Introduction
Congenital long QT syndrome (LQTS) is a potentially lethal cardiac channelopathy that affects nearly 1 in 3,000 people and has an estimated annual mortality of 1%.1) LQTS may be occult for an indefinite time period or may present with syncope, seizures, or sudden death at a young age.2) Our understanding of the genetic basis of LQTS is increasing,3) giving us the ability to classify the disease into different types. For instance, one type of LQTS is triggered by exercise, especially swimming,4) while another type of LQTS is associated with sleep or inactivity, and electrocardiographic abnormalities lessen with an increased heart rate. Yet another type of LQTS can be triggered by a startle response, e.g., something as seemingly benign as an alarm clock ringing. However, the diagnosis of LQTS still remains a challenge. The cardinal electrocardiogram (ECG) feature of LQTS, namely QT prolongation, can be difficult to recognize and may be non-specific. In addition, many physicians struggle with measuring or confirming the computer-derived rate-corrected QT interval (QTc).5) Herein we report a case of epinephrine-induced polymorphic ventricular tachycardia in a patient with congenital long QT syndrome.
Case
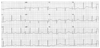
A 24-year-old Korean woman presented to the department of plastic surgery for surgical excision of a nevus on her nose. She was otherwise healthy and had no history of cardiac disease. Her routine pre-operative ECG showed a sinus rhythm with prolonged QT and QTc intervals as long as 528 and 562 ms, respectively (Fig. 1). Detailed history-taking after admission revealed three episodes of syncope associated with both physical and emotional upset, such as a 100 meter sprint, tug of war, and arguing with a stranger in a night club. Her family history was unremarkable for syncope or premature sudden death. Her routine laboratory findings and 2-dimentional echocardiographic findings were also unremarkable. As her syncopal episodes were related to physical exertion, an exercise ECG was performed; however, the test was uneventful with no syncope or ventricular arrhythmia. Thus, an epinephrine infusion test was performed according to the protocol of Shimizu and Antzelevitch.6) Immediately after the bolus injection of 0.1 µg/kg of epinephrine, the ECG showed marked prolongation of the QT interval followed by polymorphic ventricular tachycardia (Fig. 2). Direct current shock promptly terminated the ventricular tachycardia and restored a sinus rhythm with prominent T wave alternans, which lasted for a few minutes. With all of these clinical features we made the diagnosis of a long QT syndrome, probably type 1. A gene study was recommended, which was declined by the patient and her family. She was recommended to avoid competitive sports, and atenolol (100 mg per day) was prescribed. She has remained symptom-free for more than 2 year.
Discussion
In this case, the patient's resting ECG showed QT interval prolongation and a broad-based T wave, while during the exercise stress test, no ventricular tachyarrhythmia was noted, and polymorphic ventricular tachycardia was induced only after epinephrine infusion. All of the patient's features were most consistent with a diagnosis of type 1 LQTS.7) If the patient had undergone an excision of the nevus under local anesthesia with local epinephrine to control bleeding with no pre-operative ECG, she might have suffered from cardiac arrest due to epinephrine-induced polymorphic ventricular tachycardia. Even the patient considered the syncopal episodes as 'simple faints' with no clinical significance. A correct ECG reading and elaborate history-taking helped us determine the patient's disease. This is the first case of epinephrine-induced polymorphic ventricular tachycardia in Korea for the diagnosis of a suspected long QT syndrome.
Recent lines of evidence have suggested that cardiac events associated with sympathetic stimulation are more common among the LQT1 than the LQT2 or LQT3 types of congenital LQTS.4)8) Provocative testing, particularly the epinephrine QT stress test, may aid in unmasking such individuals with concealed LQTS, especially type 1 LQTS.9)10) In the normal heart, epinephrine increases both ionotropy and chronotropy.11) On the other hand, individuals with LQT1 have a compromised slow component of the delayed rectifier potassium current (IKs) which is expected to shorten the QT intervals during tachycardia less effectively than in normal individuals.11) The superimposition of major catecholamine release, as happens during exercise without appropriate QT adaptation, sets the stage for early after-depolarizations, which may then lead to polymorphic ventricular tachycardia.12) The critical role of an impaired IKs in the facilitation of adrenergic-dependent arrhythmias has implications for therapy. Indeed, 88% of LQT1 patients are at risk during conditions of sympathetic hyperactivity, for example, exercise, head up tilt test,13) or emotions.8) Thus, anti-adrenergic treatment is highly effective for LQT1.14) β-adrenergic blockade does not shorten the QT interval at rest, but suppresses cardiac events in LQT1, whereas the efficacy of β-blockade is reduced in LQT2 and unclear in LQT3.14)
The mortality of untreated and symptomatic patients with LQTS exceeds 20% in the year after the first syncopal episode and approaches 50% within 10 years;15) however, mortality can be significantly reduced by appropriate therapy. A subsequent analysis that included only adults showed a 60% reduction in the cardiac event rate with β-blockade.16) Given the incomplete effectiveness of β-blockers in preventing sudden death in LQTS, implanting a cardioverter-defibrillator may be appropriate in some patients; however, the patient described herein has remained symptom-free for more than 2 year with appropriate lifestyle modification and β-blockers.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download