Abstract
Background and Objectives
The antihypertensive efficacy and tolerability of losartan (LST) in fixed combination with hydrochlorothiazide (HCTZ) has not been compared to those of amlodipine monotherapy in Asians. This is an important comparison to draw, because Asians have been suggested to respond more favorably to calcium channel blockers and less favorably to angiotensin-converting enzyme inhibitors in comparison to Westerners. We sought to compare these two regimens in Korean patients with mild to moderate hypertension.
Subjects and Methods
174 patients were randomized to receive LST 50 mg once daily, which could be titrated to LST/HCTZ 50/12.5 mg at 4 weeks, followed by 100/25 mg at 8 weeks; or to receive amlodipine besylate 2.5 mg once daily, which could be titrated to 5 mg at 4 weeks, followed by 10 mg at 8 weeks to achieve diastolic blood pressure <90 mmHg.
Results
At 12 weeks, the differences between the LST/HCTZ and amlodipine groups with regard to diastolic and systolic blood pressure were 1.2 mmHg (95% confidence interval: -1.1 to 3.4) and -0.5 mmHg (95% confidence interval: -4.3 to 3.4), respectively. The rates of achieving systolic blood pressure <140 mmHg were 66.7% in the LST/HCTZ group and 75.9% in the amlodipine group (p=0.20). The rates of drug-related adverse events were 15.6% in the LST/HCTZ group and 11.9% in the amlodipine group (p=0.49).
In most hypertensive patients, two or more drugs are required to achieve target blood pressure goals.1) In this respect, combinations of two drugs in a single tablet (i.e., fixed combinations) carry the advantages of increased compliance and cost-effectiveness.2)3) Thus, their market share is rapidly increasing. Among the various fixed combinations of antihypertensive drugs, those of angiotensin II receptor blockers (ARBs) and hydrochlorothiazide (HCTZ) are most widely used because of their synergism in antihypertensive efficacy, as well as their counterbalance of side effects.4)5)
There have been several studies comparing the antihypertensive efficacy and tolerability of a fixed combination of losartan (LST) (the first of the ARBs) and HCTZ with those of amlodipine besylate in Westerners.6-9) However, these is little data in Asians, who have been suggested to respond more favorably to calcium channel blockers and less favorably to angiotensin-converting enzyme inhibitors compared to Westerners.10) In this study, we compared the antihypertensive efficacy and tolerability of a fixed combination of LST and HCTZ with those of amlodipine besylate monotherapy in Korean patients with mild to moderate hypertension.
This study was performed with a multi-centre, randomized, open-label, parallel-group design at six sites in the Republic of Korea. The study protocol was reviewed and approved by the institutional review board at each site.
The study consisted of initial screening, a 2-week washout period, and a 12-week active treatment period. Outpatients from 20 to 75 years of age with uncomplicated, essential hypertension were eligible for the study. All patients delivered informed consent before entering the study. Complete medical history, physical examination, and laboratory tests were evaluated during the initial screening.
After the 2-week washout period, patients whose baseline sitting diastolic blood pressure (SiDBP) was between 90 and 114 mmHg were randomized to receive either LST 50 mg once daily for the LST/HCTZ group or amlodipine besylate 2.5 mg once daily for the amlodipine group. To achieve SiDBP <90 mmHg, regimens could be titrated to LST/HCTZ 50/12.5 mg at 4 weeks, followed by 100/25 mg at 8 weeks in the LST/HCTZ group. Similarly, in the amlodipine group, amlodipine besylate could be titrated to 5 mg at 4 weeks followed by 10 mg at 8 weeks. The treatment schedule is summarized in Fig. 1.
At each visit, sitting systolic blood pressure (SiSBP), SiDBP, and pulse rate were measured. Blood pressure was measured at the same time of the day, before dosing, in the same arm, and by the same investigator, at each center, with mercury sphygmomanometers manufactured by one company (W. A. Baum Co. Inc, New York, U.S.A.).11) At each visit, patients were asked about adverse events (AEs).
The primary efficacy variable was the difference in the mean change of SiDBP between the two groups at 12 weeks. The secondary efficacy variables included the difference in the mean change of SiSBP; the mean change of SiDBP, SiSBP, and pulse rates; and the response rate defined as the proportion of patients whose SiSBP was <140 mmHg at 12 weeks.
Tolerability was assessed based on the incidence of overall (reported by the patients) or drug-related (adjudicated by the investigators) AEs, expressed as the proportion of patients reporting one or more AEs. The mean change in laboratory measures at 12 weeks was also assessed, including serum uric acid levels.
For the comparison of the two groups, the prespecified boundary for non-difference in the mean change of SiDBP was defined as [-6, 6] mmHg. Assuming the between-group difference in the mean change of SiDBP as 6.0 mmHg, with a standard deviation of 10 mmHg and an exclusion rate of 30%, we calculated that 88 patients per treatment group would provide 90% power to detect a statistically significant difference with a 2-sided α level of 0.05. Efficacy variables were compared using the analysis of covariance test. The pattern of serial changes in blood pressure through 4, 8, and 12 weeks was compared using the repeated measures analysis of variance test.
The efficacy measures were analyzed in two populations. The intention-to-treat (ITT) population included the patients who had received at least 1 dose of the study drug after randomization, had valid baseline data, and had at least 1 valid post-baseline data. On ITT analysis, any missing post-randomization measures were estimated by carrying forward the last observed data. The per-protocol (PP) population included only those patients who had completed the 12-week treatment schedule and whose drug compliance was 75% or better. Tolerability measures were analyzed in the ITT population, which included all patients who took at least 1 dose of the study drug. The incidence of AEs was compared between the two groups using the chi-square or Fisher's exact test, where appropriate.
After the 2-week washout period, 176 patients were randomly assigned to the LST/HCTZ group (n=90) or the amlodipine group (n=84). The baseline characteristics of the two groups are summarized in Table 1. During the active treatment period, 11 patients (12.2%) in the LST/HCTZ group and 11 patients (13.1%) in the amlodipine group dropped out of the study. At 12 weeks, 46 (58.2%), 19 (24.1%), and 14 (17.7%) patients in the LST/HCTZ group were treated with LST 50 mg, LST/HCTZ 50/12.5 mg, and 100/25 mg, respectively. In the amlodipine group, 33 (45.2%), 28 (38.4%), and 12 (16.4%) patients were treated with amlodipine besylate 2.5 mg, 5 mg, and 10 mg, respectively. Fig. 2 depicts the dose titration status of the two groups at 12 weeks. Drug compliance was comparable between the two treatment groups.
The number of patients whose drug compliance was 75% or better was 77 (85.6%) in the LST/HCTZ group and 72 (85.7%) in the amlodipine group.
In the ITT population (n=160), SiDBP was significantly reduced at 12 weeks by 11.6 mmHg {95% confidence interval (CI): 10.1 to 13.2} in the LST/HCTZ group and by 12.8 mmHg (95% CI: 11.2 to 14.4) in the amlodipine group (p<0.001 for both groups). However, the difference in the mean change of SiDBP between the two groups was not significant between the two groups {1.2 mmHg (95% CI: -1.1 to 3.4), p=0.31}. In the PP population (n=137), SiDBP was also significantly reduced at 12 weeks by 11.7 mmHg (95% CI: 10.0 to 13.4) in the LST/HCTZ group and by 12.9 mmHg (95% CI: 11.2 to 14.5) in the amlodipine group (p<0.001 for both groups).
However, the difference in the mean change of SiDBP between the two groups was not significant {1.1 mmHg (95% CI: -1.3 to 3.5), p=0.35}. These results are summarized in Table 2.
In the ITT population, SiSBP was significantly reduced at 12 weeks by 19.7 mmHg (95% CI: 17.0 to 22.4) in the LST/HCTZ group and by 19.2 mmHg (95% CI: 16.5 to 21.9) in the amlodipine group (p<0.001 for both groups). However, the difference in the mean change of SiSBP between the two groups was not significant {-0.5 mmHg (95% CI: -4.3 to 3.4), p=0.82}. In the PP population, SiSBP was also significantly reduced at 12 weeks by 20.4 mmHg (95% CI: 17.6 to 23.2) in the LST/HCTZ group and by 19.9 mmHg (95% CI: 17.1 to 22.6) in the amlodipine group (p<0.001 for both groups). However, the difference in the mean change of SiSBP between the two groups was not significant {-0.5 mmHg (95% CI: -4.5 to 3.4), p=0.79}. These results are summarized in Table 3.
There was no significant difference in the response rates for the LST/HCTZ group (66.7%) and the amlodipine group (75.9%) (p=0.20).
Fig. 3 demonstrates the serial changes in blood pressure. SiDBP during the active treatment period showed no significant difference between the two groups (p=0.17). There were also no significant differences in the SiDBP change between the two groups during any of the three 4-week intervals (p=0.11, 0.17, and 0.42 for the first, second, and third 4-week intervals, respectively).
The serial changes in SiSBP during the active treatment were not significantly different between the two groups (p=0.19). The SiSBP change during the first 4-week interval was greater in the LST/HCTZ group (p=0.04), but was not significantly different during the second or third 4-week intervals (p=0.49 and 0.62 for the second and third 4-week intervals, respectively).
The overall incidence of AEs was similar between the LST/HCTZ group (35.6%) and the amlodipine group (34.5%) (p=0.89). The difference in the incidence of drug-related AEs was insignificant between the LST/HCTZ group (15.6%) and the amlodipine group (11.9%) (p=0.49). The list of AEs considered to be drug-related is summarized in Table 4. Dizziness and headache were the most common AEs in both treatment groups. There were no severe AEs requiring special treatment or hospitalization. Through the three 4-week intervals, there was no significant serial increase in the incidence of AEs. The incidences of AEs were 25.6%, 23.3%, and 27.8% during the first, second, and third 4-week intervals in the LST/HCTZ group, and 21.4%, 23.8%, and 13.1% during the respective 4-week intervals in the amlodipine group. There were no significant changes in pulse rates or laboratory parameters from baseline, except for one case of liver enzyme increase in the LST/HCTZ group.
We have demonstrated that LST 50 mg titrated up to a fixed combination of LST/HCTZ 100/25 mg produced clinically equivalent blood pressure reduction to amlodipine besylate 2.5 mg titrated up to 10 mg in Korean patients with mild to moderate hypertension. Both regimens were comparably well tolerated.
Previous studies comparing LST with amlodipine in Asian populations have reported comparable efficacy of the two drugs in reducing blood pressure.12-17) However, those studies have generally made an assumption that LST 50 mg is equivalent to amlodipine besylate 5 mg, which is based on the clinical data from Western populations.6-9) In the present study, we adopted a relatively conservative strategy for the LST-based regimen, assuming that LST 50 mg is equivalent to amlodipine besylate 2.5 mg rather than 5 mg, that losartan/HCTZ 50/12.5 mg is equivalent to amlodipine besylate 5 mg, and that losartan/HCTZ 100/25 mg is equivalent to amlodipine besylate 10 mg in Korean patients. This strategy is partially supported by the report of Rhew et al., in which LST/HCTZ 50/12.5 mg once daily for 12 weeks did not significantly reduce systolic or diastolic blood pressure in Korean patients with ischemic heart failure.18) Adopting this strategy, the patterns and degrees of change in SiDBP according to serial time points were nearly identical between the two groups, although LST 50 mg was more effective than amlodipine besylate 2.5 mg was in reducing SiSBP. However, it is still uncertain whether Asians, who have been suggested to respond less favorably to angiotensin-converting enzyme inhibitors and more favorably to calcium channel blockers than Westerners respond less favorably to ARBs.
In terms of tolerability, the incidence of amlodipine-related AEs in this study (11.9%) was notably lower than that (30%) in a previous summary of 40 placebo-controlled studies by Osterloh.18) This difference might be attributable to the between-race difference in susceptibility to lower extremity edema, which potentially entails discontinuation of medication.20) The incidence of lower extremity edema in the amlodipine group in this study (1.1%) was markedly lower than that (11 to 24%) seen in previous studies of Westerners.19-22) Indeed, only one patient reported lower extremity edema in the amlodipine group, which was not considered drug-related by the investigator.
Goldberg et al.25) reported a placebo-like tolerability profile of LST in a previous pooled analysis of 2,900 patients treated in double-blinded clinical trials. Fixed combinations of LST/HCTZ 50/12.5 mg and 100/25 mg also demonstrated placebo-like tolerability profiles.26) Wu et al.14) reported better tolerability of LST in an Asian population compared with amlodipine in a Formosan population. In the present study, the LST-based regimen and amlodipine-based regimen showed comparable tolerability in terms of the overall incidence of AEs (35.6% and 34.5%, respectively) and incidence of drug-related AEs (15.6% and 11.9%, respectively). Specifically, when even 25 mg of hydrochlorothiazide was combined with LST in LST/HCTZ 100/25 mg, there was no increase in the incidence of AEs, suggesting the placebo-like tolerability of this regimen in an Asian population. There were no cases of significant uric acid elevation or dyslipidemia aggravation.
In summary, the two regimens, with a relatively higher dose of LST/HCTZ than that required by Westerners, produced equivalent blood pressure reduction and were comparably well tolerated in Korean patients with mild to moderate hypertension.
Figures and Tables
Fig. 1
The treatment schedules for the losartan/hydrochlorothiazide group and the amlodipine group. After a 2-week washout period, eligible patients were randomized to receive losartan 50 mg once daily or amlodipine besylate 2.5 mg once daily. Doses were titrated at 4 weeks and 8 weeks to achieve a diastolic blood pressure of <90 mmHg. WO: washout period, L: losartan, H: hydrochlorothiazide, A: amlodipine besylate.

Fig. 2
The proportion of patients treated with initial, once titrated, and fully titrated doses at 12 weeks in each group (sequentially from the bottom).
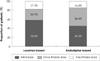
Fig. 3
Antihypertensive effects of the losartan-based regimen and the amlodipine-based regimen at 4, 8, and 12 weeks. The serial changes in sitting systolic and diastolic blood pressure during the active treatment period were no different between the two groups.
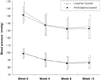
Table 2
Effect of losartan-based regimen and amlodipine-based regimen on sitting diastolic blood pressure at 12 weeks

References
1. Dahlof B, Sever PS, Poulter NR, et al. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet. 2005. 366:895–906.
2. Bangalore S, Kamalakkannan G, Parkar S, Messerli FH. Fixed-dose combinations improve medication compliance: a meta-analysis. Am J Med. 2007. 120:713–719.
3. Waeber B, Burnier M, Brunner HR. Compliance with antihypertensive therapy. Clin Exp Hypertens. 1999. 21:973–985.
4. Ruilope LM, Simpson RL, Toh J, Arcuri KE, Goldberg AI, Sweet CS. Controlled trial of losartan given concomitantly with different doses of hydrochlorothiazide in hypertensive patients. Blood Press. 1996. 5:32–40.
5. Soffer BA, Wright JT Jr, Pratt JH, Wiens B, Goldberg AI, Sweet CS. Effects of losartan on a background of hydrochlorothiazide in patients with hypertension. Hypertension. 1995. 26:112–117.
6. Martina B, Dieterle T, Weinbacher M, Battegay E. Effects of losartan titrated to losartan/hydrochlorothiazide and amlodipine on left ventricular mass in patients with mild-to-moderate hypertension: a double-blind randomized controlled study. Cardiology. 1999. 92:110–114.
7. Wilson TW, Lacourciere Y, Barnes CC. The antihypertensive efficacy of losartan and amlodipine assessed with office and ambulatory blood pressure monitoring. CMAJ. 1998. 159:469–476.
8. Phillips RA, Kloner RA, Grimm RH Jr, Weinberger M. The effects of amlodipine compared to losartan in patients with mild to moderately severe hypertension. J Clin Hypertens (Greenwich). 2003. 5:17–23.
9. Dahlof B, Lindholm LH, Carney S, Pentikainen PJ, Ostergren J. Main results of the losartan versus amlodipine (LOA) study on drug tolerability and psychological general well-being. J Hypertens. 1997. 15:1327–1335.
10. Jamerson K, DeQuattro V. The impact of ethnicity on response to antihypertensive therapy. Am J Med. 1996. 101:22S–32S.
11. Lee HY, Kang HJ, Koo BK, et al. Clinic blood pressure responses to two amlodipine salt formulations, adipate and besylate, in adult Korean patients with mild to moderate hypertension: a multicenter, randomized, double-blind, parallel-group, 8-week comparison. Clin Ther. 2005. 27:728–739.
12. Watanabe S, Okura T, Kurata M, et al. The effect of losartan and amlodipine on serum adiponectin in Japanese adults with essential hypertension. Clin Ther. 2006. 28:1677–1685.
13. Yasuda G, Ando D, Hirawa N, Umemura S, Tochikubo O. Effects of losartan and amlodipine on urinary albumin excretion and ambulatory blood pressure in hypertensive type 2 diabetic patients with overt nephropathy. Diabetes Care. 2005. 28:1862–1868.
14. Wu SC, Liu CP, Chiang HT, Lin SL. Prospective and randomized study of the antihypertensive effect and tolerability of three antihypertensive agents, losartan, amlodipine, and lisinopril, in hypertensive patients. Heart Vessels. 2004. 19:13–18.
15. Iino Y, Hayashi M, Kawamura T, et al. Renoprotective effect of losartan in comparison to amlodipine in patients with chronic kidney disease and hypertension. Hypertens Res. 2004. 27:21–30.
16. Park HC, Xu ZG, Choi S, et al. Effect of losartan and amlodipine on proteinuria and transforming growth factor-beta1 in patients with IgA nephropathy. Nephrol Dial Transplant. 2003. 18:1115–1121.
17. Ishimitsu T, Minami J, Yoshii M, et al. Comparison of the effects of amlodipine and losartan on 24-hour ambulatory blood pressure in hypertensive patients. Clin Exp Hypertens. 2002. 24:41–50.
18. Osterloh I. The safety of amlodipine. Am Heart J. 1989. 118:1114–1119. discussion 1119-20.
19. Volpe M, Junren Z, Maxwell T, et al. Comparison of the blood pressure-lowering effects and tolerability of losartan- and amlodipine-based regimens in patients with isolated systolic hypertension. Clin Ther. 2003. 25:1469–1489.
20. Leonetti G, Magnani B, Pessina AC, Rappelli A, Trimarco B, Zanchetti A. Tolerability of long-term treatment with lercanidipine versus amlodipine and lacidipine in elderly hypertensives. Am J Hypertens. 2002. 15:932–940.
21. Oparil S, Barr E, Elkins M, Liss C, Vrecenak A, Edelman J. Efficacy, tolerability, and effects on quality of life of losartan, alone or with hydrochlorothiazide, versus amlodipine, alone or with hydrochlorothiazide, in patients with essential hypertension. Clin Ther. 1996. 18:608–625.
22. Omvik P, Thaulow E, Herland OB, Eide I, Midha R, Turner RR. Double-blind, parallel, comparative study on quality of life during treatment with amlodipine or enalapril in mild or moderate hypertensive patients: a multicentre study. J Hypertens. 1993. 11:103–113.
23. Hong SJ, Ahn TH, Baek SH, et al. Comparison of efficacy and tolerability of amlodipine orotate versus amlodipine besylate in adult patients with mild to moderate hypertension: a multicenter, randomized, double-blind, placebo-controlled, parallel-group, 8-week follow-up, noninferiority trial. Clin Ther. 2006. 28:537–551.
24. Park S, Chung N, Kwon J, et al. Results of a multicenter, 8-week, parallel-group, randomized, double-blind, double-dummy, phase III clinical trial to evaluate the efficacy and tolerability of amlodipine maleate versus amlodipine besylate in Korean patients with mild to moderate hypertension. Clin Ther. 2005. 27:441–450.
25. Goldberg AI, Dunlay MC, Sweet CS. Safety and tolerability of losartan potassium, an angiotensin II receptor antagonist, compared with hydrochlorothiazide, atenolol, felodipine ER, and angiotensin-converting enzyme inhibitors for the treatment of systemic hypertension. Am J Cardiol. 1995. 75:793–795.
26. Gradman AH, Brady WE, Gazdick LP, Lyle P, Zeldin RK. A multicenter, randomized, double-blind, placebo-controlled, 8-week trial of the efficacy and tolerability of once-daily losartan 100 mg/hydrochlorothiazide 25 mg and losartan 50 mg/hydrochlorothiazide 12.5 mg in the treatment of moderate-to-severe essential hypertension. Clin Ther. 2002. 24:1049–1061.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download