Abstract
Background and Objectives
Arterial stiffness is a precursor to premature cardiovascular disease. The augmentation index (AI) and pulse pressure (PP) are cardiovascular risk factors. The aim of this study was to define the diagnostic values of the AI and PP from the peripheral arterial and central aortic waveforms in healthy subjects.
Subjects and Methods
We recruited 522 consecutive subjects (mean age 46.3±9.6 years, 290 males) who came to our facility for a comprehensive medical testing. We measured the body mass index (BMI), blood pressure, peripheral and central PP, and a pulse wave analysis that included the central and peripheral AI.
Results
The peripheral and central AIs in the female subjects were significantly higher than that in the male subjects (p<0.001). The peripheral and central PPs in the subjects with hyperlipidemia were significantly higher than subjects with normal lipid profiles (p<0.001). The peripheral and central PPs and peripheral and central AIs significantly increased with age.
Arterial stiffness is associated with cardiovascular risk factors, as well as cardiovascular morbidity and mortality in older subjects and in patients suffering from hypertension, diabetes, end-stage renal disease, and systolic dysfunction.1-6) The aortic augmentation index (AI) may be a surrogate measure of arterial stiffness.7)8) Brachial pulse pressure (PP) is also an independent predictor of the risk of cardiovascular disease in the general population.9-12)
Although the clinical importance of the brachial PP is clear, central PP may correlate more closely with the risk of cardiovascular disease than the brachial pressure.13) Deriving the central pressure from the radial pressure waveforms gives similar results as directly measuring the central pressure.14) This important risk factor remains underused in routine clinical practice for risk prediction, partly because operational thresholds for diagnosing abnormal elevations in arterial stiffness have not been defined. The reference values for the AI and PP in apparently healthy subjects are currently unknown. Thus, the aim of this study was to define the diagnostic values of the AI and PP obtained from the peripheral arterial and central aortic waveforms in healthy subjects.
We recruited 522 consecutive subjects (mean age 46.3±9.6 years, 290 males) who were seen at our facility for comprehensive medical testing from April, 2006, to May, 2006. We measured the body mass index (BMI), serum cholesterol level, systolic (SBP) and diastolic blood pressures (DBP), central and peripheral PP, and performed a pulse wave analysis that included the central and peripheral AIs.
The BMI was calculated as the body weight (kg) to height (m) squared. Hyperlipidemia was defined as a total cholesterol level exceeding 200 mg/dL. The brachial blood pressure was read from the dominant arm in supine subjects. SBP and DBP readings were taken with the dominant arm supported while the subjects were seated after at least 10 minutes of quiet rest, with a mercury column sphygmomanometer and cuff-size adjustment based on the arm circumference. The baseline values for both the SBP and DBP were averaged from two separate measurements taken by the examiner. The subjects with a history of hypertension or diabetes, any previous or concomitant cardiovascular disease, or cardiac arrhythmias were excluded from the study. All patients gave their informed consent before enrollment into the study. The interobserver variability was 88% and the intra-observer variability was 92%.
The peripheral and central PPs were defined as the difference between the SBP and DBP derived from the brachial blood pressure and aortic pulse wave, respectively. The AI was calculated from the left radial artery pulse waves. The data were collected directly into a portable computer; integral software was used to generate an averaged waveform (Gaon 21A System, Hanbyul, Jeonju, Korea). The systolic part of the peripheral arterial waveform was characterized by two pressure peaks. The first peak was caused by the left ventricular ejection, whereas the second peak was a result of the wave reflection. The difference between both pressure peaks reflected the degree to which the peripheral arterial pressure was augmented by the wave reflection.15-17) The peripheral AI was defined as the ratio of the second to first peak of the pressure wave expressed as a percentage. The central AI was calculated from the peripheral AI by an automatic mathematical transformation. The differences in the consecutive mean data during the repeated measurements were less than 0.5 m/s, and the mean data was used for the final analysis.
Statistical analyses were performed using Statistical Package for the Social Sciences 12.0 for Windows software. Chi-square tests and unpaired t-tests were used for statistical differences of the categorical and continuous parameters between genders, respectively. The correlations between the age and other parameters were determined by a linear regression analysis. The statistical differences among each age group for the continuous variables were evaluated using a one-way analysis of variance. We rounded out the 95th prediction bands in order to determine the diagnostic thresholds for the peripheral PP, peripheral AI, central PP, and central AI according to age (Fig. 1). The data are expressed as the mean±standard deviation. A p of less than 0.05 was considered statistically significant.
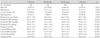
The sample was comprised of 290 males and 232 females. The mean age of the participants was similar for both the males and females. The BMI, stature and body weight, and incidence of being a smoker, and having hyperlipidemia was higher in males than females (Table 1).
The peripheral PP in the males was significantly higher than that in females (p=0.006). There was no significant difference in the central PP between the two groups. The peripheral and central AIs in the females were significantly higher than in males (p<0.001) (Fig. 2).
The peripheral PP (p<0.005) and peripheral AI (p<0.033) in the subjects with hyperlipidemia were significantly higher than in subjects with normal lipid profiles. Central PP and AI levels were similar in the two groups (Fig. 3).
The peripheral and central PPs and peripheral and central AIs had a significant positive correlation to age (Figs. 4 and 5). When divided into groups by age, the peripheral and central PPs and AIs significantly increased with age (Fig. 6) (Table 2).
To determine the diagnostic values, we rounded out the upper limit of the 95th prediction bands for middle-aged men (40 years). The procedure yielded the following thresholds: 70 mmHg for the peripheral PP, 50 mmHg for the central PP, 100% for the peripheral AI, and 40% for the central AI. The aforementioned values for the peripheral and central PPs and peripheral and central AIs needed to be adjusted for age according to the curvilinear relationships. Those values increase approximately 3.3 mmHg for peripheral PP, 5.0 mmHg for central PP, 6.6% for peripheral AI, and 4.0% for central AI for each decade of age over 40 years (Table 3).
The main finding in this study was that the PP and AI significantly increased with gender, hyperlipidemia, and age. Further, these are the data in Koreans on diagnostic values for the PP and AI.
Gatzka et al.18) found that women had smaller and stiffer elastic arteries than men, and that the ventricular contraction and outflow were slower in women than in men: it takes longer to reach the systolic peak in women and the overall systole is prolonged, which is caused by their shorter statue. This change in the wave reflection properties causes a higher AI in women than men. Further, these changes in the elastic artery stiffness parallel the peripheral and central PPs.19)20) We also found that gender was significantly related to the AI. However, we did not adjust PP levels for smoking, BMI, or hyperlipidemia.
Hyperlipidemia is a primary risk factor for the development of coronary atherosclerosis. Wilkinson et al.8)21) investigated the relation between serum cholesterol, arterial stiffness, and central arterial blood pressure. Peripheral blood pressure was similar, but the central PP and AI were higher in the group with hyperlipidemia. However, endothelial dysfunction and reduced nitric oxide bioavailability are associated with hyperlipidemia, which may contribute to the increase in the arterial stiffness and AI. We also found that hyperlipidemia was significantly related to the PP and AI.
With increased age, the walls of the systemic arteries undergo certain histologic changes. Those changes occur independently of any alterations attributed to atherosclerosis. The principal changes with age occur as the intima undergoes hyperplasia. In the load-bearing media, the elastic fibers and laminae lose the orderly arrangement seen in early life and display thinning, splitting, fraying, and fragmentation. The age related thinning and fragmentation of elastin and the increase in collagen are not seen in muscular arteries. Those functional and structural changes in the elastic arteries and arterioles cause an increase in both stiffness and resistance.22-24) Our data were in good agreement with the previous studies, regarding the findings that the peripheral and central PPs and peripheral and central AIs had a significant positive correlation to age.
Recently, many studies have examined the diagnostic values of the AI and PP in different races. Asmar et al.25) studied 61,724 consecutive subjects, and found that the mean value of the peripheral PP across all age ranges was close to 50 mmHg, and thus suggested 65 mmHg as a diagnostic value. Mitchell et al.26) who studied the Framingham Heart Study Offspring Cohort, suggested that the carotid AIs were 33% and 37% in men and women, respectively. In the European study, which included 534 Europeans, the proposed values for the arterial measurements according to age, were approximately 60 mmHg for the peripheral PP, 40 mmHg for the central PP, 90% for the peripheral AI, and 30% for the central AI.27) In another study which included 185 South Africans of black ancestry, the value at an age of 30 years old was 70 mmHg for the peripheral PP, 50 mmHg for the central PP, 100% for the peripheral AI, and 40% for the central AI. Those values needed to be adjusted by 2.5 mmHg, 4.0 mmHg, 10%, and 6%, respectively, for each decade of age over 30 years.28) In a Chinese study, the approximate values for normal peripheral and central PP values were 58 mmHg and 48 mmHg, respectively, and those for the peripheral and central AIs were 105% and 45%, respectively.29) The proposed values in the South African and Chinese were higher than those estimates in the Europeans, but were similar to our Korean data. This discrepancy might be explained by the Korean participants being older than the Europeans, but shorter height in Koreans subjects is probably the main determinant of these ethnic differences.
There were several limitations to this study. First, we analyzed a small number of patients over 60 years old, limiting our ability to detect significant differences in that age group. Studies involving a large number of patients are essential to generalize the results of this study. Second, the AI could have been influenced by the heart rate. Therefore, although we did not adjust for the heart rate, we measured it after 10 minutes of a quiet rest. Third, our data was from a single center; large-scale, long-term follow-up studies will be required in the future. Fourth, this study did not exclude smoking and hyperlipidemia, and may be difficult to apply to general populations.
In conclusion, pending further validation in prospective outcome-based studies, a peripheral PP of 70 mmHg, central PP of 50 mmHg, peripheral AI of 100%, and central AI of 40% may be preliminary diagnostic values in adult subjects.
Figures and Tables
Fig. 6
Relationship of the pulse pressure (PP) and augmentation index (AI) according to the decade of age.

Acknowledgments
We thank Mr. John Martin for his linguistic review. This work was supported by grant No. RTI04-01-01 from the Regional Technology Innovation Program of the Ministry of Commerce, Industry and Energy (MOCIE).
References
1. Park HY, Lee SY, Cho SW, et al. Correlations between the left ventricular diastolic function and aortic stiffness in healthy aged subjects. Korean Circ J. 2006. 36:393–399.
2. Chae CU, Pfeffer MA, Glynn RJ, Mitchell GF, Taylor JO, Hennekens CH. Increased pulse pressure and risk of heart failure in the elderly. JAMA. 1999. 281:634–639.
3. Madhavan S, Ooi WL, Cohen H, Alderman MH. Relation of pulse pressure and blood pressure reduction to the incidence of myocardial infarction. Hypertension. 1994. 23:395–401.
4. Fukui M, Kitagawa Y, Nakamura N, et al. Augmentation of central arterial pressure as a marker of atherosclerosis in patients with type 2 diabetes. Diabetes Res Clin Pract. 2003. 59:153–161.
5. Lee YS, Kim KS, Hyun DW, et al. The change of arterial stiffness according to dialysis in patients with end-stage renal disease. Korean Circ J. 2004. 34:865–873.
6. Domanski MJ, Mitchell GF, Norman JE, Exner DV, Pitt B, Pfeffer MA. Independent prognostic information provided by sphygmomanometrically determined pulse pressure and mean arterial pressure in patients with left ventricular dysfunction. J Am Coll Cardiol. 1999. 33:951–958.
7. Cameron JD, McGrath BP, Dart AM. Use of radial applanation tonometry and a generalized transfer function to determine aortic augmentation in subjects with treated hypertension. J Am Coll Cardiol. 1998. 32:1214–1220.
8. Wilkinson IB, Prasad K, Hall IR, et al. Increased central pulse pressure and augmentation index in subjects with hypercholesterolemia. J Am Coll Cardiol. 2002. 39:1005–1011.
9. Benetos A, Safar M, Rudnichi A, et al. Pulse pressure: a predictor of long-term cardiovascular mortality in a French male population. Hypertension. 1997. 30:1410–1415.
10. Franklin SS, Larson MG, Khan SA, et al. Does the relation of blood pressure to coronary heart disease risk changes with aging? The Framingham Heart Study. Circulation. 2001. 103:1245–1249.
11. London GM, Blacher J, Pannier B, Guerin AP, Marchais SJ, Safar ME. Arterial wave reflections and survival in end-stage renal failure. Hypertension. 2001. 38:434–438.
12. Lee JW. Pulse pressure and systolic blood pressure. Korean Circ J. 2002. 32:293–298.
13. Agabiti-Rosei E, Mancia G, O'Rourke MF, et al. Central blood pressure measurements and antihypertensive therapy: a consensus document. Hypertension. 2007. 50:154–160.
14. Adji A, Hirata K, Hoegler S, O'Rourke MF. Noninvasive pulse waveform analysis in clinical trials: similarity of two methods for calculating aortic systolic pressure. Am J Hypertens. 2007. 20:917–922.
15. Nürnberger J, Keflioglu-Scheiber A, Opazo Saez AM, Wenzel RR, Philipp T, Schäfers R. Augmentation index is associated with cardiovascular risk. J Hypertens. 2002. 20:2407–2414.
16. O'Rourke MF, Gallagher DE. Pulse wave analysis. J Hypertens Suppl. 1996. 14:S147–S157.
17. Wilkinson IB, Cockcroft JR, Webb DJ. Pulse wave analysis and arterial stiffness. J Cardiovasc Pharmacol. 1998. 32:Suppl 3. S33–S37.
18. Gatzka CD, Kingwell BA, Cameron JD, et al. Gender differences in the timing of arterial wave reflection beyond differences in body height. J Hypertens. 2001. 19:2197–2203.
19. Waddell TK, Dart AM, Gatzka CD, Cameron JD, Kingwell BA. Women exhibit a greater age-related increase in proximal aortic stiffness than men. J Hypertens. 2001. 19:2205–2212.
20. Hayward CS, Kelly RP. Gender-related differences in the central arterial pressure waveform. J Am Coll Cardiol. 1997. 30:1863–1871.
21. Wilkinson IB, Cockcroft JR. Cholesterol, endothelial function and cardiovascular disease. Curr Opin Lipidol. 1998. 9:237–242.
22. Nichols WW, O'Rourke MF, Avolio AP, et al. Effects of age on ventricular-vascular coupling. Am J Cardiol. 1985. 55:1179–1184.
23. Cheitlin MD, Zipes DP. Braunwald E, Zipes DP, Libby P, editors. Cardiovascular disease in the elderly. Heart Disease. 2001. 6th ed. Philadelphia: WB Saunders.
24. Nichols WW, Singh BM. Augmentation index as a measure of peripheral vascular disease state. Curr Opin Cardiol. 2002. 17:543–551.
25. Asmar R, Vol S, Brisac AM, Tichet J, Topouchian J. Reference values for clinic pulse pressure in a nonselected population. Am J Hypertens. 2001. 14:415–418.
26. Mitchell GF, Parise H, Benjamin EJ, et al. Changes in arterial stiffness and wave reflection with advancing age in healthy men and women. The Framingham Heart Study. Hypertension. 2004. 43:1239–1245.
27. Wojciechowska W, Staessen JA, Nawrot T, et al. Reference values in white Europeans for the arterial pulse wave recorded by means of the ShygmoCor device. Hypertens Res. 2006. 29:475–483.
28. Shiburi CP, Staessen JA, Maseko M, et al. Reference values for SphygmoCor measurements in South Africans of African ancestry. Am J Hypertens. 2006. 19:40–46.
29. Li Y, Staessen JA, Li LH, Huang QF, Lu L, Wang JG. Reference values for the arterial pulse wave in Chinese. Am J Hypertens. 2008. 21:668–673.




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download