Introduction
Inhaled iloprost is used as a therapeutic option for pulmonary hypertension, especially in adults; however, have been but a few reports on the use of iloprost in neonates and infants. Prostacyclin (PGI2) is an arachidonic acid metabolite formed by prostacyclin synthase in the vascular endothelium. Its effect on vascular tone is mediated by an increment in adenosine 3':5'-cyclic monophosphate (cAMP) levels and is comparable to that of inhaled nitric oxide (NO), which increases the cyclic guanosine monophosphate (cGMP) levels. Herein we report the use of iloprost in treating pulmonary hypertension in an infant with bronchopulmonary dysplasia (BPD). Inhaled iloprost reduced the pulmonary hypertension and improved oxygenation without decreasing the systemic blood pressure.
Case
A 5-month-old male infant was brought to the premature baby clinic with severe dyspnea and chest retractions. He was immediately transferred to the intensive care unit.
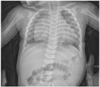
The infant was born at 26 weeks of gestation via caesarean section because of acute chorioamninitis and placentitis. The birth weight was 800 gm. He received neonatal intensive care due to respiratory distress syndrome and prematurity, during which he developed BPD. He was discharged from the neonatal intensive care unit in stable condition after 4 months. The initial oxygen saturation was 80%. The liver was palpated 4 cm below the right subcostal margin. A chest radiograph showed severe cardiomegaly and BPD (Fig. 1). Based on echocardiography, the pulmonary pressure was elevated, with a pressure gradient (TR PG) of 48 mmHg and there was a severely dilated right ventricle (RV) with tricuspid valve regurgitation (Fig. 2).
Therapeutic strategies were aimed at optimizing respiratory function and alkalinization in order to decrease the pulmonary artery pressure. The initial treatments included respiratory support with high frequency oscillatory ventilation (HFOV) and sildenafil (3 mg/kg/day), an oral phosphodiesterase-5 inhibitor; however, the clinical condition had not improved significantly by the 3rd hospital day. The infant had chest retractions and the oxygen saturation was between 70% and 80%. His oxygen requirements progressively increased, persistent cardiomegaly was noted on the chest radiograph, and serial echocardiograms showed pulmonary hypertension, thus the HFOV was discontinued.
NO was not available at our hospital, therefore inhaled iloprost was added with continuous oral sildenafil. We applied iloprost through an aerosolizing circuit and nebulizer for 20 days. With the additional administration of iloprost, his condition improved and he was weaned from oxygen. A follow-up chest radiograph showed improvement in the cardiomegaly (Fig. 3). The inhaled iloprost increased the oxygenation (saturation >95%). Serial echocardiograms showed mild elevated pulmonary pressure, with a TR PG of 34 mmHg and a decrease in the size of the RV (Fig. 4).
Enteral nutrition was successful. The hepatomegaly was resolving. After 23 days, he was discharged with a normal oxygen saturation on room air.
Discussion
Pulmonary artery hypertension (PAH) is a common cardiovascular complication in preterm infants with BPD and is associated with increased morbidity and mortality.1)2)
PAH is characterized by elevation of the pulmonary artery pressure and pulmonary vascular resistance, which can lead to progressive right heart failure and death.3-6) Premature infants with BPD and severe PAH are at a high risk of death, particularly during the first 6 months after the diagnosis of PAH.7)
On the basis of advances in vascular biology and known pathogenic mechanisms underlying PAH, three general classes of therapeutic agents have been developed and are currently available for the treatment of PAH, including prostacyclin analogues (epoprostenol, treprostinil, and iloprost), endothelin receptor antagonists (bosentan and ambrisentan), and phosphodiesterase inhibitors (sildenafil).5)8)9)
Iloprost is a prostacyclin-analog which is an important mediator of pulmonary vasodilatation. However, few data are available about its use in the critical care of infants. Ivy et al.10) reported the safety and efficacy of inhaled iloprost in pediatric patients with PAH; the acute pulmonary vasodilator response to inhaled iloprost was equivalent to the effects of inhaled NO.10)
Our clinical experience indicates that iloprost is a promising therapy for pulmonary hypertension, especially in situations in which inhaled NO is unavailable. Direct lung administration is the main advantage of iloprost. Future studies are warranted to better define the safety and efficacy of iloprost in comparison with other vasodilator drugs.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download