Abstract
Background and Objectives
The early morning blood pressure surge (EMBPS) has been reported to be associated with cardiovascular events. The aim of this study was to investigate the relationship between 24-hour ambulatory BP monitoring (ABPM) parameters and conventional cardiovascular risk factors.
Subjects and Methods
Patients (n=346) never-treated for essential hypertension with no other cardiovascular risk factors, such as diabetes, dyslipidemia, and nephropathy were enrolled. The EMBPS was defined as the early morning systolic BP minus the lowest night systolic BP. We compared the 24-hour ABPM parameters in two groups divided by age (<60 and ≥60 years) and examined the association between the 24-hour ABPM parameters and cardiovascular risk factor.
Results
The EMBPS (18±14 vs. 24±14 mmHg, p=0.002), 24-hour mean blood pressure {MBP; 102±9 vs. 105±11 mmHg, p=0.044}, and 24-hour mean pulse pressure (PP; 52±10 vs. 58±11 mmHg, p<0.001) were significantly increased in the elderly subjects compared to the younger subjects. The degree of decrease was less in the elderly subjects (10±8 vs. 7±10%, p=0.002). Based on multivariate analysis, age was an independent risk factor for the highest quartile of EMBPS (>28 mmHg) after adjusting for gender differences, body mass index, and various 24-hour ABPM parameters (odds ratio, 1.051; 95% confidence interval, 1.028-1.075; p<0.001).
Twenty-four-hour ambulatory blood pressure monitoring (24-hour ABPM) provides more accurate information on the diurnal variation of blood pressure (BP) than office- or home-monitored BP, and allows more accurate predictions of target organ damage (TOD) than BP measurements taken in an office. In cases in which the 24-hour mean systolic BP (SBP) is >135 mmHg, the risk of developing cardiovascular complications is 2 times higher than in other cases.1)2)
Generally, the mean BP at night is lower (by at least 10-20%) than during the day, and is referred to as "the dipper." It has been reported that in cases without nocturnal BP reduction (non-dippers), the risk of cardiovascular events is 3 times higher than in dippers. However, in cases with marked nocturnal BP reduction (≥20%; extreme dippers), transient ischemic attacks (TIA) are more prevalent.1)2) In a study of hypertensive patients,3) it was demonstrated that BP is generally lowest at 3 a.m., begins to rise at 6 a.m., and exhibits the highest values at 10 a.m. In addition, in hypertensive patients, SBP rises by 3 mmHg per hour and diastolic BP (DBP) rises by 2 mmHg per hour in each of the 4-6 hours after awakening.3) Based on multivariate analysis, the waking morning BP surge is significantly associated with cardiovascular risk, independent of age and 24-hour BP level.4)
There are 3 pathophysiologic mechanisms associated with the increased risk of cardiovascular events in the early morning period. The first is increased intra-arterial pressure and vasoconstriction of the coronary artery due to the activation of the sympathetic nerve system in the early morning. The second is the elevation of BP itself, which promotes an increase in cardiac stroke work, resulting in increasing shear stress on blood vessels and an increased risk of plaque rupture. The third, hypercoagulability in the early morning, is induced by an increase in platelet aggregation and reduces the function of the fibrinolytic system. As a consequence of these 3 mechanisms, the threshold for myocardial infarction becomes low, promoting plaque rupture in the coronary arteries, and causing vessel occlusion and infarction.5)6)
With aging, not only the elevation of BP,7-9) but also excessive early morning BP surges (EMBPS), are associated with cardiovascular events, such as myocardial infarction, stroke, and sudden cardiac death; consequently, excessive EMBPS are considered to be an independent risk factor for various cardiovascular events.10-12) Additionally, beyond the approximate age of 60 years, SBP continues to increase, but DBP reaches a plateau or gradually falls, and this leads to an accelerated rise in pulse pressure (PP).9)
Thus, the aim of this study was to examine the age-related changes among the parameters determined by 24-hour ABPM, including EMBPS, and conventional cardiovascular risk factors, and examine the association between 24-hour ABPM parameters and cardiovascular risk factors.
All subjects were older than 21 years of age who visited the Cardiology Outpatient Unit of the Catholic University St. Mary's Hospital or Holy Family Hospital for the first time between 1 January and 31 December 2005. The subjects were referred for evaluation and management of hypertension on the basis of a persistently elevated BP in the outpatient clinic of the Department of Internal Medicine under suspicion of hypertension. We identified all patients who had 1) essential hypertension, defined as an office SBP >140 mmHg and/or an office DBP >90 mmHg, according to the guidelines of the Joint National Committee VII,13) the British Hypertension Society,14) and the European Society of Hypertension,15)16) 2) a 24-hour mean SBP >125 mmHg or a 24-hour mean DBP >80 mmHg15)16) for the exclusion of white coat hypertension; and 3) never previously taken antihypertensive drugs. Patients with diabetes mellitus (DM), hyperlipidemia, and nephropathy (serum creatinine of >1.3 mg/dL in women and >1.5 mg/dL in men) were excluded from the study, as were pregnant women. All eligible patients underwent 24-hour ABPM. Eventually, we studied 346 patients (mean age, 48±12 years; M:F ratio, 175:171).
This study was approved by our Institutional Review Committee. Patients were informed of the investigative nature of the study and written informed consent was obtained before enrollment.
Office BP readings were taken twice in the morning (between 8 and 10 a.m.) by trained nurses using an appropriate sized arm cuff and a mercury sphygmomanometer after a 10-minute rest in the sitting position. The office BP was the average of two consecutive readings.
Twenty-four-hour ABPM was measured using a Pressurometer IV (model 1990A/1991; Del Mar Avionics, Irvine, CA, USA). A cuff for adults was applied to the patient's non-dominant upper arm and the SBP, DBP, and heart rate (HR) were measured automatically every 30 minutes between 6 a.m. and 10 p.m. and every hour between 10 p.m. and 6 a.m. the next day. It was recommended that routine daily life be continued during the ABPM measurement period. All subjects underwent 24-hour ABPM in the morning (between 8 and 10 a.m.) within 3 days after office BP measurement.
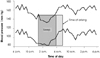
Early morning SBP was defined as the mean SBP reading during the first 2 hours after awakening and the lowest night SBP was the mean SBP reading across 3 consecutive measurements, including the middle value as the lowest SBP reading recorded during the night, as described previously (Fig. 1).10) The morning BP surge was defined as the early morning SBP minus the lowest night SBP >28 mmHg (highest quartile of morning BP surge) in this study.
The subjects were divided into 2 groups based on age (<60 and ≥60 years), and traditional cardiovascular risk factors, such as age, gender, and body mass index {BMI=weight (kg)/height2 (m2); a BMI >25 kg/m2 is considered overweight} were compared with the parameters from the 24-hour ABPM, such as EMBPS, 24-hour mean SBP, 24-hour mean DBP, 24-hour mean mean blood pressure (MBP), 24-hour mean PP, 24-hour mean HR, day-time mean SBP, day-time mean DBP, day-time MAP, day-time PP, day-time HR, night-time mean SBP, night-time mean DBP, night-time MBBP, night-time PP, and night-time HR. The degree of dipping {degree of nocturnal BP dip (%)} was calculated as {(mean day-time MBP-mean night-time MBP)/mean daytime MBP}×100.17)
All data are presented as the means and standard deviations, and statistical analysis was performed using SPSS (version 13.0; SPSS Inc., Chicago, IL, USA). Student's t-test was used for comparison of the measured values from the two groups divided according to age. For correlation of the variables from the 24-hour ABPM, linear and multivariate regression analyses were used. In order to compare the significance among the groups, a chi-square test was used. A p<0.05 was considered statistically significant.
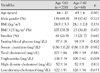
In the groups divided by age, there were 278 subjects <60 years of age (mean, 44±10 years) and 68 subjects ≥60 years of age (mean, 65±4 years) (Table 1). There were no significant differences between the 2 groups in baseline clinical characteristics with respect to traditional cardiovascular risk factors, such as gender, BMI (obesity), and smoking. There were no significant differences between the 2 groups in baseline clinical characteristics with respect to blood chemistry, except serum triglycerides (p<0.05). The younger subjects (<60 years of age) had higher serum triglyceride levels than the older subjects.
The significant differences in 24-hour ABPM parameters for the <60 and ≥60 year-old subject groups were as follows: EMBPS, 18±14 and 24±14 mmHg (p=0.002); 24-hour mean MBP, 102±9 and 105±11 mmHg (p=0.044); 24-hour mean PP, 52±10 and 58±11 mmHg (p<0.001); day-time mean DBP, 90±11 and 85±11 mmHg (p=0.039); day-time mean MBP, 105±9 and 109±11 mmHg (p=0.005); day-time mean PP, 53±10 and 58±11 mmHg (p<0.001); and night-time mean PP, 50±11 and 54±15 mmHg (p<0.001), respectively. These parameters were significantly increased in the older group compared to the younger group. However, the degree of dipping was significantly decreased in the older group (10±8% vs. 7±10%, p=0.002) (Table 2).
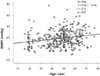
The study subjects exhibited a circadian pattern of BP variation similar to that observed in other studies (Fig. 1).1)2) There was a positive correlation between EMBPS and age (r=0.213, p<0.001) (Fig. 2). However, there was no gender difference in EMBPS (p=0.325) (Fig. 3), and the correlation between EMBPS and BMI was weak and not statistically significant (r=-0.086, p=0.131).
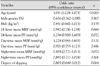
After adjusting for gender, BMI, and the various 24-hour ABPM parameters, age was shown to be an independent risk factor for the highest quartile (>28 mmHg) of EMBPS values (odds ratio, 1.051; 95% confidence interval, 1.028-1.075; p<0.001) (Table 3).
This study is the first to demonstrate that age is correlated with EMBPS (r=0.213, p<0.001) (Fig. 2) and is an independent predictor of EMBPS in patients never-treated for hypertension, after adjusting for gender differences, BMI, and various 24-hour ABPM parameters (odds ratio, 1.051; 95% confidence interval, 1.028-1.075; p<0.001) (Table 3).
The vascular factors that contribute to an increase in cardiovascular events with increasing age, including arterial stiffness, BP, and baroreflex sensitivity, should also be considered from a physiologic perspective. Najjar et al.18) have reported that increasing arterial stiffness and impaired endothelial function are two factors that occur with vascular aging in humans.
Aging is strongly associated with the development of isolated systolic hypertension (widened PP), and is also a stronger predictor of cardiovascular risk in older adults than either DBP or MAP.19) In addition, Laurent et al.20)21) reported that pulse wave velocity, a marker reflecting arterial stiffness that increases with age, is associated with hypertension, and is a cardiovascular risk factor. As SBP rises and DBP falls with stiffness, the increase in PP is an important factor reflecting arterial stiffness.
Many observational studies evaluating the changing pattern of BP with the aging process have shown a concomitant increase in SBP and PP until middle adult life.22) Khattar et al.22) reported that the relative prognostic significance of 24-hour ABPM parameters depends on age; DBP provided the best prognostic value in middle-aged subjects, whereas PP was the most predictive in the elderly (≥60 years of age).
Our data also revealed that PP in particular was significantly increased in the older group compared with the younger group (24-hour mean PP, p<0.001; day-time mean PP, p<0.001; and night-time mean PP, p<0.001) (Table 2).
The relationship between EMBPS and cardiovascular risk has recently become a subject of increasing interest. Although differing in the types of patients assessed and the results obtained, several previous studies have also demonstrated an association between EMBPS and cardiovascular events.10-12)
EMBPS also appears to increase hypertensive heart disease.4) EMBPS was associated with cardiac hypertrophy and common carotid artery intima-media thickenss independent of 24-hour ABPM parameters.23)24)
We investigated the association between 24-hour ABPM parameters, including EMBPS and conventional cardiovascular risk factors. The results (Table 3) (Fig. 2) showed that only EMBPS was associated with age after adjusting for other cardiovascular risk factors and other 24-hour ABPM parameters. Thus, we can exclude the effect of other BP parameters.
An EMBPS is linked to increased target organ damage, as well as stroke and other cardiovascular complications, particularly in elderly patients with hypertension and impaired autoregulation of hypertensive target organ damage.25-28) Once-daily antihypertensive drugs are now widely used. However, even though the medicated hypertensive is well-controlled, it is difficult to know whether the morning hypertension is controlled in the current clinical practice for hypertension. Therefore, 24-hour ABPM or self-measured home BP monitoring targeting EMBPS will achieve more beneficial cardiovascular outcome in elderly patients with hypertension.25) In addition, controlling the EMBPS with antihypertensive drugs might prevent various cardiovascular complications and improve stroke prognosis.10) To reduce the magnitude of the EMBPS notably, it may be necessary for some personalized therapeutic strategies, such as the use of long-acting drugs and the other medications that specially antagonize the morning surge (such as alpha-blockers or blockers of the rennin-angiotensin-aldosterone system).29)30)
Further experimental and clinical studies are necessary to control the EMBPS effectively in elderly patients with hypertension.
This study showed that age is the most important risk factor for EMBPS in 24-hour ABPM. Therefore, we suggest that 24-hour ABPM is needed in elderly patients with hypertension and specific studies targeting EMBPS should be a particular focus for the future.
Figures and Tables
Fig. 1
The early morning surge (EMBPS) is the early morning SBP minus the lowest night SBP. The early morning SBP is the mean SBP during the first 2 hours after awakening. The lowest night SBP is the mean SBP reading across three consecutive measurements, with the middle value the lowest SBP reading recorded during the night. EMBPS: early morning blood pressure surge, SBP: systolic blood pressure.
Acknowledgments
This study was supported by a grant of the Seoul R&BD Program, Republic of Korea (#10526).
References
1. Verdecchia P, Clement D, Fagard R, Palatini P, Parati G. Blood Pressure Monitoring. Task Force III. Target organ damage, morbidity and mortality. Blood Press Monit. 1999. 4:303–317.
2. Mancia G, Zanchetti A, Agabiti-Rosei E, et al. Ambulatory blood pressure is superior to clinic blood pressure in predicting treatment-induced regression of left ventricular hypertrophy. Circulation. 1997. 95:1464–1470.
3. Millar-Craig MW, Bishop CN, Raftery EB. Circadian variation of blood pressure. Lancet. 1978. 1:795–797.
4. Kario K. Caution for winter morning surge in blood pressure: a possible link with cardiovascular risk in the elderly. Hypertension. 2006. 47:139–140.
5. Tofler GH, Brezinski D, Schafer AI, et al. Concurrent morning increase in platelet aggregability and the risk of myocardial infarction and sudden cardiac death. N Engl J Med. 1987. 316:1514–1518.
6. Anwar YA, White WB. Chronotherapeutics for cardiovascular disease. Drugs. 1998. 55:631–643.
7. Clement DL, De Buyzere ML, De Bacquer DA, et al. Prognostic value of ambulatory blood-pressure recordings in patients with treated hypertension. N Engl J Med. 2003. 348:2407–2415.
8. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002. 360:1903–1913.
9. Franklin SS, Larson MG, Khan SA, et al. Does the relation of blood pressure to coronary heart disease risk change with aging? Circulation. 2001. 103:1245–1249.
10. Kario K, Pickering TG, Umeda Y, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation. 2003. 107:1401–1406.
11. Elliott WJ. Circadian variation in the timing of stroke onset: a meta-analysis. Stroke. 1998. 29:992–996.
12. Cohen MC, Rohtla KM, Lavery CE, Muller JE, Mittleman MA. Meta-analysis of the morning excess of acute myocardial infarction and sudden cardiac death. Am J Cardiol. 1997. 79:1512–1516.
13. Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003. 42:1206–1252.
14. Williams B, Poulter NR, Brown MJ, et al. British Hypertension Society guidelines for hypertension management 2004 (BHS-IV): summary. BMJ. 2004. 328:634–640.
15. European Society of Hypertension-European Society of Cardiology Guidelines Committee. 2003 European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens. 2003. 21:1011–1053.
16. O'Brien E, Asmar R, Beilin L, et al. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens. 2003. 21:821–848.
17. O'Brien E, Scheridan J, O'Malley K. Dippers and non-dippers. Lancet. 1988. 2:397.
18. Najjar SS, Scuteri A, Lakatta EG. Arterial aging: is it an immutable cardiovascular risk factor? Hypertension. 2005. 46:454–462.
19. Franklin SS. Pulse pressure as a risk factor. Clin Exp Hypertens. 2004. 26:645–652.
20. Laurent S, Katsahian S, Fassot C, et al. Aortic stiffness is an independent predictor of fatal stroke in essential hypertension. Stroke. 2003. 34:1203–1206.
21. Laurent S, Boutouyrie P, Asmar R, et al. Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension. 2001. 37:1236–1241.
22. Khattar RS, Swales JD, Dore C, Senior R, Lahiri A. Effect of aging on the prognostic significance of ambulatory systolic, diastolic, and pulse pressure in essential hypertension. Circulation. 2001. 104:783–789.
23. Kaneda R, Kario K, Hoshide S, Umeda Y, Hoshide Y, Shimada K. Morning blood pressure hyper-reactivity is an independent predictor for hypertensive cardiac hypertrophy in a community-dwelling population. Am J Hypertens. 2005. 18:1528–1533.
24. Zakopoulos NA, Tsivgoulis G, Barlas G, et al. Time rate of blood pressure variation is associated with increased common carotid artery intima-media thickness. Hypertension. 2005. 45:505–512.
25. Kario K. Time for focus on morning hypertension: pitfall of current antihypertensive medication. Am J Hypertens. 2005. 18:149–151.
26. Kim CH. Ambulatory blood pressure monitoring. Korean Circ J. 1997. 27:1218–1221.
27. Lee SM, Kang HS, Song JS, et al. Study of 24 hour ambulatory blood pressure monitoring in acute stroke patients. Korean Circ J. 1999. 29:1212–1218.
28. Jeon HC, Kim YK, Kim KY, et al. Determinants of left ventricular mass in healthy adults: a study using echocardiography and 24 hour ambulatory blood pressure monitiring. Korean Circ J. 1995. 25:811–819.
29. Head GA, Reid CM, Shiel LM, Jennings GL, Lukoshkova EV. Rate of morning increase in blood pressure is elevated in hypertensives. Am J Hypertens. 2006. 19:1010–1017.
30. Kario K. Morning surge and variability in blood pressure: a new therapeutic target? Hypertension. 2005. 45:485–486.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download