Abstract
Background and Objectives
Poor R-wave progression (PRWP) is a common electrocardiographic diagnosis. However, the diagnostic usefulness of PRWP for coronary artery disease (CAD) and the plausible explanation for subjects with normal heart function are unclear.
Subjects and Methods
We included 20,739 subjects who had routine medical examinations and applied the commonly used criteria (R-waves in V3 or V4 ≤2 mm) and the Marquette criteria in the current study. Subjects with PRWP by the Marquette criteria, but with no evidence of specific causes, were identified. Healthy age- and gender-matched controls were selected randomly for comparing cardiothoracic ratios.
Results
The commonly used criteria in practice were met by 372 of the 20,739 subjects (1.8%). The Marquette criteria were met by 96 subjects (0.5%), and 82 of who agreed to medical evaluation. Five subjects had known CAD and only one subject was shown to have a silent myocardial infarction by additional testing. Therefore, the positive predictive value of PRWP for CAD was 7.3% (6/82) based on the Marquette criteria. As compared with the control group, the subjects with PRWP had a significantly low cardiothoracic ratio (0.425 vs. 0.445, p<0.05), especially among the male group (0.454 vs. 0.407, p=0.02).
Poor R-wave progression (PRWP) is a common electrocardiographic diagnosis. However, there are no standard diagnostic criteria for PRWP, although several complex criteria have been suggested (Table 1).1-6) In addition, the clinical implications of PRWP are as unclear as its definition, and there are no guidelines regarding how to evaluate patients with PRWP. PRWP also occurs in various conditions, such as left bundle branch block, left ventricular hypertrophy, Wolff-Parkinson-White (WPW) syndrome, and coronary artery disease (CAD).4) In clinical practice, it is important to estimate the possibility of CAD among patients with PRWP, i.e., the positive predictive value. One of the aims of the present study was to determine the positive predictive value of PRWP.
In addition, there is no plausible explanation for PRWP in subjects without any specific cause. This can lead physicians to perform unnecessary diagnostic evaluations. Basically, the R-wave amplitude represents the cumulative electrical activation of the ventricle, so it is used for the diagnosis of ventricular hypertrophy.7) Because the heart's location in the thorax can also influence R-wave amplitude, the positions of the precordial electrocardiogram (ECG) leads are determined by bony landmarks on the precordium. A measured R-wave becomes decreased when the lead is further away from the heart. For example, the R-wave amplitude in the left precordium decreases in subjects with a vertical heart position or dextrocardia. A chest radiograph may be helpful in visualizing the relationship between bony landmarks in the chest wall and the actual position of the heart, and the distance from the heart to the ECG leads on the left precordium can be increased in individuals with a low cardiothoracic ratio. Therefore, we hypothesized that PRWP is correlated with a low cardiothoracic ratio (Fig. 1).
We included 20,739 consecutive subjects who underwent routine medical examinations, including an ECG, a chest radiograph and other extensive medical testing, between September 2001 and December 2007 at the National Cancer Center in Korea. We applied the following two PRWP criteria: 1) the commonly used criteria in practice (R-wave in V3 or V4 ≤2 mm) and 2) the Marquette system (Table 1). Further analysis was only performed using the Marquette system because the commonly used criteria were neither objective nor consistent among physicians. We enrolled 82 subjects undergoing further medical evaluations for PRWP, which included history-taking and identifying risk factors for cardiovascular disease, as well as additional tests, such as nuclear single-photon emission computed tomography (SPECT), echocardiography, or exercise treadmill testing, at their cardiologist's discretion.
To evaluate our hypothesis that the PRWP in subjects with normal hearts is correlated with a low cardiothoracic ratio, we identified 76 subjects with PRWP and without evidence of specific causes, such as CAD, left bundle branch block, left ventricular hypertrophy, or WPW syndrome. Then, age- and gender-matched controls without PRWP were randomly selected. They had no cardiovascular symptoms, such as dyspnea, chest discomfort, edema, or syncope, nor did they have risk factors, such as diabetes, hypertension, a smoking habit, dyslipidemia, obesity, or a relevant family history. Chest radiographs were obtained on the same day as the ECG, and cardiothoracic ratios were calculated for subjects with PRWP and for the controls. The cardiac diameters were measured blinded to the patient's age, gender, and clinical details by an investigator.
The cardiothoracic ratio was calculated as the ratio of the maximal transverse diameter of the cardiac silhouette to the distance between the internal margins of the ribs at the level of the right hemidiaphragm. Comparisons of the cardiothoracic ratio were performed among male, female, and all subjects.
Statistical analyses were performed using Stata, version 10.0 (StataCorp LP, College Station, TX, USA). Continuous variables were expressed as the mean±standard deviation and then compared using two-tailed Student's t-tests. Categorical variables were reported as the number and percentile, and compared using chi-squared tests. A p< 0.05 was considered statistically significant.
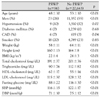
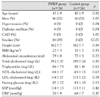
The baseline characteristics of the subjects with and without PRWP are listed in Table 2. The subjects with PRWP were predominantly female (74%) and significantly younger than the males (48±10 years vs. 53±10 years, p<0.01). Further, they had low CAD risk factor profiles, including obesity, lipid, fasting glucose, and blood pressure.
Based on the commonly used criteria in practice (R-wave in V3 or V4 ≤2 mm), the prevalence of PRWP in the general population was 1.8% (372/20,739), and based on the Marquette system it was 0.5% (96/20,739). Further analysis was only performed on the basis of the Marquette system. Six subjects had apparent causes of PRWP, such as left bundle branch block, left ventricular hypertrophy, and WPW syndrome. Eight subjects declined further cardiac evaluation. In the remaining 82 subjects, 5 subjects had known CAD. Sixty-one subjects had neither symptoms nor risk factors for cardiovascular disease, and hence did not undergo further cardiac evaluations.
At the cardiologist's discretion, 16 subjects underwent additional tests (echocardiography in 10 subjects, SPECT in 2 subjects, exercise treadmill testing in 1 subject, and coronary calcium score in 3 subjects); only 1 subject was shown to have had a silent myocardial infarction. Therefore, the positive predictive value of PRWP for CAD was 7.3% (6/82) based on the Marquette system.
We compared 76 subjects without specific PRWP causes with 76 controls, according to the cardiothoracic ratio (Table 3). The cardiothoracic ratios were significantly lower in the subjects with PRWP than in the controls (0.425 vs. 0.445, respectively, p<0.01) (Fig. 2). The difference was more profound in the male group (0.407 vs. 0.454, respectively, p=0.02); however, the cardiothoracic ratio did not differ significantly between subjects with and without PRWP in the female group (0.430 vs. 0.442, respectively, p=0.10).
The present study revealed the prevalence and positive predictive value of PRWP in the general population. This is the first study to investigate this topic and suggest a reasonable cause of PRWP, i.e., a low cardiothoracic ratio. The prevalence of PRWP in the general population (0.5% by the Marquette criterion or 1.8% by the simple criterion based on R-wave amplitude of only two precordial leads) was even lower than in hospitalized adult patients (10%) or in patients examined for CAD (8%).2)8) Subjects with PRWP tend to be female, younger, weigh less, and shorter in height than those without PRWP. Considering that a low cardiothoracic ratio is frequent in the young and those who weigh less,9) it is also postulated that PRWP is associated with a low cardiothoracic ratio.
The positive predictive value of PRWP for CAD was 7.3%, which is also < the previously reported value of 20% in patients with suspected CAD2) because the previous study population was a high risk group different from the general population.
Furthermore, most subjects with CAD and PRWP were already known to be CAD patients from their medical history and only one subject was newly detected by additional cardiac testing. Thus, additional testing for asymptomatic subjects with PRWP may be not reasonable in the general population.
It has been reported that there is a direct correlation between the R-wave amplitude and the left ventricular size or mass.10)11) These reports support our hypothesis that a lower cardiothoracic ratio is associated with PRWP (Fig. 1).
Indeed, we found that the cardiothoracic ratio of subjects with PRWP is lower than that of subjects without PRWP in males, but not in females. There are several explanations for this observation. One reason might be an inconsistent ECG lead placement in females because of the presence of breast tissue. In addition, the females in the control group had a low cardiothoracic ratio; hence the difference in cardiothoracic ratio between the controls and subjects with PRWP might be too small to be distinguishable.
The lack of standard diagnostic criteria for PRWP is confusing for clinicians and the existing criteria are too complex to be applied in practice (Table 1).1-4) It has been reported that the diagnostic values for PRWP are similar among various criteria,12) and the Marquette system is easily applicable as well as being the most commonly used computerized interpretation system.1) Therefore, the Marquette system was used in the present study. Second, although the subjects with PRWP were referred to cardiologists and underwent history-taking and physical examinations, it is possible that we missed some patients with silent myocardial infarctions. We could not perform further cardiac evaluation on all subjects with PRWP because some of them declined further evaluation or had no symptoms or risk factors. Actually, none of the current diagnostic methods is perfect and it is very difficult to detect all cases of silent myocardial infarction. Given that the prevalence of silent myocardial infarction is much <5%,13)14) the number of subjects with silent myocardial infarctions that we missed is likely to be very small, and hence the omission of these subjects is less likely to have a significant effect on our findings. Third, although we included >20,000 subjects, only 96 subjects had PRWP because of its low prevalence (0.5%); as a result of this small sample size, there might have been insufficient statistical power.
Figures and Tables
Fig. 1
Chest radiographs and electrocardiogram in a normal control subject (A) showing a normal cardiothoracic ratio, and in a subject with PRWP (B) showing a low cardiothoracic ratio. PRWP: poor R-wave progression.

Fig. 2
Box plots comparing cardiothoracic ratios in the control and PRWP groups. The cardiothoracic ratio is significantly associated with the presence of PRWP in all (A) and male subjects (B) although it is not in female subjects (C). The central boxes include the middle 50 percentile of the data and horizontal lines show the middle of 80 percentile of data. CT ratios: cardiothoracic ratios, PRWP: poor R-wave progression.

References
1. Physician's Guide to Marquette Electronics Resting ECG Analysis. 1991. Milwaukee, Wis: Marquette Electronics Inc.
2. DePace NL, Colby J, Hakki AH, Manno B, Horowitz LN, Iskandrian AS. Poor R wave progression in the precordial leads: clinical implications for the diagnosis of myocardial infarction. J Am Coll Cardiol. 1983. 2:1073–1079.
3. Wagner A, Mahrholdt H, Holly TA, et al. Contrast-enhanced MRI and routine single photon emission computed tomography (SPECT) perfusion imaging for detection of subendocardial myocardial infarcts: an imaging study. Lancet. 2003. 361:374–379.
4. Zema MJ, Collins M, Alonso DR, Kligfield P. Electrocardiographic poor R-wave progression: correlation with postmortem findings. Chest. 1981. 79:195–200.
5. Joo IJ, Hur DY, Kim ES, et al. Differential diagnosis in cases showeing poor R-wave progression on EKG by ventorcardiography. Korean Circ J. 1986. 16:349–356.
6. Won KH, Chang MY, Oh KS, Kim YC, Lee HC. Clinical observation on poor R-wave progression. Korean Circ J. 1983. 13:195–201.
7. Wagner GS. Marriott's Practical Electrocardiography. 2001. 10th ed. Philadelphia, PA: Lippincott Williams & Wilkins.
8. Zema MJ, Kligfield P. Electrocardiographic poor R wave progression: I. correlation with the Frank vectorcardiogram. J Electrocardiol. 1979. 12:3–10.
9. Zaman MJ, Sanders J, Crook AM, et al. Cardiothoracic ratio within the "normal" range independently predicts mortality in patients undergoing coronary angiography. Heart. 2007. 93:491–494.
10. Feldman T, Borow KM, Neumann A, Lang RM, Childers RW. Relation of electrocardiographic R-wave amplitude to changes in left ventricular chamber size and position in normal subjects. Am J Cardiol. 1985. 55:1168–1174.
11. Sugita S, Takada K, Takada H, Nagashima M, Hayano J. The relationship between R amplitude in lead V5 (RV5) and left ventricular mass in the groups of adolescent subjects classified by body composition. Jpn Circ J. 1998. 62:893–899.
12. Gami AS, Holly TA, Rosenthal JE. Electrocardiographic poor R-wave progression: analysis of multiple criteria reveals little usefulness. Am Heart J. 2004. 148:80–85.
13. Sigurdsson E, Thorgeirsson G, Sigvaldason H, Sigfusson N. Unrecognized myocardial infarction: epidemiology, clinical characteristics, and the prognostic role of angina pectoris. Ann Intern Med. 1995. 122:96–102.
14. Kannel WB, Cupples LA, Gagnon DR. Incidence, precursors and prognosis of unrecognized myocardial infarction. Adv Cardiol. 1990. 37:202–214.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download