Abstract
Background and Objectives
Percutaneous coronary intervention for chronic total occlusion lesions is technically difficult despite equipment advances. Changes in electrocardiographic patterns, such as Q and T waves, during chronic total occlusion can provide information about procedural success and myocardial viability. In this study, we investigated clinical, electrocardiographic, and procedural characteristics of chronic total occlusions.
Subjects and Methods
Patients (2,635) who underwent coronary angiography between January 2006 and July 2007 at six Catholic University Hospitals were identified using a dedicated Internet database.
Results
A total of 195 patients had total occlusion lesions (7.4%). Percutaneous coronary interventions were attempted in 136 total occlusion lesions (66.0%) in 134 patients. Successful recanalization with stent implantation was accomplished in 89 lesions, with a procedural success rate of 66.4%. One procedure-related death occurred because of no-reflow phenomenon. After excluding 8 patients with bundle branch block, Q and T wave inversions were observed in 60 (32.1%) and 78 patients (41.7%), respectively. The presence of Q waves was associated with severe angina, decreased left ventricular ejection fraction, regional wall motion abnormality, and T wave inversion, but was not related to procedural success.
Conclusion
Percutaneous coronary intervention is a safe and useful procedure for the revascularization of coronary chronic total occlusion lesions. The procedural success rate was not related to the presence of pathologic Q waves, which were associated with severe angina and decreased left ventricular function.
Percutaneous coronary intervention (PCI) of chronic total occlusion (CTO) lesions has a low success rate and is technically difficult regardless of operator experience and despite advances in equipment. CTO treatment remains a major challenge and is a frequent reason for patient referral for coronary artery bypass surgery (CABG), leading some to refer to the treatment as the "last frontier" of PCI.1)2) However, CTOs account for 10% of all PCI,3) with the majority of patients treated with either CABG or medical therapy. The choice of therapy depends on center policies and operator experience. Several studies performed during the bare metal stent (BMS) era showed high rates of restenosis (32-55%) and re-occlusion (8-12%).4)5) Drug-eluting stents are safe and effective in this challenging lesion subset because they markedly reduce the incidence of restenosis and the need for target lesion revascularization.6-9) Several retrospective observational studies have reported the clinical impact of successful percutaneous CTO revascularization on long-term survival.10) Other studies have demonstrated statistically significant improvements in left ventricular function and regional wall motion with successful CTO recanalization.11-13)
Electrocardiogram (ECG) is performed for almost all patients who undergo cardiologic evaluation. In old Q wave myocardial infarctions, persistent negative T wave inversion in infarction-related leads (IRL) is associated with transmural infarction with a thin fibrotic layer,14-16) and normalization of the T wave can identify viable myocardium.17) The absence of a Q wave, which confers the non-existence of a previous myocardial infarction, is a predictor of improved left ventricular systolic function after successful recanalization of the CTO.18)
Here, we analyzed the clinical and angiographic characteristics and trends in revascularization and the treatment of CTOs at the six hospitals in the Catholic Medical Center, Korea, between January, 2006, and July, 2007. We also analyzed Q and T wave patterns, which predict myocardial viability, in CTO patients.
Demographic and procedural data for all patients undergoing coronary angiography at Catholic Medical Center were prospectively entered into a dedicated internet database. All data, including age, gender, medical history, coronary angiographic results, ejection fraction, and treatment recommendations, were prospectively collected at the time of cardiac catheterization. All chronically occluded vessels observed between January 2006, and July 2007, were retrospectively identified. Patients with previous bypass surgery or recent (<3 months) myocardial infarction were excluded.
Significant coronary disease was defined as ≥1 lesion of ≥70% luminal diameter stenosis. Total coronary artery occlusion was defined as 100% luminal diameter stenosis without a discernable lumen and the absence of anterograde flow. CTO was defined as total coronary artery occlusion of ≥1 month in duration. Multivessel disease was defined as ≥70% stenosis in ≥2 vessels.
Before the procedure, all patients were treated with a loading dose of ≥300 mg clopidogrel and 100 mg aspirin. At the start of the procedure, patients received a single bolus of unfractionated heparin (80-120 U/kg body weight). Procedures were performed using a standard femoral approach. In more than 90% of cases, guidewires with microcatheter support were used to cross the lesion, but newer techniques were also attempted, such as intravascular ultrasound (IVUS)-guided manipulation of the guidewire. Procedural success was defined as reduction of residual lumen diameter stenosis to <50% and successful stent employment in the CTO segment without a major adverse cardiac event (MACE). MACE consisted of in-hospital death, myocardial infarction, urgent or emergent CABG, or a cerebrovascular event.
An ECG was performed at the time of admission for coronary intervention. The presence of a Q wave ≥30 msec in leads III and aVF was regarded as the Q wave area in right coronary artery occlusion, while the presence of a Q wave ≥30 msec or R waves ≤20 mV in leads V3 and V4 was defined as the Q wave area in left anterior descending artery occlusion. Q waves longer than 30 msec in two or more leads of V5, V6, and aVL, were defined as the Q wave area in left circumflex artery occlusion. Patients with left or right bundle branch block (QRS duration ≥120 msec) were excluded from ECG analysis. In-hospital and 30-day clinical data were also accessed from the internet registry.
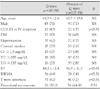
Between January 2006, and July 2007, 2,635 patients underwent coronary angiograms and 195 had at least one CTO (7.4%). Eleven patients had 2 CTO lesions, giving a total of 206 detected CTO lesions. The baseline demographics of the patients are presented in Table 1. About half of the patients had 3-vessel disease, and CTOs were most commonly observed in the right coronary arteries (Table 2).
PCI was not attempted in 61 patients: 58 patients decided to only take medication and 3 patients were referred for CABG. Recanalization using PCI was attempted in 134 patients for 136 CTO lesions. Successful recanalization with stent implantation was accomplished in 89 patients and 89 CTO lesions, giving a procedural success rate of 66.4% (Table 2).
Recanalization was most frequently attempted for CTO of the left anterior descending artery. In most cases, coronary lesion passage was initially attempted with a soft guidewire with microcatheter support. CTO lesion passage was accomplished in 61 cases (success rate: 44.1%). In 3 cases, guidewires with stiffer tips were used initially. In the remaining 72 cases, coronary guidewires with stiffer tips were subsequently used to cross over the CTO lesion, and lesion crossing was accomplished in 28 cases. After adequate balloon dilatation, stent implantation was attempted. Sirolimus-eluting coronary stents (SES) (Cypher™ stent, Cordis Johnson and Johnson, Miami, FL, USA) were the most common stent. One patient died during the procedure due to no-reflow phenomenon (Table 2).
Failure of guidewire crossover through the CTO lesion was the most common reason for unsuccessful procedures (38 CTO lesions: 80.9%). In 8 cases (17%), the stent could not pass the CTO lesion although balloon dilatation was successful. Unacceptable engagement of the guiding catheter was the reason for failure in one CTO lesion (2.1%).
Eight patients were excluded from the ECG analysis because they had bundle branch block. More than 90% of patients had regular sinus rhythm (n=181, 96.8%), and atrial fibrillation was observed in 6 patients (Table 3). The presence of a Q wave was related to more severe anginal symptoms according to the Canadian Cardiovascular Society (CCS) classification system for angina; decreased left ventricular ejection fraction and regional wall motion abnormality were observed by echocardiography (p<0.01), but other clinical and laboratory findings did not differ whether the patients had Q waves or not. The Q wave was not related to the procedural success rate (p=0.55) (Table 4).
Here we measured the clinical, electrocardiographic, and procedural characteristics of CTO lesions in multiple Korean centers. While the technical and procedural success rates of PCI in CTOs have steadily increased over the last 15 years because of greater operator experience and improvements in equipment and procedural techniques,19)20) PCI of CTO lesions still has a low success rate and is technically difficult. In a series of 1,074 consecutive patients undergoing PCI, the primary success rate was 90% in non-occluded lesions, 78% in functional total occlusions {Thrombolysis in Myocardial Infarction (TIMI) flow grade 1}, and 63% in true CTOs.21) Contemporary series found procedural success rates from 55% to 80%, with the variability reflecting differences in operator technique and experience, availability of advanced guidewires, CTO definition, and case selection.2)3)10)
We sampled subjects for a year and a half beginning in Jan, 2006, when the internet-based coronary artery database from Catholic Medical Center became available. Drug-eluting stents (DESs) became commercially available in March, 2003, in Korea. Thus, bare metal stents were not used in this study. The SES (Cypher™ stent, Cordis Johnson and Johnson, Miami, FL, USA) was most common DES, in part because it was available sooner than other DESs. In this study, the operator chose the coronary stent.
The most common cause of the inability to cross the lesion was failure to traverse the lesion with a guidewire, which occurred at a similar percentage as previously reported.22) The success rate for percutaneous CTO recanalization has improved over the last five years due to the introduction of stiffer, more powerful, and more supportive wires with greater torque responses.2) In this study, we observed that a guidewire with a soft tip crossed the CTO lesion in almost 70% of cases when the operator was accustomed to manipulating the guidewire and when the backup power was increased using a microcatheter. The procedural success of CTO was particularly dependent on operator skill and on case selection; therefore, every operator should be accustomed to manipulating the guiding catheter and guidewire and the coronary angiogram should be reviewed carefully to identify anatomical structures, including collateral flows, before the CTO procedure.
Although the procedural success rate was similar to that in previous studies, MACE occurred in only one patient during the procedure, perhaps due to differences in defining MACE. However, this finding also suggests that PCI for CTO is a safe treatment choice when the operator is comfortable with procedure and the case is carefully selected. Many new techniques and devices have improved the success rate of CTOs recanalization.23)24) Although successful PCI for CTO lesions confers a long-term clinical advantage,24) controversies remain whether all CTOs should be recanalized.
Various ECG parameters, such as T wave normalization, help assess myocardial viability or recovery of function.17) We could not examine whether negative T waves were normalized because our study was observational in nature, using a internet-based registry in which follow-up data were not available. The absence of a Q wave predicts improved LV systolic function after successful recanalization of CTO.18) Also, ECG before PCI can predict the functional outcome of intervention for CTO. According to our data, CTO patients with Q waves showed more severe angina symptoms (CCS class III or IV); however, previous studies reported that LV function was less likely to improve in these patients after successful PCI.25) Thus, CTO patients with Q waves cannot be helped by successful PCI for CTOs. However, our study also suggests that improved LV function can be expected in more than half of patients after successful PCI for CTO lesions based on ECG patterns. The procedural success rate was not influenced by ECG patterns.
This study has several limitations. The most important limitation is that this is only an observational study based on data in an internet-based registry. Also, predictors of long-term survival or procedural success cannot be explained in this study. The results of this study were also influenced by differences in selection criteria, operator experience, and technique among the participating centers.
These data represent a multicenter series of consecutive patients with CTO in Korea. A relatively high success rate with a low incidence of complications was observed, indicating that further standardization of procedures, especially of guidewire manipulation, will improve the rate of successful PCI for CTO. PCI for CTO should be seriously considered in selected CTO patients for better clinical outcomes. Furthermore, all operators who perform PCI for CTO should be accustomed to new devices and techniques, such as the TornusTM catheter or the retrograde approach,2)23)24) to improve the success rate of the procedure.
Figures and Tables
References
1. Puma JA, Sketch MH Jr, Tcheng JE, et al. Percutaneous revascularization of chronic coronary occlusions: an overview. J Am Coll Cardiol. 1995. 26:1–11.
2. Nakamura S, Bae JH. Recent progress of the use of interventional therapy for chronic total occlusion. Korean Circ J. 2008. 38:295–300.
3. Hoye A, van Domburg RT, Sonnenschein K, Serruys PW. Percutaneous coronary intervention for chronic total occlusions: the Thoraxcenter experience 1992-2002. Eur Heart J. 2005. 26:2630–2636.
4. Rubartelli P, Niccoli L, Verna E, et al. Stent implantation versus balloon angioplasty in chronic coronary occlusions: results from the GISSOC trial. J Am Coll Cardiol. 1998. 32:90–96.
5. Buller CE, Dzavik V, Carere RG, et al. Primary stenting versus balloon angioplasty in occluded coronary arteries. Circulation. 1999. 100:236–242.
6. Ge L, Iakovou I, Cosgrave J, et al. Immediate and mid-term outcomes of sirolimus-eluting stent implantation for chronic total occlusions. Eur Heart J. 2005. 26:1056–1062.
7. Werner GS, Krack A, Schwarz G, Prochnau D, Betge S, Figulla HR. Prevention of lesion recurrence in chronic total coronary occlusions by paclitaxel-eluting stents. J Am Coll Cardiol. 2004. 44:2301–2306.
8. Lotan C, Almagor Y, Kuiper K, Suttorp MJ, Wijns W. Sirolimuseluting stent in chronic total occlusion. J Interv Cardiol. 2006. 19:307–312.
9. Suttorp MJ, Laarman GJ, Rahel BM, et al. Primary Stenting of Totally Occluded Native Coronary Arteries II (PRISON II): a randomized comparison of bare metal stent implantation with sirolimus-eluting stent implantation for the treatment of total coronary occlusions. Circulation. 2006. 114:921–928.
10. Suero JA, Marso SP, Jones PG, et al. Procedural outcomes and long-term survival among patients undergoing percutaneous coronary intervention of a chronic total occlusion in native coronary arteries: a 20-year experience. J Am Coll Cardiol. 2001. 38:409–414.
11. Dzavik V, Carere RG, Mancini GB, et al. Predictors of improvement in left ventricular function after percutaneous revascularization of occluded coronary arteries. Am Heart J. 2001. 142:301–308.
12. Sirnes PA, Myreng Y, Molstad P, Bonarjee V, Golf S. Improvement in left ventricular ejection fraction and wall motion after successful recanalization of chronic coronary occlusions. Eur Heart J. 1998. 19:273–281.
13. Engelstein E, Terres W, Hofmann D, Hansen L, Hamm CW. Improved global and regional left ventricular function after angioplasty for chronic coronary occlusion. Clin Investig. 1994. 72:442–447.
14. Park YH, Kim JH, Jeong JH, et al. The meaning of pathologic Q wave in myocardial infarction assessed by magnetic resonance imaging. Korean Circ J. 2004. 34:945–952.
15. Kim JY, Park SH, Ko YG, et al. The relationship between Q-wave regression and improvement in the left ventricular systolic function after an anterior wall acute myocardial infarction. Korean Circ J. 2004. 34:356–361.
16. Maeda S, Imai T, Kuboki K, Chida K, Watanabe C, Ohkawa S. Pathologic implications of restored positive T waves and persistent negative T waves after Q wave myocardial infarction. J Am Coll Cardiol. 1996. 28:1514–1518.
17. Altun A, Durmus-Altun G, Birsin A, Gultekin A, Tatli E, Ozbay G. Normalization of negative T waves in the chronic stage of Q wave anterior myocardial infarction as a predictor of myocardial viability. Cardiology. 2005. 103:73–78.
18. Surber R, Schwarz G, Figulla HR, Werner GS. Resting 12-lead electrocardiogram as a reliable predictor of functional recovery after recanalization of chronic total coronary occlusions. Clin Cardiol. 2005. 28:293–297.
19. Kinoshita I, Katoh O, Nariyama J, et al. Coronary angioplasty of chronic total occlusions with bridging collateral vessels: immediate and follow-up outcome from a large single-center experience. J Am Coll Cardiol. 1995. 26:409–415.
20. Berger PB, Bresnahan J. Use of excimer laser in the treatment of chronic total occlusion of a coronary artery that cannot be crossed with a balloon catheter. Cathet Cardiovasc Diagn. 1993. 28:44–46.
21. Safian RD, McCabe CH, Sipperly ME, McKay RG, Baim DS. Initial success and long-term follow-up of percutaneous transluminal coronary angioplasty in chronic total occlusions versus conventional stenoses. Am J Cardiol. 1988. 61:23G–28G.
22. Olivari Z, Rubartelli P, Piscione F, et al. Immediate results and one-year clinical outcome after percutaneous coronary interventions in chronic total occlusions: data from a multicenter, prospective, observational study (TOAST-GISE). J Am Coll Cardiol. 2003. 41:1672–1678.
23. Surmely JF, Tsuchikane E, Katoh O, et al. New concept for CTO recanalization using controlled antegrade and retrograde subintimal tracking: the CART technique. J Invasive Cardiol. 2006. 18:334–338.
24. Kirtane AJ, Stone GW. The Anchor-Tornus technique: a novel approach to "uncrossable" chronic total occlusions. Catheter Cardiovasc Interv. 2007. 70:554–557.
25. Chung CM, Nakamura S, Tanaka K, et al. Effect of recanalization of chronic total occlusions on global and regional left ventricular function in patients with or without previous myocardial infarction. Catheter Cardiovasc Interv. 2003. 60:368–374.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download