Introduction
Postcardiac injury syndrome (PCIS) refers to a generalized inflammatory reaction to various types of myocardial injuries. The characteristic features of PCIS are pleuritic chest pain, low-grade fever, an abnormal chest X-ray, and the presence of exudative pericardial or pleural effusions.1) PCIS includes postmyocardial infarction syndrome, postcommissurotomy syndrome, and postpericardiotomy syndrome. This syndrome also has been observed after percutaneous intervention, pacemaker implantation, and radiofrequency catheter ablation.2)3)
Acute myocardial infarction (AMI) and percutaneous coronary intervention (PCI) are two causes of PCIS, but cases with presenting features of acute mediastinitis are extremely rare. We report a rare case of PCIS after PCI for AMI in which the presenting clinical features were characteristic of acute mediastinitis.
Case
A 41-year-old male with a history of cigarette smoking sought evaluation at the emergency room due to pain in the anterior chest and epigastrium of 35 hours duration. At the time of onset of the chest pain, he was isolated on an island and unable to access transportation for transfer to the hospital. On registration in the emergency department, the patient's vital signs were as follows: temperature, 37.1℃; heart rate, 116 beats per minute; blood pressure, 130/90 mmHg; and pulse oximetry, 98% on room air. The electrocardiogram (ECG) showed marked ST segment elevation in the precordial leads (Fig. 1). The results of laboratory tests were notable for a white blood cell count of 1,7540/mm3 and elevated cardiac biomarkers. The C-reactive protein was elevated to 151.54 mg/dL. An echocardiographic examination revealed akinesia of the left ventricular septum and severe left ventricular dysfunction. He subsequently underwent coronary angioplasty and stenting of the left anterior descending artery using two sirolimus-eluting stents (Fig. 2).
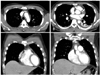
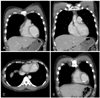
One day after the PCI, the patient complained of severe pleuritic chest pain radiating to both shoulders and the lower jaw. On physical examination, pericardial friction rubs and a crunching sound were heard over the precordium. The erythrocyte sedimentation rate was elevated to 120 mm/h. A repeat echocardiogram was performed, and the results were unchanged. Computed tomography (CT) showed small gas bubbles around the aortic wall and mild pericardial thickening with subtle air densities suggesting acute mediastinitis (Fig. 3). Based on these results, the patient was diagnosed with PCIS and acute mediastinitis, and was given oral ibuprofen and broad-spectrum intravenous antibiotics (ceftriaxone, aminoglycoside, and lingcosimide). The patient began to feel some subjective improvement within 24 hours and the pericardial friction rub was no longer heard on physical examination. The antibiotics were terminated on the 6th day. A chest CT was repeated; the previously noted soft tissue density lesion surrounding the ascending aortic wall and the subtle streaky fatty infiltrations with small gas bubbles had resolved. However, multiple low-density nodules were noted in the apex of the left ventricle, suggesting acute thrombi (Fig. 4). Thus, intravenous heparin with oral warfarin treatment was started. The patient was discharged from the hospital on the day 17 with persistent apical mural thrombi.
Discussion
PCIS was first described in 1953 following mitral commissurotomy.4) In 1956, Dressler5) reported the development of PCIS in a patient after a myocardial infarction (MI). Dressler's syndrome or postmyocardial infarction syndrome pertains to patients who develop PCIS after MI.5) Dressler's syndrome is usually a late complication developing weeks-to-months after an acute MI, but rarely may be evident within the first week following a MI. A similar syndrome has been reported following PCIs, pericardiotomy, radiofrequency catheter ablation, and chest trauma.2)3)6)7) Although there are some records to suggest an immunologic or viral origin for PCIS, the causes of PCIS remain uncertain.1) Immunologic factors are considered to be of primary importance in PCIS.1)8)9) Therefore, the presumptive pathogenic sequence begins with a myocardial injury, which releases cardiac antigens and stimulates antibody formation. Immune complexes are generated and accumulate in the pericardium, pleura, and lungs. Finally, the inflammatory response occurs. Kennedy et al.9) reported that studies in patients undergoing cardiac surgery have revealed a statistically significant correlation between the postoperative to preoperative ratios of actin and myosin antibodies and the clinical occurrence of PCIS.
The clinical manifestations of PCIS include malaise, pleuritic chest pain, a pericardial friction rub, and high fever. Pleural or pericardial effusions are characteristic findings and the erythrocyte sedimentation rate is generally high.
Although PCIS has been reported after minor cardiac procedures, such as pacemaker implantation, PCIS has rarely been reported after coronary angioplasty. Valander and colleagues2) described a case of PCIS in which Dressler's syndrome developed after an extensive MI.2) More recently, Hearne et al.10) reported a case of PCIS 3 weeks after coronary intervention.
Prior to the development of cardiovascular surgery, most cases of mediastinitis arose from esophageal perforation or contiguous spread of odontogenic or retropharyngeal infections. In modern practice, however, most cases of mediastinitis are complications of cardiovascular or thoracic surgical procedures.11-13) The radiologic hallmark of non-postoperative mediastinitis is mediastinal widening on chest X-ray. Other rare abnormalities include air fluid levels in the mediastinum or subcutaneous tissue, and mediastinal air on lateral chest radiographs. A CT diagnosis of mediastinitis is based on the presence of mediastinal air and fluid collections with or without peristernal abnormalities, such as soft tissue edema or sternal separation.14-16)
The case presented herein showed that PCIS occurred within a few days of an AMI, and that the clinical condition was similar in appearance to acute mediastinitis. Indeed, PCIS rarely occurs several days after an AMI. Moreover, it has never been reported that PCIS presenting as mediastinitis occurs after an AMI.
Our case is the first case of PCIS presenting as acute mediastinitis. One should consider this diagnosis after coronary angioplasty when the patient develops sudden chest pain and if the chest CT reveals pericardial thickening with small gas bubbles.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download