMID: 12578863.
28. Nissen SE, Gurley JC, Grines CL, et al. Intravascular ultrasound assessment of lumen size and wall morphology in normal subjects and patients with coronary artery disease. Circulation. 1991; 84:1087–1099. PMID: 1884441.
29. Pinto NM, Marino BS, Wernovsky G, et al. Obesity is a common comorbidity in children with congenital and acquired heart disease. Pediatrics. 2007; 120:e1157–e1164. PMID: 17974711.
30. Li J, Tulloh RM, Cook A, Schneider M, Ho SY, Anderson RH. Coronary arterial origins in transposition of the great arteries: factors that affect outcome: a morphological and clinical study. Heart. 2000; 83:320–325. PMID: 10677414.
Fig. 1
The progression of aortic insufficiency (A) and pulmonary insufficiency (B) after arterial switch operation. Aortic insufficiency (AI) tended to progress during the follow-up period (p=0.014), while pulmonary insufficiency (PI) did not progress significantly during follow-up (p=0.189). Both columns show the number of patients with various levels of AI or PI corresponding to the follow-up period.

Fig. 2
The progression of aortic stenosis (A) and pulmonary stenosis (B) after arterial switch operation. Aortic stenosis (AS) and pulmonary stenosis (PS) did not progress significantly during the follow-up period (p=0.687, 0.168 respectively). Both columes show the number of patients with various levels of AS or PS corresponding to the follow-up period.
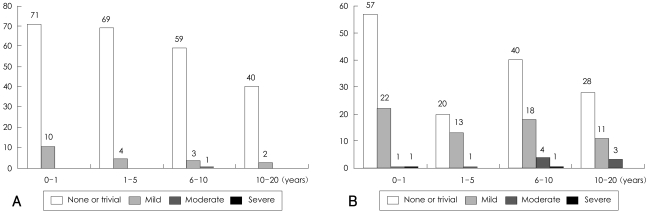
Fig. 3
Twenty-year follow-up results considering aortic insufficiency (AI) and pulmonary stenosis (PS) after arterial switch operation. The 20-year rates of freedom from significant AI (A) and PS (B) were 78.6% and 67.8%, respectively.
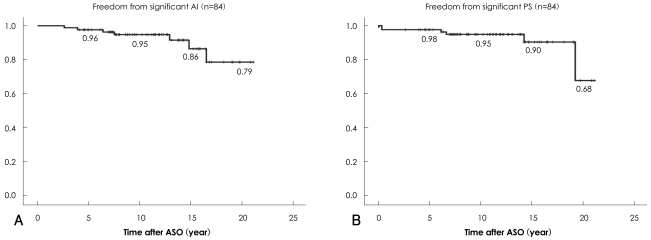
Fig. 4
Survival and re-operation-free rates after arterial switch operation. The survival rate was 96% at 20 years, and the re-operation-free rate was 96%, 90%, 87%, and 83%, respectively, at 5, 10, 15, and 20 years post-operative.

Fig. 5
Growth status (A) and body mass index (B) of patients who underwent arterial switch operation. Patients' growth status and body mass index (BMI) were described 11.3±4.9 years after the arterial switch operation. Most patients (98.8%) demonstrated no delayed growth. A BMI of more than 25, signifying obesity, was observed in 6 patients (7.5%), a prevalence similar to that of the general pediatric population.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download