1. Zijlstra F, de Boer MJ, Hoorntje JC, Reiffers S, Reiber JH, Suryapranata H. A comparison of immediate coronary angioplasty with intravenous streptokinase in acute myocardial infarction. N Engl J Med. 1993; 328:680–684. PMID:
8433726.
2. Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003; 361:13–20. PMID:
12517460.
3. Boersma E. Does time matter?: a pooled analysis of randomized clinical trials comparing primary percutaneous coronary intervention and in-hospital fibrinolysis in acute myocardial infarction patients. Eur Heart J. 2006; 27:779–788. PMID:
16513663.
4. Yoon MH, Tahk SJ, Choi SY, et al. Microvascular integrity and ventricular function according to early ST-segment resolution in acute myocardial infarction. Korean Circ J. 2003; 33:183–195.
5. Choi SY, Tahk SJ, Yoon MH, et al. Comparison of TIMI myocardial perfusion grade with coronary flow reserve for prediction of recovery of LV function and LV remodeling in acute myocardial infarction. Korean Circ J. 2004; 34:247–257.
6. Ito H, Okamura A, Iwakura K, et al. Myocardial perfusion patterns related to thrombolysis in myocardial infarction perfusion grades after coronary angioplasty in patients with acute anterior wall myocardial infarction. Circulation. 1996; 93:1993–1999. PMID:
8640973.
7. Kloner RA, Ganote CE, Jennings RB. The 'no-reflow' phenomenon after temporary coronary occlusion in dog. J Clin Invest. 1974; 54:1496–1508. PMID:
4140198.
8. Reffelmann T, Kloner RA. The 'no-reflow' phenomenon: basic science and clinical correlates. Heart. 2002; 87:162–168. PMID:
11796561.
9. Gibson CM, Schomig A. Coronary and myocardial angiography: angiographic assessment of both epicardial and myocardial perfusion. Circulation. 2004; 109:3096–3105. PMID:
15226226.
10. Fearon WF, Faroque HM, Balsam LB, et al. Comparison of coronary thermodilution and Doppler velocity for assessing coronary flow reserve. Circulation. 2003; 108:2198–2200. PMID:
14568891.
11. Lim HS, Tahk SJ, Yoon MH, et al. A novel index of microcirculatory resistance for invasively assessing myocardial viability after primary angioplasty for treating acute myocardial infarction. Korean Circ J. 2007; 37:318–326.
12. Matetzky S, Novikov M, Gruberg L, et al. The significance of persistent ST elevation versus early resolution of ST segment elevation after primary PTCA. J Am Coll Cardiol. 1999; 34:1932–1938. PMID:
10588206.
13. Kobayashi N, Ohmura N, Nakada I, et al. Further ST elevation at reperfusion by direct percutaneous transluminal coronary angioplasty predicts poor recovery of left ventricular systolic function in anterior wall AMI. Am J Cardiol. 1997; 79:862–866. PMID:
9104895.
14. Schroder R, Wegscheider K, Schroder K, Dissmann R, Meyo-Sabellek W. Extent of early ST segment elevation resolution: a strong predictor of outcome in patients with acute myocardial infarction and a sensitive measure to compare thrombolytic regimens. J Am Coll Cardiol. 1995; 26:1657–1664. PMID:
7594100.
15. de Lemos JA, Braunwald E. ST segment resolution as a tool for assessing the efficacy of reperfusion therapy. J Am Coll Cardiol. 2001; 38:1283–1294. PMID:
11691496.
16. Sclarovsky S, Mager A, Kusniec J, et al. Electrocardiographic classification of acute myocardial ischemia. Isr J Med Sci. 1990; 26:525–531. PMID:
2228566.
17. The TIMI Study Group. The Thrombolysis in Myocardial Infarction (TIMI) trial: phase I findings. N Engl J Med. 1985; 312:932–936. PMID:
4038784.
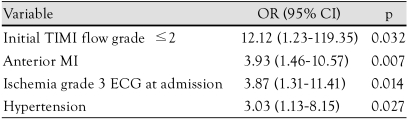
18. An SG, Oh JH, Park TI, et al. Risk factors for reflow disturbance phenomenon during percutaneous coronary intervention in patients with acute myocardial infarction. Korean J Med. 2008; 74:16–22.
19. Matetzky S, Novikov M, Gruberg L, et al. The significance of persistent ST elevation versus early resolution of ST segment elevation after primary PTCA. J Am Coll Cardiol. 1999; 34:1932–1938. PMID:
10588206.
20. Galiuto L. Optimal therapeutic strategies in the setting of post-infarct no reflow: the need for a pathogenetic classification. Heart. 2004; 90:123–125. PMID:
14729769.
21. De Luca G, Ernst N, Zijlstra F, et al. Preprocedural TIMI flow and mortality in patients with acute myocardial infarction treated by primary angioplasty. J Am Coll Cardiol. 2004; 43:1363–1367. PMID:
15093868.
22. De Luca G, Maas AC, Suryapranata H, et al. Prognostic significance of residual cumulative ST-segment deviation after mechanical reperfusion in patients with ST-segment elevation myocardial infarction. Am Heart J. 2005; 150:1248–1254. PMID:
16338267.
23. Stone GW, Brodie BR, Griffin JJ, et al. Prospective, multicenter study of the safety and feasibility of primary stenting in acute myocardial infarction: in-hospital and 30-day results of the PAMI stent pilot trial. J Am Coll Cardiol. 1998; 31:23–30. PMID:
9426013.
24. Stone GW, Brodie BR, Griffin JJ, et al. Clinical and angiographic follow-up after primary stenting in acute myocardial infarction. Circulation. 1999; 99:1548–1554. PMID:
10096929.
25. McLaughlin MG, Stone GW, Aymong E, et al. Prognostic utility of comparative methods for assessment of ST-segment resolution after primary angioplasty for acute myocardial infarction. J Am Coll Cardiol. 2004; 44:1215–1223. PMID:
15364322.
26. Brodie BR, Stuckey TD, Hansen C, et al. Relation between electrocardiographic ST-segment resolution and early and late outcomes after primary percutaneous coronary intervention for acute myocardial infarction. Am J Cardiol. 2005; 95:343–348. PMID:
15670542.
27. Birnbaum Y, Herz I, Sclarovsky S, et al. Prognostic significance of the admission electrocardiogram in acute myocardial infarction. J Am Coll Cardiol. 1996; 27:1128–1132. PMID:
8609331.
28. Birnbaum Y, Goodman S, Barr A, et al. Comparison of primary coronary angioplasty versus thrombolysis in patients with ST-segment elevation acute myocardial infarction and grade II and grade III myocardial ischemia on the enrollment electrocardiogram. Am J Cardiol. 2001; 88:842–847. PMID:
11676944.
29. Wolak A, Yaroslavtsev S, Amit G, et al. Grade 3 ischemia on the admission electrocardiogram predicts failure of ST resolution and of adequate flow restoration after primary percutaneous coronary intervention for acute myocardial infarction. Am Heart J. 2007; 153:410–417. PMID:
17307421.
30. Kunadian B, Dunning J, Vijayalakshmi K, Thornley AR, de Belder MA. Meta-analysis of randomized trials comparing anti-embolic devices with standard PCI for improving myocardial reperfusion in patients with acute myocardial infarction. Catheter Cardiovasc Interv. 2007; 69:488–496. PMID:
17286249.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download