Abstract
Background and Objectives
The purpose of this study was to investigate 1) the beneficial effect of bosentan treatment (125 mg twice daily) on exercise capacity and echocardiographic variables and 2) the profiles and frequency of adverse events in Korean patients with World Health Organization (WHO) class III or IV pulmonary artery hypertension (PAH).
Subjects and Methods
Twelve patients who received bosentan treatment were investigated in an open label manner. One patient was excluded in the final analyses due to a prohibited concomitant medication. A 6-minute walk test and echocardiography were performed at baseline and after 12 weeks of treatment.
Results
The administration of bosentan for 12 weeks resulted in a significant improvement in exercise capacity (measured with the 6-minute walking distance), WHO functional capacity, and in echocardiographic variables. Bosentan treatment was associated with a decrease in the maximal tricuspid regurgitation jet velocity {from 4.7 m/sec (95% confidence interval, 3.89-5.45) at baseline to 4.4 m/sec (95% confidence interval, 3.61-5.1) at 12 weeks, p=0.03} and systolic pulmonary arterial pressure {from 105 mmHg (95% confidence interval, 74.4-135.6) at baseline to 93 mmHg (95% confidence interval, 66.3-120.1) at 12 weeks, p=0.04}. Treatment with bosentan at a dose of 125 mg twice a day was not associated with life-threatening side effects, although a higher incidence of elevated liver enzymes compared to previous studies was noted.
Pulmonary artery hypertension (PAH) is a devastating condition that is characterized by a progressive increase in pulmonary vascular resistance, ultimately leading to right heart failure and death.1) To date, the prognosis for patients with PAH is poor due mainly to the limited treatment options. The estimated median survival time is 2.8 years and the estimated 1-, 3-, and 5-year survival rates are 68%, 48%, and 34%, respectively, in patients treated with conventional medications, such as high-dose calcium-channel blockers and prostanoids.2)
Endothelin-1 (ET-1) is a 21-amino-acid, generated from big endothelin by endothelin-converting enzymes in endothelial cells. It is known to have potent effects on vasoconstriction, mitosis, and cell proliferation.3)4) The ET-1 concentrations are increased in the tissues and plasma of patients with PAH due to a reduction in clearance in the pulmonary vascular bed.5) An elevated ET-1 concentration is strongly correlated with disease severity and prognosis in PAH,6) all of which suggest a pathogenic role of ET-1 in PAH. Previous clinical trials using bosentan have clearly demonstrated improvements in pulmonary hemodynamics and exercise tolerance in patients with PAH, supporting its use as a therapeutic strategy for PAH.4-9) European and US treatment guidelines have incorporated bosentan as a treatment option for PAH patients according to World Health Organization (WHO) functional class.10-12)
Bosentan was recently approved for PAH treatment in Korea. However, its beneficial effects on PAH have not been clinically proven in Korean patients. Therefore, the objective of this study was to investigate the effect of bosentan on exercise capacity and pulmonary hemodynamics measured by echocardiography in Korean PAH patients with WHO class III or IV. We also evaluated the profile and the frequency of adverse events related to bosentan treatment.
Patients with PAH over 12 years of age were enrolled into the study if they met the following criteria: 1) symptomatic, severe idiopathic PAH (IPAH), PAH due to collagen vascular disease (e.g., mixed connective tissue disease, systemic lupus erythematosus, or systemic sclerosis), or PAH due to congenital heart disease with previous surgical correction, 2) functional class III or IV according to the 1998 WHO classification, despite maximal conventional medical therapy, and 3) a baseline 6-minute walking distance between 150 and 500 m. In addition to these criteria, the following hemodynamic variables measured at right heart catheterization within 3 months prior to recruitment must also be fulfilled; mean pulmonary arterial pressure (mPAP) >25 mmHg at rest by right heart catheterization, pulmonary capillary wedge pressure (PCWP) <15 mmHg, and pulmonary vascular resistance (PVR) >3 mmHg/L/min. The invasive right heart catheterization was performed at the screening visit only for patients who had no hemodynamic confirmation of PAH within 3 months of enrollment. Due to the teratogenic nature of bosentan, patients who had a possibility of pregnancy were excluded. Patients who had taken phosphodiesterase V inhibitors, such as sildenafil, vardenafil, or tadalafil, within 1 month before enrollment were also excluded. The local ethics committees approved the protocol and written informed consent was obtained from all patients.
Transthoracic echocardiography was also performed at the screening visit, 4 week thereafter (if necessary), and the end of the study or after premature discontinuation from the study. Right heart catheterization and the initial echocardiographic examination were performed within 5-8 days of one another, with a mean interval of 0.5±3.3 days. The right ventricular (RV) end-diastolic and end-systolic areas were carefully measured in the apical 4-chamber view to estimate the RV percentage area change using the following formula:13) RV percentage area change=(RV end-diastolic area-RV endsystolic area)/RV end-diastolic area×100. The RV percentage area change is known to be the best indicator of RV systolic function.13)14) The left ventricular (LV) outflow tract (LVOT) diameter (D; in cm) was measured at the level of the aortic annulus from inner edge to inner edge, utilizing a zoomed image from the parasternal long-axis view, from which the cross-sectional area of the LVOT (CSALVOT) was calculated using the formula: CSALVOT=3.14×(D/2)2. From the apical 5-chamber view, the LVOT time velocity integral (LVOT TVI; in cm) was obtained by positioning the sample volume of the pulsed wave Doppler at the LVOT. The cardiac output (CO) was determined from the pulsed wave measurements of the LVOT velocity profile as follows: CO=CSALVOT×LVOT TVI×heart rate. The cardiac index (CI; in L/min/m2) was calculated by dividing the cardiac output by the body surface area (BSA) of the patient (CI=CO/BSA). The maximal tricuspid regurgitation velocity (TR Vmax; in cm/sec) was obtained from continuous-wave Doppler of the TR signal. The Doppler-derived systolic pulmonary artery pressure (sPAP; in mmHg) was then calculated from the maximal TR Vmax using the simplified Bernoulli formula as follows: sPAP=4×(TR Vmax)2+right atrial pressure (RAP). RAP was estimated by the response of the inferior vena cava to deep inspiration.15)
In the presence of pulmonary regurgitation (PR), the mean pulmonary artery pressure (mPAP) was estimated from the maximal PR velocity (PR Vmax) using the simplified Bernoulli formula as follows: mPAP=4×(PR Vmax)2+RAP.
After obtaining baseline measurements, bosentan administration was launched at a dose of 62.5 mg twice daily for 4 weeks, and 125 mg twice daily for the subsequent 8 weeks. Safety was assessed on the basis of recorded adverse events, clinical laboratory parameters, vital signs, and electrocardiography. The efficacy of bosentan treatment was assessed by changes in the 6-minute walking distance and the WHO functional class after 4 and 8 weeks of treatment, and at the end of study visit or after premature discontinuation from the study.
All values are expressed as the mean±SD or as a number (percentage). Parameters obtained at the 12-week visit were compared to the corresponding baseline values with the Wilcoxon signed-rank sum test. All statistical analyses were performed using Statistical Package for Social Science (SPSS) 13.0 (SPSS Inc., Chicago, IL, USA), and a p<0.05 was considered statistically significant.
Twelve patients were recruited from six centers. One patient was excluded from the efficacy analysis owing to a prohibited concomitant medication (tadalafil). Therefore, the efficacy analyses were completed in 11 patients, whereas safety profiles were analyzed based on all 12 patients.
The baseline characteristics of the 12 patients are shown in Table 1. All patients were in WHO functional class III at baseline. The causes of PAH were idiopathic in nine patients, collagen vascular disease in two patients, and corrected congenital heart disease in one patient. The pulmonary hemodynamic data in these patients are shown in Table 1.
The values of sPAP obtained by Doppler echocardiography were highly correlated with the values obtained at the right heart catheterization (Spearman's r=0.85, p=0.001, n=11) (Fig. 1). The mean difference in sPAP between echocardiography and invasive catheterization measurements was 2.8±18.6 mmHg.
The changes in Doppler echocardiographic values at baseline and during treatment are summarized in Table 2. In comparison with previously published echocardiographic data in normal subjects,16)17) the patients with PAH in the present study had a severely dilated RV. After 12 weeks of bosentan treatment, RV end-systolic and end-diastolic areas tended to decrease, but without reaching statistical significance (p=0.12 and 0.13, respectively). RV systolic function, as evidenced by RV percentage area change, was not modified with bosentan treatment (p>0.99). Whereas sPAP derived from the TR Vmax displayed a significant reduction with bosentan treatment (p=0.04 for sPAP and p=0.03 for TR Vmax), the mPAP estimated from the PR Vmax did not show a significant change (p=0.45 for mPAP and p=0.64 for PR Vmax). The CI trended toward an increase with bosentan therapy (p=0.23).
At the beginning of therapy, all 11 patients were WHO class III. After 4 weeks of therapy, 7 patients improved from class III to class II (p=0.02). At the last follow-up, 6 patients became WHO class II, and 1 patient improved to WHO class I (p=0.02), whereas 4 patients remained WHO class III (Fig. 2).
After 12 weeks of bosentan treatment, the 6-minute walking distance significantly increased from 350.5 m to 412.6 m (p=0.005) (Fig. 3).
There were no deaths in relation to bosentan treatment during the study period. There was also no clinically significant change in systemic blood pressure. Overall, bosentan at a dose of 125 mg twice daily, was well tolerated. Regarding the adverse drug reactions related to bosentan treatment, a moderate headache requiring a transient interruption of bosentan treatment was observed in 1 patient (8.3%), and increases in serum aminotransferase levels were noted in 2 patients (16.7%). In these two patients, the aminotransferase levels returned to the baseline value with a reduction of bosentan dose in one patient, and the other patient showed a marked increment in aminotransferase values to >8 x the upper limit of normal after 6 weeks of bosentan treatment, which normalized after cessation of bosentan.
In Korea, the drugs approved for PAH treatment include iloprost inhalation, oral beraprost, and the oral ET receptor antagonist, bosentan. Of these medications, according to the modified 2007 American College of Chest Physician guidelines, the ET receptor antagonist is recommended as a first-line therapy in patients with WHO functional class III, together with iloprost inhalation.18) Recent studies conducted in Western countries suggest that bosentan also offers a long-term therapeutic strategy for the treatment of PAH. Bosentan monotherapy for patients with idiopathic PAH resulted in estimated 1- and 2-year survival rates of 85% and 70%, respectively.10) Furthermore, the estimated 1- and 2-year survival rates of patients with WHO class III idiopathic PAH, who were actively treated with oral bosentan as a first-line therapy, did not differ from those of an historical cohort of patients initiated on intravenous epoprostenol.19) Of note, ethnic differences have not been reported with respect to the pharmcokinetics of bosentan. In this context, it has been reported that a dose adjustment is not required to treat the Asian PAH population with reference to Caucasians. In one study, a significant improvement in cardiopulmonary hemodynamics, symptoms, and functional capacity over a 12-week treatment with bosentan (125 mg twice daily) wasclearly demonstrated for Japanese patients with severe PAH.20) A recent long-term study (>2.5 years) conducted in Japan also showed that bosentan is associated with sustained clinical improvement.21)
Echocardiography is a well-established diagnostic approach for estimation of sPAP and mPAP. The values of sPAP and mPAP obtained by Doppler echocardiography are known to be highly correlated with values obtained by invasive catheterization.22) This is further supported by the current study, as demonstrated in Fig. 1, with a correlation coefficient of 0.85 despite the lack of simultaneous measurement. Due to the limitation of invasive catheterization in serial evaluation of sPAP and mPAP, we employed tricuspid and pulmonary regurgitation obtained by Doppler echocardiography to serially evaluate sPAP and mPAP during the follow-up period. Given the high concordance between values by Doppler echocardiography and invasive catheterization and the ethical dilemma in the serial performance of invasive catheterization solely for study purposes, our approach for the non-invasive evaluation of pulmonary artery pressure utilized in this study was rational and reasonable.
The current study is the first multicenter study in Korea that was designed to evaluate the beneficial and adverse effects of bosentan treatment for patients with PAH. The administration of bosentan for 12 weeks led to a significant improvement in exercise capacity and WHO classification. The magnitude of improvement in exercise capacity and WHO functional classification was greater than or similar to previous reports.8)23) With respect to echocardiographic variables, with 12 weeks of bosentan therapy, a decrease in TR Vmax and sPAP was noted; however, mPAP that was derived from the PR Vmax was not statistically significant, despite a trend toward a decrease in absolute terms. Although the discrepancy between the change in sPAP and mPAP cannot be clearly explained based on the current study, we suggest that either the small number of patients enrolled in this study or a slight increment in diastolic PAP might be responsible. Future research should include data on diastolic PAP to resolve this question. Apart from mPAP, the RV end-diastolic and end-systolic areas, LVOT TVI, and the CI were not affected by bosentan administration over the 12-week study period. An earlier study also showed a trend toward a decrease in RV end-systolic and end-diastolic areas with oral bosentan treatment without achieving statistical significance,24) which is in agreement with the results of the current study. In spite of a significant decrement in sPAP, bosentan treatment only showed a small increment in the CI. Because pulmonary artery pressure is determined by both pulmonary vascular resistance and pulmonary blood flow, a significant reduction in sPAP accompanied only by a trend toward an increase in the CI should imply that a gradual increase in pulmonary blood flow is preceded by a bosentan-induced decrease in pulmonary vascular resistance. A more lengthy follow-up period may allow for detection of a significant increase in the CI.
Treatment with 125 mg of bosentan twice a day was not associated with any life-threatening adverse events; however, a significant proportion of patients experienced an elevation in aminotransferase levels (16.7%), which is greater than the previous data reporting abnormal hepatic function to be only 4% on the same bosentan dose. Nevertheless, an elevation in aminotransferase levels did not necessitate premature termination of bosentan treatment during the study period in any of the patients enrolled, and the abnormal elevation of liver enzymes gradually improved only with a dosage adjustment of bosentan. Thus, precautionary measures, such as periodic monitoring of aminotransferase levels, should be accompanied by the initiation of bosentan treatment to detect this adverse event.
Korean patients with severe PAH showed a significant improvement in RV hemodynamics, exercise capacity, and functional capacity over 12 weeks of treatment with bosentan (125 mg twice daily). Aminotransferase levels were elevated in 2 cases, but returned to the baseline levels with a reduction of dose or after discontinuation of the medication. Therefore, bosentan, 125 mg twice daily, is considered a clinically optimal dose of treatment and can be employed in clinical practice as a valuable treatment option in Korean patients with PAH. Given the more frequent elevation in liver enzyme levels in comparison with data from Western patients, however, close monitoring of liver function tests during the first few weeks of treatment appears to be mandatory for the early detection of this adverse event.
Figures and Tables
Fig. 1
Correlation between measurement of systolic pulmonary arterial pressure (sPAP) by right heart catheterization and Doppler echocardiography (n=11).
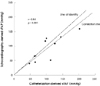
Fig. 2
Changes in World Health Organization (WHO) functional class from baseline to the 12-week follow-up.

Fig. 3
Absolute v alues of 6-minute walking distance from baseline to the 12-week follow-up. P in comparison with baseline value.

Table 2
Effect of bosentan on hemodynamic parameters measured by Doppler-echocardiography from baseline to the 12-week follow-up

*By echocardiography. CI: confidence interval, sPAP: systolic pulmonary arterial pressure, TR Vmax: maximal tricuspid regurgitation velocity, mPAP: mean pulmonary arterial pressure, PR Vmax: maximal pulmonary regurgitation velocity, RV: right ventricle, LVOT: left ventricular outflow tract, TVI: time velocity integral
References
1. Rubin LJ. Primary pulmonary hypertension. N Engl J Med. 1997. 336:111–117.
2. D'Alonzo GE, Barst RJ, Ayres SM, et al. Survival in patients with primary pulmonary hypertension: results from a national prospective registry. Ann Intern Med. 1991. 115:343–349.
3. Yanagisawa M, Kurihara H, Kimura S, et al. A novel potent vasoconstrictor peptide produced by vascular endothelial cells. Nature. 1988. 332:411–415.
4. McLaughlin VV, McGoon MD. Pulmonary arterial hypertension. Circulation. 2006. 114:1417–1431.
5. Giaid A, Yanagisawa M, Langleben D, et al. Expression of endothelin-1 in the lungs of patients with pulmonary hypertension. N Engl J Med. 1993. 328:1732–1739.
6. Rubens C, Ewert R, Halank M, et al. Big endthelin-1 and endothelin-1 plasma levels are correlated with severity of primary pulmonary hypertension. Chest. 2001. 120:1562–1569.
7. Channnick RN, Simonneau G, Sitbon O, et al. Effects of the dual endothelin-receptor antagonist bosentan in patients with pulmonary hypertension: a randomized placebo-controlled study. Lancet. 2001. 358:1119–1123.
8. Rubin LJ, Badesch DB, Barst RJ, et al. Bosentan therapy for pulmonary arterial hypertension. N Engl J Med. 2002. 346:896–903.
9. McLaughlin VV, Sitbon O, Badesch DB, et al. Survival with first-line bosentan in patients with primary pulmonary hypertension. Eur Respir J. 2005. 25:244–249.
10. Galie N, Torbicki A, Barst R, et al. Guidelines on diagnosis and treatment of pulmonary arterial hypertension. Eur Heart J. 2004. 25:2243–2278.
11. Humbert M, Sitbon O, Simonneau G. Treatment of pulmonary arterial hypertension. N Engl J Med. 2004. 351:1425–1436.
12. Galie N, Seeger W, Naeije R, Simonneau G, Rubin LJ. Comparative analysis of clinical trials and evidence-based treatment algorithm in pulmonary arterial hypertension. J Am Coll Cardiol. 2004. 43:12 Suppl S. 81S–88S.
13. Kim HK, Kim YJ, Park JS, et al. Determinants of the severity of functional tricuspid regurgitation. Am J Cardiol. 2006. 98:236–242.
14. Sagie A, Schwammenthal E, Padial LR, Vazquez de Prada JA, Weyman AE, Levine RA. Determinants of functional tricuspid regurgitation in incomplete tricuspid valve closure: Doppler color flow study of 109 patients. J Am Coll Cardiol. 1994. 24:446–453.
15. Kircher BJ, Himelman RB, Schiller NB. Noninvasive estimation of right atrial pressure from the inspiratory collapse of the inferior vena cava. Am J Cardiol. 1990. 66:493–496.
16. Hinderliter AL, Willis PW 4th, Barst RJ, et al. Effect of long-term infusion of prostacyclin (epoprostenol) on echocardiographic measures of right ventricular structure and function in primary pulmonary hypertension. Circulation. 1997. 95:1479–1486.
17. Hinderliter AL, Willis PW 4th, Long W, et al. Frequency and prognostic significance of pericardial effusion in primary pulmonary hypertension. Am J Cardiol. 1999. 84:481–484.
18. Badesch DB, Abman SH, Simonneau G, Rubin LJ, McLaughlin VV. Medical therapy for pulmonary arterial hypertension: updated ACCP evidence-based clinical practice guidelines. Chest. 2007. 131:1917–1928.
19. Sitbon O, McLaughlin VV, Badesch DB, et al. Survival in patients with class III idiopathic pulmonary arterial hypertension treated with first line oral bosentan compared with an historical cohort of patients started on intravenous epoprostenol. Thorax. 2005. 60:1025–1030.
20. Sasayama S, Kunieda T, Tomoike H, et al. Effects of the endothelin receptor antagonist bosentan on hemodynamics, symptoms and functional capacity in Japanese patients with severe pulmonary hypertension. Circ J. 2005. 69:131–137.
21. Sasayama S, Satoh T, Izumi T, Yoshida S, Kyotani S, Tahara N. Long-term trial of bosentan monotherapy for pulmonary arterial hypertension in Japanese patients. Curr Med Res Opin. 2007. 23:395–400.
22. Bossone E, Duong-Wagner TH, Paciocco G, et al. Echocardiographic features of primary pulmonary hypertension. J Am Soc Echocardiogr. 1999. 12:655–662.
23. Channick RN, Simonneau G, Sitbon O, et al. Effects of the dual endothelin-receptor antagonist bosentan in patients with pulmonary hypertension: a randomised placebo-controlled study. Lancet. 2001. 358:1119–1123.
24. Galié N, Hinderliter AL, Torbicki A, et al. Effects of the oral endothelin-receptor antagonist bosentan on echocardiographic and Doppler measures in patients with pulmonary arterial hypertension. J Am Coll Cardiol. 2003. 41:1380–1386.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download