Abstract
Background and Objectives
High aerobic exercise capacity and sport-related physical activity are reported to be inversely associated with arterial stiffness in healthy young adults. However, it is unknown whether increased physical activity and/or high aerobic exercise capacity attenuate arterial stiffness in patients with untreated hypertension.
Subjects and Methods
We studied subjects with never-treated hypertension {n=84 (55 males); mean age±SD, 49±7 years; age range, 36-65 years}. We excluded subjects with a history of diabetes, angina, myocardial infarction, major arrhythmia, or cerebrovascular diseases and those who were taking any cardiovascular medications, including lipid-lowering agents. Carotid intima-media thickness (IMT) and heart-femoral pulse wave velocity (hfPWV) were measured before exercise testing was performed. Physical activity was estimated using a modified Baecke questionnaire. Aerobic exercise capacity was measured with maximal cardiopulmonary exercise testing (maximum oxygen uptake, Vo2max).
Results
Linear regression analysis showed a significant inverse correlation between sport-index and hfPWV (r=-0.404; p<0.001), which multiple linear regression analysis showed to be independent of the individual variables of age, gender, body mass index, mean arterial pressure, total cholesterol, fasting blood glucose, and heart rate (beta=-0.277; p=0.004). However, the work- and leisure-indices and Vo2max were not associated with hfPWV (p>0.05). Carotid IMT was not associated with physical activity indices or Vo2max.
Conclusion
In patients with untreated hypertension, increased sport activity was associated with lower aortic stiffness, but high aerobic exercise capacity was not. These results suggest that regular daily exercise, but not exercise capacity, is an important determinant of aortic stiffness in patients with untreated hypertension.
Many longitudinal studies have demonstrated that increased aortic stiffness is an independent predictor for all-cause and cardiovascular mortality, fatal and non-fatal coronary events, and fatal stroke in patients with uncomplicated essential hypertension,1) type 2 diabetes,2) end-stage renal disease,3) and old age,4) as well as in the general population.5)6) Increased carotid intima-media thickness (IMT) is also a good predictor of adverse cardiovascular event risk.7)8) Thus, recent guidelines for the management of hypertension have adopted measurement of aortic pulse wave velocity (PWV) and carotid IMT for the evaluation of target organ damage and the prediction of risk of cardiovascular disease in hypertensive subjects.9) Although data is limited, it is thought that reduction in aortic stiffness will dramatically decrease cardiovascular events and mortality, regardless of the intervention.10)
High aerobic exercise capacity has been reported to be associated with lower risk of all cause and cardiovascular disease mortality,11) and regular aerobic physical activity may prevent cardiovascular disease.12) Several studies have found that significant age-related increases in aortic stiffness are absent in physically active men13) and women14) and that habitual aerobic endurance-exercise may attenuate age-related increases in aortic stiffness in healthy subjects.13)15)16) However, in subjects with hypertension, data for the effects of aerobic exercise capacity on aortic stiffness are limited and controversial.
Higher levels of aerobic exercise capacity are inversely associated with carotid atherosclerosis,17) but not with aortic stiffness.18) The effect of aerobic exercise capacity and physical activity on aortic stiffness in subjects with never treated hypertension has not yet been defined. Therefore, the present study was performed to evaluate whether increased physical activity and/or high aerobic exercise capacity are associated with attenuation of arterial stiffness and carotid IMT in subjects with never treated hypertension.
We studied subjects between the ages of 36 and 65 years who had never been treated for hypertension (n= 84, 55 males, mean age±SD, 49±7 years). Hypertension was defined as systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg. The blood pressure was confirmed during two or more clinic visits. Exclusion criteria included resting systolic blood pressure ≥180 mmHg and/or diastolic blood pressure ≥110 mmHg; duration of hypertension greater than 2 years; or history of angina, diabetes mellitus, myocardial infarction, significant arrhythmia, stroke, peripheral arterial disease, heart failure, or significant ST changes suggesting coronary artery disease during exercise test. Informed consent was obtained from all patients.
Body mass index was calculated as the weight in kilograms divided by the square of the height in meters. Blood samples were taken for measurement of fasting blood glucose and serum lipid/lipoprotein profiles after subjects had fasted overnight. The PWV and carotid IMT were measured with the patient in the supine position after at least 10 minutes of rest in a controlled environment (quiet room at 22±1℃). Data concerning frequency, duration, and type of habitual physical activity were obtained using the modified Baecke questionnaire of habitual activity, which was designed to quantify work, sports, and non-sport leisure activities.19) A graded treadmill exercise with Bruce protocol was performed to measure aerobic exercise capacity. Maximal oxygen consumption (Vo2max) was measured using online, computer-assisted, open circuit spirometry.
Physical activity was assessed using the modified Baecke physical activity questionnaire at the first visit, before cardiopulmonary exercise testing.19) In brief, the three Baecke survey ordinal indices (work, leisure, and sports) were graded from low (1) to high (5) with respect to physical activity. The work index included eight self-rated questions about work vigor (compared to others of the same age) and frequency of sitting, standing, walking, lifting, carrying heavy loads, sweating, and fatigue experienced after work. The leisure index included four questions that focused on the frequency of television watching and light-intensity activities: walking, bicycling, and walking or bicycling to or from work or shopping. The sport index assessed the sum of the yearly frequency, weekly duration, and coded intensity (low, medium, or high) of up to four self-reported sport activities, as well as the frequency of sweating, general frequency of sport play, and self-rated amount of leisure activities compared with other persons the same age.
Arterial stiffness was assessed by measuring the heart-femoral PWV (hfPWV).20) Measurements were performed using an automated device (VP-2000, Colin, Japan).21) One trained observer performed all the measurements. In brief, electrocardiography electrodes were placed on both wrists, and a heart sound microphone was placed on the left sternal border. Occlusion cuffs that were connected to oscillometric sensors were wrapped around both upper arms and ankles. Both the brachial and ankle blood pressure (BP) were measured simultaneously, and the ankle-brachial pressure index (ABI) was calculated. The carotid and femoral arterial pulse waves were acquired using multielement tonometric sensors placed on the left carotid artery and the femoral artery. The heart-femoral (from the aortic orifice to the femoral artery) pulse transit time was calculated through summation of the carotid-femoral pulse transit time and the heart-carotid pulse transit time. The path length of the heart-carotid segment was automatically calculated based on the patient's height.
Ultrasound measurement of the carotid IMT of the common carotid artery (CCA) was performed using a GE Vivid7 scanner (GE Medical Systems, USA) equipped with a 12 MHz linear array transducer, as previously described.21) All measurements were performed by a well trained sonographer, with the subject in the supine position and the subject's head turned slightly contralateral to the side being examined. The right and left CCAs were scanned first in a transverse plane, and then scanned longitudinally. Two images of the right CCA and two images of the left CCA were scanned and stored as digital images. Measurement of the CCA IMT was conducted using a computer system with automatic IMT measurement software (M'Ath®-Std©, Metris, France).22) The CCA IMT was measured within 2 cm proximal to the carotid bifurcation along at least 1 cm of axial length. The mean values of the right and left CCA IMTs were used for analysis.
Maximal exercise capacity was measured using a treadmill exercise test.23) Vo2max was used as a measure of maximal aerobic capacity. Graded exercise testing was performed using the Bruce treadmill protocol (Q-Stress TM55, V3.5, Quinton, USA), and analysis of expired gases was accomplished using a metabolic cart with online, computer assisted, open circuit spirometry (Sensor-Medics Vmax Encores 29, SensorMedics, USA). For analysis, we used the Vo2max measured in a plateau while workload and heart rate were still increasing.
The Statistical Package for Social Science (SPSS) 13.0 (SPSS Inc, Chicago, Il, USA) statistical software package was used for all statistical analysis. Descriptive statistics of baseline and clinical characteristics are expressed as either means and standard deviations (SD) or as percentages, as appropriate. A p<0.05 was regarded as statistically significant. Associations of sports index, work index, leisure index, and Vo2max with hfPWV and CCA IMT were analyzed using a multiple linear regression model under adjustment for age, sex, body mass index (BMI), mean arterial pressure (MAP), total cholesterol, fasting blood glucose, and heart rate. The results are depicted as standardized coefficients, with p in parentheses. We implemented Analysis of Variance (ANOVA) using the General Linear Model to compare hfPWV, according to tertiles of sport index and Vo2max, as separate models under adjustment for the covariates of age, sex, BMI, heart rate, MAP, total cholesterol, and fasting blood glucose.
The demographic and clinical characteristics of the study subjects are presented in Table 1. Mean systolic blood pressure was 150±15 mmHg, and mean diastolic blood pressure was 94±9 mmHg. Mean Vo2max was 32.2±7.7 mL/kg per minute. Mean hfPWV was 965±114 cm/sec.
Table 2 shows the association of physical activity and Vo2max with hfPWV and CCA IMT. Among the determinants, sport index was significantly associated with hfPWV on multiple regression analysis with adjustment (standardized regression coefficient -0.277; p=0.0004). The other physical activity scores, such as work and leisure index and Vo2max, were not associated with hfPWV (Table 2). CCA IMT was not associated with physical activity scores or Vo2max (Table 2). The highest tertile of the sport index was significantly associated with hfPWV (Table 3). The sport-index was inversely correlated with the hfPWV (Pearson's correlation r=-0.404; p<0.0001; Fig. 1).
Aerobic exercise capacity and physical activity have been reported to be inversely associated with arterial stiffness in young adults.13-16) Habitual aerobic-endurance exercise attenuates age-associated increases in arterial stiffness in healthy subjects. Aortic PWV increases with age, but the difference in aortic PWV between younger and older adults has been shown to be smaller in endurance-trained men, compared with recreationally inactive and sedentary men.15) One study showed no age-related increase in aortic stiffness in physically active women.14) Endurance-trained athletes also had greater arterial compliance compared with age-matched sedentary control subjects.24) An interventional study concerning the effect of exercise on arterial stiffness also showed that short-and long-term regular aerobic exercise can attenuate age-related arterial stiffness in previously sedentary subjects and healthy older subjects.13)25)26)
However, the effects of aerobic exercise on arterial stiffness in subjects with hypertension are controversial. Although aerobic exercise is known to lower blood pressure in patients with hypertension,27) elderly subjects with isolated systolic hypertension have shown resistance to aerobic exercise training.28)29) Furthermore, it is unknown whether increased physical activity reduces aortic stiffness in hypertensive patients. A recent study reported that higher aerobic exercise capacity is not associated with lower aortic stiffness in hypertensive individuals.18) However, the study population was inhomogeneous, included subjects taking antihypertensive medications, and did not evaluate the relationship between physical activity and arterial stiffness. Antihypertensive medication can affect aortic stiffness, and results from inhomogeneous subjects cannot exclude the effects of antihypertensive medications. In addition, previous studies have not evaluated the effects of physical activity and/or aerobic exercise capacity in younger subjects with hypertension.
The present study showed that aortic stiffness is inversely related to sports activity in never-treated hypertensive patients, but not to aerobic exercise capacity. Our findings suggest that daily regular exercise before or soon after the diagnosis of hypertension may attenuate the progression of aortic stiffness. Similar to previous reports, the present study showed no relationship between aerobic exercise capacity and aortic stiffness in hypertensive subjects. Aerobic exercise capacity may be higher in younger sedentary subjects than it is in elderly subjects. Thus, measurement of aerobic exercise capacity may not reflect long-term habitual exercise. The present study implemented the Baecke physical activity questionnaire in order to evaluate long-term, habitual physical activity. This method has been validated and can measure habitual physical activity over a period of one year,30) suggesting that long-term physical activity is more important in the attenuation of aortic stiffness.
In the present study, carotid IMT was not associated with aerobic exercise capacity or physical activity. Jae et al.17) reported a significant negative association between aerobic exercise capacity and the prevalence of carotid atherosclerosis in hypertensive men. However, their study population was different from that of the present study. Their subjects were older. Furthermore, some of them were taking antihypertensive medications and/or had diabetes mellitus. Half of the subjects with atherosclerosis were taking antihypertensive medications, and 33.5% of them were diabetic, a higher proportion than that seen in the non-atherosclerosis group. It is possible that the duration of hypertension in the subjects taking antihypertensive medications might have been longer than in those subjects who had never been treated and were newly diagnosed. Subjects with advanced age, longer duration of hypertension, and a history of diabetes mellitus might have a higher risk of advanced atherosclerosis.
Limitations of the present study include 1) the cross-sectional nature and 2) the study population. In cross-sectional studies, the subject population is not a controlled condition. In order to verify the results of the present study, longitudinal and interventional studies should be undertaken in a well controlled cohort before the diagnosis of hypertension. Follow-up study of that cohort will confirm the effects of regular exercise on the attenuation of aortic stiffness after diagnosis of hypertension. Our study was also limited in that we looked at a small population with a broad age range, from 35 to 65 years. Aerobic exercise capacity may be age-dependent. Thus, to verify the findings of the present study, further longitudinal study should be pursued in a large population.
In conclusion, regular aerobic exercise appears to attenuate aortic stiffness in subjects with hypertension, but aerobic exercise capacity does not appear to have an effect on aortic stiffness. This suggests that daily, regular aerobic exercise before and soon after diagnosis of hypertension may play an important role in the prevention of cardiovascular complications.
Figures and Tables
Fig. 1
Linear regression analysis showed a significant inverse correlation between sport-index and heart-femoral pulse wave velocity (r=-0.404, p<0.0001).
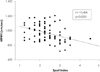
Table 1
Baseline and clinical characteristics of studied subjects (n=84)

Descriptive statistics of baseline and clinical characteristics are expressed using means and standard deviations or percentages, as appropriate. *Indices from modified Baecke questionnaire.19) SD: standard deviation, BMI: body mass index, LDL: low density lipoprotein, HDL: high density lipoprotein, hfPWV: heart-femoral pulse wave velocity, IMT: intima-media thickness
Table 2
Association of physical activity and aerobic exercise capacity with heart-femoral pulse wave velocity and carotid intima-media thickness. Data are standardized regression coefficients (p). Each determinant was analyzed by multiple regression analysis adjusted to age, sex, body mass index, mean arterial pressure, total cholesterol, fasting blood glucose, and heart rate

*Indices from modified Baecke questionnaire.19) hfPWV: heart-femoral pulse wave velocity, IMT: intima-media thickness, Vo2max: maximal oxygen consumption on cardiopulmonary function test
References
1. Laurent S, Boutouyrie P, Asmar R, et al. Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension. 2001. 37:1236–1241.
2. Cruickshank K, Riste L, Anderson SG, Wright JS, Dunn G, Gosling RG. Aortic pulse-wave velocity and its relationship to mortality in diabetes and glucose intolerance: an integrated index of vascular function? Circulation. 2002. 106:2085–2090.
3. Blacher J, Guerin AP, Pannier B, Marchais SJ, Safar ME, London GM. Impact of aortic stiffness on survival in end-stage renal disease. Circulation. 1999. 99:2434–2439.
4. Sutton-Tyrrell K, Najjar SS, Boudreau RM, et al. Elevated aortic pulse wave velocity, a marker of arterial stiffness, predicts cardiovascular events in well-functioning older adults. Circulation. 2005. 111:3384–3390.
5. Mattace-Raso FU, van der Cammen TJ, Hofman A, et al. Arterial stiffness and risk of coronary heart disease and stroke. Circulation. 2006. 113:657–663.
6. Willum-Hansen T, Staessen JA, Torp-Pedersen C, et al. Prognostic value of aortic pulse wave velocity as index of arterial stiffness in the general population. Circulation. 2006. 113:664–670.
7. Bots ML, Hoes AW, Koudstaal PJ, Hofman A, Grobbee DE. Common carotid intima-media thickness and risk of stroke and myocardial infarction. Circulation. 1997. 96:1432–1437.
8. Chambless LE, Heiss G, Folsom AR, et al. Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: The Atherosclerosis Risk in Communities (ARIC) study, 1987-1993. Am J Epidemiol. 1997. 146:483–494.
9. Mancia G, De Backer G, Dominiczak A, et al. 2007 guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2007. 25:1105–1187.
10. Guerin AP, Blacher J, Pannier B, Marchais SJ, Safar ME, London GM. Impact of aortic stiffness attenuation on survival of patients in end-stage renal failure. Circulation. 2001. 103:987–992.
11. Evenson KR, Stevens J, Thomas R, Cai J. Effect of cardiorespiratory fitness on mortality among hypertensive and normotensive women and men. Epidemiology. 2004. 15:565–572.
12. Paffenbarger RS Jr, Hyde RT, Wing AL, Hsieh CC. Physical activity, all-cause mortality, and longevity of college alumni. N Engl J Med. 1986. 314:605–613.
13. Tanaka H, Dinenno FA, Monahan KD, Clevenger CM, DeSouza CA, Seals DR. Aging, habitual exercise, and dynamic arterial compliance. Circulation. 2000. 102:1270–1275.
14. Tanaka H, DeSouza CA, Seals DR. Absence of age-related increase in central arterial stiffness in physically active women. Arterioscler Thromb Vasc Biol. 1998. 18:127–132.
15. Gates PE, Tanaka H, Graves J, Seals DR. Left ventricular structure and diastolic function with human ageing: relation to habitual exercise and arterial stiffness. Eur Heart J. 2003. 24:2213–2220.
16. Boreham CA, Ferreira I, Twisk JW, Gallagher AM, Savage MJ, Murray LJ. Cardiorespiratory fitness, physical activity, and arterial stiffness. Hypertension. 2004. 44:721–726.
17. Jae SY, Carnethon MR, Heffernan KS, Choi YH, Lee MK, Fernhall B. Association between cardiorespiratory fitness and prevalence of carotid atherosclerosis among men with hypertension. Am Heart J. 2007. 153:1001–1005.
18. Kraft KA, Arena R, Arrowood JA, Fei DY. High aerobic capacity does not attenuate aortic stiffness in hypertensive subjects. Am Heart J. 2007. 154:976–982.
19. Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982. 36:936–942.
20. Rhee MY, Lee HY, Park JB. Measurements of arterial stiffness: methodological aspects. Korean Circ J. 2008. 38:343–350.
21. Rhee M. Acute and chronic effects of smoking on the arterial wall properties and the hemodynamics in smokers with hypertension. Korean Circ J. 2005. 35:493–499.
22. Bae JH, Seung KB, Jung HO, et al. Analysis of Korean carotid intima-media thickness in Korean healthy subjects and patients with risk factors: Korea Multi-Center Epidemiological Study. Korean Circ J. 2005. 35:513–524.
23. Fletcher GF, Balady GJ, Amsterdam EA, et al. Exercise standards for testing and training: a statement for healthcare professionals from the American Heart Association. Circulation. 2001. 104:1694–1740.
24. Kingwell BA, Cameron JD, Gillies KJ, Jennings GL, Dart AM. Arterial compliance may influence baroreflex function in athletes and hypertensives. Am J Physiol. 1995. 268:H411–H418.
25. Tabara Y, Yuasa T, Oshiumi A, et al. Effect of acute and long-term aerobic exercise on arterial stiffness in the elderly. Hypertens Res. 2007. 30:895–902.
26. Cameron JD, Dart AM. Exercise training increases total systemic arterial compliance in humans. Am J Physiol. 1994. 266:H693–H701.
27. Nelson L, Jennings GL, Esler MD, Korner PI. Effect of changing levels of physical activity on blood-pressure and haemodynamics in essential hypertension. Lancet. 1986. 2:473–476.
28. Ferrier KE, Waddell TK, Gatzka CD, Cameron JD, Dart AM, Kingwell BA. Aerobic exercise training does not modify large-artery compliance in isolated systolic hypertension. Hypertension. 2001. 38:222–226.
29. Stewart KJ, Bacher AC, Turner KL, et al. Effect of exercise on blood pressure in older persons: a randomized controlled trial. Arch Intern Med. 2005. 165:756–762.
30. Pereira MA, FitzerGerald SJ, Gregg EW, et al. A collection of physical activity questionnaires for health-related research. Med Sci Sports Exerc. 1997. 29:S5–S9.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download