Abstract
Background and Objectives
Right ventricular (RV) dysfunction is associated with a poor prognosis in patients with an acute pulmonary embolism (APE). We studied the role of electrocardiography and biomarkers for early detection and recovery of right ventricular dysfunction (RVD) in APE.
Subjects and Methods
The medical records of 48 consecutive patients diagnosed with APE using CT-angiography, at the Kangdong Sacred Heart Hospital, between January 2004 and February 2008 were reviewed retrospectively. RVD was assessed by serial echocardiography (ECG). Patients with one of the following were considered to have RVD: 1) RV dilatation (enddiastolic diameter >30 mm in the parasternal long axis view), 2) RV free wall hypokinesia, and 3) paradoxical septal systolic motion. We compared the electrocardiographic findings and the biomarkers for the early detection of RVD.
Results
The electrocardiographic findings showed T-wave inversion (TWI) in leads V1 to V3 with a sensitivity of 75% and a specificity of 95%, and a diagnostic accuracy of 80% for the detection of RVD, with positive and negative predictive values of 95.5% and 73.1%, respectively; these results were better than the biomarkers such as cardiac enzymes or B-type natriuretic peptide (BNP) for the early detection of RVD. TWIs persisted throughout the period of RVD, in contrast to a transient S1Q3T3 pattern detected during the acute phase only.
Right ventricular (RV) dysfunction is a frequent consequence of severe pulmonary embolism (PE), and correlates with a poor prognosis and high mortality rates.1-5) Therefore, the detection of right ventricular dysfunction (RVD) is important for deciding on the optimal management strategy for patients with acute pulmonary embolism (APE). Previous studies have suggested that several cardiac biomarkers such as cardiac troponins or natriuretic peptides can improve risk stratification of patients with APE.6-12) However, because of its simplicity, widespread availability and low cost, the 12-lead electrocardiogram (ECG) has definite clinical advantages for the emergency triage of patients with APE. Among various ECG findings, some studies focused on inverted T waves in the precordial leads and found them to be related to RVD in patients with APE.13-16)
This study was conducted to compare the clinical usefulness of ECG findings and cardiac biomarkers for the assessment of RV involvement and short-term prognosis in patients with acute pulmonary embolism.
The medical records of 92 consecutive patients with an acute pulmonary embolism that were treated at the Kangdong Sacred Heart Hospital between January 2004 and February 2008 were reviewed retrospectively. The diagnosis of APE was confirmed by high-resolution computed tomography of the chest. The exclusion criteria were chronic obstructive pulmonary disease or cor pulmonale, dilated cardiomyopathy, and evidence at ECG of right ventricular hypertrophy, suggesting long-standing RVD.
Transthoracic ECG was performed within 24 hours of presentation.17) Patients with one or more of the following were considered to have RV dysfunction: 1) RV dilatation (end-diastolic diameter >30 mm in the parasternal long axis view), 2) RV free wall hypokinesia, and 3) paradoxical septal systolic motion. The study population was grouped as patients with or without RVD.
We analyzed the ECG findings previously shown to be associated with pulmonary embolism: 1) T-wave inversion (TWI) in the precordial leads, 2) S1Q3T3, 3) complete or incomplete right bundle branch block (RBBB), 4) sinus tachycardia, 5) peripheral low voltage, and 6) pulmonary P waves.15)18) Precordial TWIs were defined by the presence of pointed and symmetrical inverted T waves from V1 to V3 or beyond. The S1Q3T3 pattern was defined according to the criteria of McGinn and White {S wave in lead I and Q wave in lead III, with an amplitude of more than 0.15 mV (1.5 mm) associated with TWIs in lead III}. A right bundle branch block was defined according to conventional criteria. Sinus tachycardia was defined as an increase in sinus rhythm to >100 beats/min. Peripheral low QRS voltage was defined when the amplitude of the largest QRS deviation (positivity or negativity) in the peripheral leads was <5 mm. Pulmonary P waves were defined when its amplitude reached 0.25 mV in lead II. If a patient showed serial ECG changes all ECG patterns were analyzed.
Blood samples were obtained within 24 hours of presentation. Cardiac troponin I (cTnI) levels were determined using the immunometric assay (ADVIA Centaur, Bayer Diagnostics, Tarrytown, NY, USA). Detectable plasma cTnI levels (>0.78 ng/mL) were considered to be elevated. B-type natriuretic peptide (BNP) was measured on the ADVIA Centaur system (Bayer Diagnostics, Tarrytown, NY, USA) on plasma specimens. The normal range of BNP was less than 100 pg/mL.
Continuous variables were expressed as the mean±SD. The dichotomous variables were expressed as a percent. Statistical comparisons of the continuous variables were performed by the Student's t test. Chi-square analysis was used to compare categorical variables. A p<0.05 was considered to be statistically significant. All statistical analyses were performed with Statistical Package for Social Science (SPSS) 12.0 for Windows (SPSS Inc., Chicago, IL, USA).
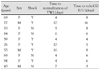
Among 92 patients diagnosed with APE, 44 were excluded from the study (38 with missing data for the biomarkers; either troponin or BNP, or both, 4 with dilated cardiomyopathy or New York Heart Association class III or IV heart failure, 2 with a chronic pulmonary embolism). The mean age of the study population was 66±15 years, and 52.1% of patients were women. Among 48 of the study patients, 20 (41.7%) had normal RV function, and the other 28 (58.3%) had RV dysfunction. There were more patients presenting with shock, defined as persistent systolic arterial pressure less than 90 mmHg and clinical signs of organ hypoperfusion (clouded sensorium, oliguria, and cold and clammy skin) among patients with RVD (p=0.007). Six patients (12.5%) died during the hospital admission, and among these six deaths, five patients were in the group with RVD. The mean value for cardiac troponin I was significantly higher in patients with RVD compared to patients without RVD (0.76±1.14 vs. 0.15±0.91 mg/dL, p=0.015); however, this value was not considered to be elevated (>0.78 mg/dL). The levels of BNP were not significantly different between the patients with RVD and those without RVD (Table 1).
Among the 48 patients, only four patients (8.3%) had normal electrocardiographic results. Eight patients had atrial fibrillation. No patient had pulmonary P waves. TWIs in the precordial leads were the most prevalent findings (45.8%) and low voltage the least (12.5%). TWIs in leads V1 to V3, or more, were significantly more frequent in patients with RV dysfunction than in those without RV dysfunction (75.0% vs. 5.0%, p<0.0001). Similarly, sinus tachycardia and complete or incomplete RBBB were significantly more frequently observed in patients with RV dysfunction than in those without RV dysfunction (50.0% vs. 15.0%, p=0.012, and 46.4% vs. 15.0%, p=0.023, respectively). Although the mean cTnI value was greater in patients with RVD than in patients without RVD (p=0.015) (Table 1), the frequency of elevated cTnI was not significantly different between the two groups. The frequency of elevated BNP was greater in patients with RVD than in those without RVD, however, this difference did not reach statistical significance (Table 2). Of the electrocardiographic criteria studied for the prediction of RV dysfunction, precordial TWIs had a sensitivity of 75.0%, specificity of 95.0%, and positive and negative predictive values of 95.5% and 73.1%, respectively.
Among 21 patients with RVD that showed TWI on the ECG, 12 patients had normalization of the T-wave inversions during hospitalization. Ten patients showed improved RVD on ECG. Table 3 summarizes age, gender, presence of shock, the time to normalization of TWI, and the time to confirmation of improvement of RVD on the ECG of these patents. The interval to ECG change and echocardiographic change were similar as shown in Table 3. Fig. 1 shows serial ECG changes in a representative case. Note that TWIs appeared on the day of the event and normalization of the T-wave with time, associated with improvement of the right ventricular dysfunction.
In the present study, we compared well-known electrocardiographic features with biomarkers of APE to determine their utility for the identification of RV dysfunction. TWIs in the precordial leads had good specificity and moderate sensitivity for the identification of RV dysfunction, consistent with the findings of previous studies.9)13)19) Several prior studies have shown the usefulness of cardiac troponin and BNP for the detection of RVD.7)8)20) However, the results of this study showed no significant association between the elevation of cTnI or BNP and RVD on transthoracic ECG.
The pathophysiology of T-wave changes in the precordial leads is not well-established. Some authors attribute them to coronary insufficiency.19) However, there have been contradictory reports linking high coronary blood flow with PE that drops only during the final stages. Others have suggested a cathecholamine-mediated phenomenon as in other clinical conditions known to cause global TWIs.19)21) However, there is not enough evidence to support this theory.
Persistent RVD is known to be associated with recurrent thromboembolic events.22) The optimal timing for follow-up of right ventricular function is not known. Yoshigawa et al.19) reported serial changes of negative T waves in 15 patients with acute massive pulmonary embolisms. They reported that disappearance of the TWI was associated with improvement of pulmonary hypertension, consistent with our findings. Therefore, the disappearance of TWIs may guide the clinician to the appropriate time for follow up ECG to evaluate the patient for RV function.
This study was conducted retrospectively and the interpretation of the findings is limited by the small sample size. The study population with RVD was greater than the patients without RVD; the cardiac troponin and BNP were usually measured in the patients with RVD. The timing for the follow-up ECG was not consistent; therefore, the exact time that the RVD improved could not be confirmed. Prospective studies with larger numbers of patients are required to investigate the usefulness of TWIs for guiding the clinician in the time to perform follow-up ECG to confirm improvement of RVD.
In conclusion, electrocardiographic features of negative TWIs in the precordial leads was a more reliable finding for the identification of RV dysfunction in patients with acute pulmonary embolism compared to biomarkers such as cardiac troponin and BNP. In addition, improvement of RV function can be confirmed by the disappearance of TWI in patients with such ECG changes.
Figures and Tables
Fig. 1
Representative example of serial changes on the electrocardiogram (ECG) of a 67-year-old patient with a massive pulmonary embolism during admission for multiple rib fractures. Normal ECG on admission (A) changed with appearance of complete right bundle branch block (RBBB) and sinus tachycardia on day 4 when the patient presented with sudden dyspnea and shock (B). Panel C shows T-wave inversions (TWIs) in leads V1-4, which followed the disappearance of RBBB after thrombolytic therapy on the day of the event with right ventricular enlargement and hypokinesis on ECG. Note the normalized TWIs in the precordial leads on day 8 (D), and the ECG performed on the same day showed improvement of right ventricular dysfunction.

References
1. Stein PD, Beemath A, Matta F, et al. Enlarged right ventricle without shock in acute pulmonary embolism: prognosis. Am J Med. 2008. 121:34–42.
2. Kreit JW. The impact of right ventricular dysfunction on the prognosis and therapy of normotensive patients with pulmonary embolism. Chest. 2004. 125:1539–1545.
3. Wolfe MW, Lee RT, Feldstein ML, Parker JA, Come PC, Goldhaber SZ. Prognostic significance of right ventricular hypokinesis and perfusion lung scan defects in pulmonary embolism. Am Heart J. 1994. 127:1371–1375.
4. Lualdi JC, Goldhaber SZ. Right ventricular dysfunction after acute pulmonary embolism: pathophysiologic factors, detection, and therapeutic implications. Am Heart J. 1995. 130:1276–1282.
5. Kasper W, Konstantinides S, Geibel A, Tiede N, Krause T, Just H. Prognostic significance of right ventricular afterload stress detected by echocardiography in patients with clinically suspected pulmonary embolism. Heart. 1997. 77:346–349.
6. Aksay E, Yanturali S, Kiyan S. Can elevated troponin I levels predict complicated clinical course and inhospital mortality in patients with acute pulmonary embolism? Am J Emerg Med. 2007. 25:138–143.
7. Amorim S, Dias P, Rodrigues RA, et al. Troponin I as a marker of right ventricular dysfunction and severity of pulmonary embolism. Rev Port Cardiol. 2006. 25:181–186.
8. Pieralli F, Olivotto I, Vanni S, et al. Usefulness of bedside testing for brain natriuretic peptide to identify right ventricular dysfunction and outcome in normotensive patients with acute pulmonary embolism. Am J Cardiol. 2006. 97:1386–1390.
9. Punukollu G, Khan IA, Gowda RM, Lakhanpal G, Vasavada BC, Sacchi TJ. Cardiac troponin I release in acute pulmonary embolism in relation to the duration of symptoms. Int J Cardiol. 2005. 99:207–211.
10. Kruger S, Graf J, Merx MW, et al. Brain natriuretic peptide predicts right heart failure in patients with acute pulmonary embolism. Am Heart J. 2004. 147:60–65.
11. La Vecchia L, Ottani F, Favero L, et al. Increased cardiac troponin I on admission predicts in-hospital mortality in acute pulmonary embolism. Heart. 2004. 90:633–637.
12. Pruszczyk P, Bochowicz A, Torbicki A, et al. Cardiac troponin T monitoring identifies high-risk group of normotensive patients with acute pulmonary embolism. Chest. 2003. 123:1947–1952.
13. Kosuge M, Kimura K, Ishikawa T, et al. Prognostic significance of inverted T waves in patients with acute pulmonary embolism. Circ J. 2006. 70:750–755.
14. Geibel A, Zehender M, Kasper W, Olschewski M, Klima C, Konstantinides SV. Prognostic value of the ECG on admission in patients with acute major pulmonary embolism. Eur Respir J. 2005. 25:843–848.
15. Punukollu G, Gowda RM, Vasavada BC, Khan IA. Role of electrocardiography in identifying right ventricular dysfunction in acute pulmonary embolism. Am J Cardiol. 2005. 96:450–452.
16. Sarin S, Elmi F, Nassef L. Inverted T waves on electrocardiogram: myocardial ischemia versus pulmonary embolism. J Electrocardiol. 2005. 38:361–363.
17. Kwak MH, Oh J, Jeong JO, et al. Role of echocardiography as a screening test in patients with suspected pulmonary embolism. Korean Circ J. 2001. 31:500–506.
18. Yoon NS, Cho JG, Park HW, et al. Usefulness of the 12-lead electrocardiography in the diagnosis and evaluation of severity of pulmonary thromboembolism. Korean Circ J. 2005. 35:389–395.
19. Yoshinaga T, Ikeda S, Nishimura E, et al. Serial changes in negative T wave on electrocardiogram in acute pulmonary thromboembolism. Int J Cardiol. 1999. 72:65–72.
20. Zhu L, Yang YH, Wu YF, Zhai ZG, Wang C. Value of transthoracic echocardiography combined with cardiac troponin I in risk stratification in acute pulmonary thromboembolism. Chin Med J. 2007. 120:17–21.
21. Lui CY. Acute pulmonary embolism as the cause of global T wave inversion and QT prolongation: a case report. J Electrocardiol. 1993. 26:91–95.
22. Grifoni S, Vanni S, Magazzini S, et al. Association of persistent right ventricular dysfunction at hospital discharge after acute pulmonary embolism with recurrent thromboembolic events. Arch Intern Med. 2006. 166:2151–2156.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download