Abstract
Background and Objectives
Left transradial coronary angiography may result in damage of both radial arteries in patients who experienced right radial access. In some patients, the left radial artery has been used as a graft. We investigated whether graft angiography using right radial access is feasible in patients with bypass surgery to preserve the left radial artery as a future graft.
Subjects and Methods
A total of 109 consecutive patients with bypass surgery who had undergone right radial access underwent graft angiography via the same access.
Results
Sixteen (15%) patients were excluded because of the presence of a severely tortuous right subclavian artery. Bypass graft angiography via right radial or brachial access was completed successfully in 90 (97%) out of 93 patients. In 3 (3%) of patients, femoral access was needed to complete the angiography. Saphenous vein grafts were cannulated selectively in 150 (90%) of 167 grafts with satisfactory image quality and not found even on the aortogram in the other 17 (10%) grafts. Ninety-two (89%) out of 103 left mammary grafts were cannulated selectively or semi-selectively using a modified Simmons catheter, resulting in satisfactory image quality. The other 11 (11%) grafts were visualized non-selectively using a Judkins Left catheter, and resulting in acceptable image quality in 10 (91%) grafts. There were no procedure-related complications.
With the advancement of technology and equipment, transradial coronary angiography and intervention causes less risk of developing local vascular complications, makes patients more comfortable, and makes ambulation possible at an early stage following the procedure.1-3) Due to these advantages, it has been performed frequently in Korea as well as in overseas countries.4-7) Besides, transradial vascular access has an extended role in angiography or in interventions of the vertebral artery,8-13) abdominal aorta or renal artery.14)15) In the angiography or intervention of coronary artery, a right transradial approach is commonly selected because it is advantageous in that equipments are easily manipulated or accustomed.16) Besides, in doing angiography in patients who previously had bypass surgery, the left transradial approach is favored because it makes it easier to insert a catheter for a left mammary graft and to perform the angiography.17)18)
With the increased use of the radial artery as a graft vessel, however, other problems have been reported. That is, the left radial artery had already been used as a graft vessel in some patients and the selection of a left radial approach is impossible. Also, if a left radial approach was taken in patients who underwent angiography via a right radial approach, both radial arteries would be damaged, although both arteries are the key source for a graft vessel in cases in which revision bypass surgery is needed. In this view, if patients who previously underwent coronary bypass surgery had also undergone coronary angiography via a right radial approach, it would be a wise choice to avoid a left radial approach for angiography of native coronary artery and bypass graft vessels.19)
Given the above background, we examined the possibility of doing angiography of bypass graft vessels via a repeated right radial approach performed to preserve the left radial artery in patients who previously underwent coronary angiography via a right radial approach.
Of those who underwent coronary bypass surgery at our institution during the period from January 1999 to December 2004, we identified and enrolled into the current study 109 patients who underwent preoperative coronary angiography via a right radial approach. Via a repeated right radial approach, we did angiography of the native coronary artery and bypass graft vessels.
The only exclusion criterion for a repeated right radial approach was the presence of severe tortuosity of the right subclavian artery during a right radial approach that was performed for the first time prior to the surgery. There are no clear definitions of the degree of tortuosity of the right subclavian artery. Therefore, severe tortuosity of the right subclavian artery was arbitrarily defined. It was defined as cases where the most rigid, third guidewire was essential for successful passage and manipulation in addition to a polytetrafluoro ethylene (PTFE)-coated guidewire with a J-shaped tip and a flexible hydrophilic guidewire.20) Before embarking on the study, patients submitted written informed consent for the procedure.
Following cannulation of the right radial artery, a 5-Fr sheath (MAXIMUM™ hemostasis introducer set, DAIG, USA) was inserted in the radial artery. A saline solution containing nitroglycerin (200 ug), verapamil (2 mg), and heparin (5,000 units) was infused through an inducer tube via its side port. In cases in which no pulse was perceived from the radial artery and an arterial puncture became a failure, a right brachial approach was attempted.
First, angiography of the native coronary artery was performed. An angiogram of the saphenous vein grafts was performed in accordance with standard sequences such as 5 Fr Amplatz Right, Amplatz Left, or Right Coronary Bypass (RCB) or Left Coronary Bypass (LCB) catheters. An angiogram of the left mammary artery graft was performed using a Judkins Left catheter in a non-selective manner in the early stage of the study period. A Judkins Left 3.5 catheter was placed according to its original curvature within the ascending aorta and then retracted. Meanwhile, it was rotated in a clockwise manner. Then, a catheter was placed in the proximal part of the left subclavian artery.21) Thereafter, by adjusting the tip of the catheter, the catheter was advanced towards the origin of the left mammary artery as much as possible. A cuff of the sphygmomanometer surrounded the left forearm and then was inflated to a pressure of approximately 200 mmHg. Approximately 6-8 mL of contrast medium was strongly infused into the catheter in a hand-assisted manner.
In the late-stage of the study period, with the use of a modified Simmons catheter (Jung Sung co., Seoul, Korea) (Fig. 1) which was prepared by bending the tip of a catheter, selective angiography of the left mammary artery graft was performed. Within the ascending aorta, attempts were made to make the tip of the catheter placed superiorly. Then, the catheter was pulled gradually and then rotated in a clockwise manner. Thus, it progressed within the left subclavian artery.22) The catheter was further pulled and thereby its tip reached the ostium of the left mammary artery. Then, it was rotated in a clockwise direction and then placed within the left mammary artery. In cases in which selective cannulation was difficult at the ostium of the left mammary artery, angiography was performed under the status of a semi-selective cannulation where the tip of the catheter was directed to the ostium of the left mammary artery.
On angiography, the image quality was assessed based on criteria that were proposed by Bhatt et al.22) In cases in which the major part of grafted vessels including the anastomosis site and the distal blood vessels were completely visualized, satisfactory outcomes were determined.
Clinical and angiographic characteristics of all 109 patients are shown in Table 1. Mean age was 61±6 years and the number of male patients was 78 (72%). Indications for angiography included an assessment of graft vessels following bypass surgery in 47 patients (43%), stable angina in 27 patients (25%), unstable angina in 14 patients (13%), and atypical chest pain in 21 patients (19%). The mean time difference between bypass surgery and angiography was 410±603 days (range: 7-2,481 days). Forty patients (37%) visited our outpatient clinic and then underwent angiography. On the day of angiography, they were discharged.
In 16 patients (15%), there was a severe tortuosity of the right subclavian artery at the right radial approach prior to the bypass surgery. These patients were therefore excluded from the current study where a repeated right radial approach was needed. Instead, a femoral approach was used for angiography. Following the bypass surgery, which was conducted in 93 patients, a repeated right radial approach was attempted in 85 (94%) of 90 patients (97%) following the bypass surgery and a right brachial approach was attempted in five patients (6%). Thus, angiography of graft vessels was successfully performed. In three patients (3%), complete angiography of the graft vessels was difficult via the right radial approach. In these patients, it was converted to a femoral approach and thereby a complete angiography of the graft vessels was achieved.
For native coronary angiographies, 20 patients (18%) had two-vessel disease, 62 (57%) three-vessel diseases, and 27 (25%) left main disease. Mean left ventricular ejection fraction was 54±6%.
Of a total of 167 grafts of the saphenous vein, in 150 (90%) selective cannulation and angiography was possible using an Amplatz Right or Left catheter or an RCB or LCB catheter. The ostia of the remaining 17 grafts (10%) could not be identified due to a lack of a mark ring. Also, the ostia could not be observed on angiography of the ascending aorta. In the overall grafts for which a selective cannulation was performed, satisfactory images were obtained (Fig. 2).
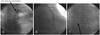
Of a total of 103 grafts of the left mammary artery, in 92 (89%) a selective cannulation (64 grafts, 70%) or a semi-selective one (28 grafts, 30%) were possible (Fig. 3). In all the grafts, satisfactory images were obtained. In the early stage of the study period, a non-selective angiography was performed using a Judkins Left catheter in the remaining 11 grafts (11%), of which satisfactory images were obtained in ten grafts (91%) (Fig. 4). In all left mammary artery grafts, the grafts were patent and blood flow was "fair". There were no cases in which an intervention was needed.
We found that angiography of the native coronary artery and bypass graft vessels can be successfully done in most patients who underwent coronary bypass surgery and in whom there is a lack of severe tortuosity of the right subclavian artery. The current study is the first one that systematically examined the feasibility of doing angiography of graft vessels via a right radial approach in patients who underwent coronary bypass surgery. In patients who underwent coronary bypass surgery in whom a femoral approach was difficult or impossible despite the necessity of invasive angiography, or those in whom the left radial artery must be preserved, a right radial approach for angiography is an alternative.
In patients who underwent coronary artery bypass graft surgery, angiography of the native coronary artery and graft vessels is done via a femoral approach as the standard method.24) In cases in which the angiography is performed via the vessels of the upper extremities, a left-sided vascular approach is favored because it makes it easier to cannulate the left mammary artery graft. In patients who underwent coronary bypass surgery and in whom an angiography was performed via a right radial approach prior to the surgery, however, a left radial approach would damage the left radial artery and both the left and right radial arteries would be damaged. This would be unfortunate because both arteries could otherwise be used as graft vessels in cases in which further bypass surgery is needed. Also, the left radial artery was already used as a bypass graft in some patients. It is therefore unwise to attempt a left radial approach.
There are almost no available data about whether angiography was done via a right radial approach in patients who underwent coronary bypass surgery. This might be because angiography of left mammary artery grafts can not easily be performed via the right radial artery. According to a study using a mammary catheter,25) angiography of left mammary artery grafts was successfully performed via a right radial approach in ten (77%) of 13 patients although a relatively longer procedure time of 32±4 minutes was needed. According to studies using a Judkins Left JL-3.5 catheter21) or a modified Simmons catheter,22) however, angiography of the left mammary artery via a right radial approach was performed with higher success rates of 98% and 100%, respectively, and with a shorter procedure time -11±8 second and 233±168 second, respectively. In the current study, this angiographic technique was extensively applied to patients who underwent bypass surgery in whom there was a lack of severe tortuosity of the right subclavian artery. Angiography of the left mammary artery grafts was performed using a modified Simmons catheter. According to the current study, a selective or a semi-selective cannulation was possible in 92 (89%) of 103 grafts (Fig. 3). It can also be inferred, however, that the anatomical factors, including the location of the ostium and the degree of proximal curvature of the left subclavian artery, and the location and direction of the ostium of the left mammary artery as well as the presence of severe tortuosity of the right subclavian artery, would affect a selective cannulation of the left mammary artery graft. According to the current study, in cases in which a Judkins Left catheter was used, ten (91%) of 11 grafts showed a satisfactory imaging quality (Fig. 4). In these cases, however, there is the limitation that a non-selective visualization is the only measure that can be used. In the current study, angiography of saphenous vein grafts via the right radial artery was done using an Amplatz Right (AR-2) or Left (AL-1) catheter. In a study that was conducted by Louvard et al.,17) angiography was performed using a Judkins Right or Multipurpose catheter.
One limitation of the current study is that no controlled studies were conducted using a standard femoral approach. Recent years have introduced the protocol that patients can be discharged on the day following prompt hemostasis after an angiography was done in patients who underwent bypass surgery via the femoral artery with the use of a 5- or 6-Fr catheter. Also, there are limits to doing angiography via a repeated radial artery in patients who underwent bypass surgery, and these must be seriously considered. In cases in which grafts of bilateral mammary arteries were used, the angiography can be performed in a problem-free manner. In cases in which a graft of the gastroepiploic artery was used, however, the radial approach can not be made.26) In these cases, it must therefore be confirmed whether this graft can be used. Second, the presence of severe tortuosity of the right subclavian artery affects the manipulation of the catheter that is used for the passage of a catheter and a selective cannulation. One must therefore examine whether there is a severe tortuosity of the right subclavian artery when a right radial approach is first attempted. In cases in which a right radial approach was first planned in patients who underwent bypass surgery, a serious determination should be made following a close examination of the predictors associated with the presence of severe tortuosity of the right subclarian artery.20) Third, in patients who have undergone a radial approach even once, the failure rate of arterial puncture is increased due to the decreased or lost radial arterial pulse. Following the repeated use of a radial approach, the rate of the disappearance of the radial artery pulse is increased.27-29) Finally, there is a modified Simmons catheter whose tip was designed specifically for the current study, but is not commercially available. If the design of this modified Simmons catheter were further advanced, and came in variable lengths, selective cannulation would become easier.
In conclusion, the current study shows that angiography of bypass surgery grafts via a repeated right radial approach can be successfully performed in most patients who have no severe tortuosity of the right subclavian artery. This procedure could be used as one of the alternative approaches for angiography in patients who underwent coronary bypass surgery and in whom a femoral approach is difficult or impossible despite the necessity of invasive angiography or for those in whom the left radial artery must be preserved (Fig. 5).
Figures and Tables
Fig. 1
Modified Simmons catheters with a newly angled tip and 3 different curve lengths (7.5 cm, 7.7 cm, and 8.5 cm).22)
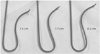
Fig. 2
Selective angiography of saphenous vein grafts with Amplatz Left (AL) and Right (AR) catheters.
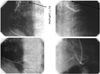
Fig. 3
Semi-selective angiography of a left mammary graft with a modified Simmons catheter. Although the catheter tip is not cannulated selectively (arrow, A), the image quality is excellent in the anastomosis site (B) and collateral vessel (arrow, C).
References
1. Cooper CJ, El-Shiekh RA, Cohen DJ, et al. Effect of transradial access on quality of life and cost of cardiac catheterization: a randomized comparison. Am Heart J. 1999. 138:430–436.
2. Louvard Y, Lefevre T, Allain A, Morice M. Coronary angiography through the radial or the femoral approach: the CARAFE study. Catheter Cardiovasc Interv. 2001. 52:181–187.
3. Kiemeneij F, Laarman GJ, Odekerken D, Slagboom T, van der Wieken R. A randomized comparison of percutaneous transluminal coronary angioplasty by the radial, brachial and femoral approaches: the access study. J Am Coll Cardiol. 1997. 29:1269–1275.
4. Yoon J, Lee SH, Kim JY, et al. The experience of trans-radial coronary intervention in Wonju. Korean Circ J. 1998. 28:1443–1451.
5. Kim MH, Cha KS, Kim JS. Transradial interventions in coronary artery disease: comparison with transfemoral interventions. Korean Circ J. 1998. 28:1941–1952.
6. Kim PH, Gwon HC, Kim YH, et al. The safety and feasibility in trans-radial coronary interventions for chronic total occlusion. Korean Circ J. 2004. 34:767–774.
7. Park SJ, Park JH, Lee JH, et al. The clinical feasibility of transradial primary percutaneous coronary intervention with an ST elevation acute myocardial infarction. Korean Circ J. 2007. 37:72–77.
8. Cha KS, Kim MH, Kim YD, Kim JS. Combined right transradial coronary angiography and selective carotid angiography: safety and feasibility in unselected patients. Catheter Cardiovasc Interv. 2001. 53:380–385.
9. Yoo BS, Lee SH, Kim JY, et al. A case of transradial carotid stenting in a patient with total occlusion of distal abdominal aorta. Catheter Cardiovasc Interv. 2002. 56:243–245.
10. Iwasaki S, Yokoyama K, Takayama K, et al. The transradial approach for selective carotid and vertebral angiography. Acta Radiol. 2002. 43:549–555.
11. Fessler RD, Wakhloo AK, Lanzino G, Guterman LR, Hopkins LN. Transradial approach for vertebral artery stenting: technical case report. Neurosurgery. 2000. 46:1524–1527.
12. Matsumoto Y, Hongo K, Toriyama T, Nagashima H, Kobayashi S. Transradial approach for diagnostic selective cerebral angiography: results of a consecutive series of 166 cases. AJNR Am J Neuroradiol. 2001. 22:704–708.
13. Levy EI, Boulos AS, Fessler RD, et al. Transradial cerebral angiography: an alternative route. Neurosurgery. 2002. 51:335–340.
14. Cowling MG, Buckenham TM, Belli AM. The role of transradial diagnostic angiography. Cardiovasc Intervent Radiol. 1997. 20:103–106.
15. Galli M, Tarantino F, Mameli S, et al. Tranradial approach for renal percutaneous transluminal angioplasty and stenting: a feasibility pilot study. J Invasive Cardiol. 2002. 14:386–390.
16. Wu CJ, Lo PH, Chang KC, Fu M, Lau KW, Hung JS. Transradial coronary angiography and angioplasty in Chinese patients. Cathet Cardiovasc Diagn. 1997. 40:159–163.
17. Louvard Y, Krol M, Pezzano M, et al. Feasibility of routine transradial coronary angiography: a single operator's experience. J Invasive Cardiol. 1999. 11:543–548.
18. Mann T, Raza JA, Whitlock CH, Arrowood M. Transradial management of saphenous vein bypass graft disease using rheolytic thrombectomy and coronary stenting. J Invasive Cardiol. 2003. 15:221–223.
19. Saito S. Right or left side? Catheter Cardiovasc Interv. 2003. 58:305.
20. Cha KS, Kim MH, Kim HJ. Prevalence and clinical predictors of severe tortuosity of right subclavian artery in patients undergoing transradial coronary angiography. Am J Cardiol. 2003. 92:1220–1222.
21. Cha KS, Kim MH, Hung JS, Woo JS, Kim YD, Kim JS. Nonselective left internal mammary artery angiography during right transradial coronary angiography: a simple, rapid and safe technique. Angiology. 2001. 52:773–779.
22. Cha KS, Kim MH. Feasibility and safety of concomitant left internal mammary arteriography at the setting of the right transradial coronary angiography. Catheter Cardiovasc Interv. 2002. 56:188–195.
23. Bhatt SN, Jorgensen MB, Aharonian VJ, Mahrer PR. Nonselective angiography of the internal mammary artery: a fast, reliable, and safe technique. Cathet Cardiovasc Diagn. 1995. 36:194–198.
24. Kuntz RE, Baim DS. Internal mammary angiography: a review of technical issues and newer methods. Cathet Cardiovasc Diagn. 1990. 20:10–16.
25. Louvard Y. Marco J, Fajadet J, Henry M, Amor M, editors. Graft angiography via the right transradial approach. Endovascular Therapy Course Coronary And Peripheral: Ninth Complex Coronary Angioplasty Course Book. 1998. Paris: Europa;325–327.
26. Sharma GL, Louvard Y, Tavolaro O, et al. Less invasive PTCA of a gastroepiploic artery combining the transradial approach and 5 Fr guiding catheter: a case report. Catheter Cardiovasc Interv. 2002. 56:494–497.
27. Caputo RP, Simons A, Giambartolomei A, et al. Safety and efficacy of repeat transradial access for cardiac catheterization procedures. Catheter Cardiovasc Interv. 2001. 54:188–190.
28. Yoo BS, Lee SH, Ko JY, et al. Procedural outcomes of repeated transradial coronary procedure. Catheter Cardiovasc Interv. 2003. 58:301–304.
29. Wakeyama T, Ogawa H, Iida H, et al. Intima-media thickening of the radial artery after transradial intervention: an intravascular ultrasound study. J Am Coll Cardiol. 2003. 41:1109–1114.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download