Abstract
Stress-induced cardiomyopathy is characterized by reversible systolic dysfunction of the ventricles, usually involving the apical segments. It occurs more commonly in women and is frequently precipitated by emotional or physical stressors. Ever since the first report of typical stress-induced cardiomyopathy-usually known as Takotsubo cardiomyopathy or transient left ventricular apical ballooning syndrome-was issued, variant forms of stress-induced cardiomyopathy have been reported. We describe a patient who presented with typical ischemic chest pain, but who was found to have an atypical form of stress-induced cardiomyopathy: midventricular ballooning syndrome involving both the left and right ventricles. Transthoracic echocardiography and computed tomography were used in this patient.
Ever since the first description of stress-induced cardiomyopathy was issued in 1991, this disease entity has been predominantly called "Takotsubo cardiomyopathy" or "transient left ventricular (LV) apical ballooning" due to the fact that on left ventriculography it resembles the Japanese fishing pots used to trap octopus.1) It usually presents with symptoms and electrocardiographic findings analogous to those of acute coronary syndrome, in combination with increased cardiac enzymes. Notwithstanding, there is no significant epicardial coronary artery stenosis. Due to its similar manifestations in terms of clinical symptoms, electrocardiographic findings, and elevation in cardiac enzymes, its differentiation from acute myocardial infarction is clinically challenging.
A 53-year-old woman presented to the emergency department with sudden-onset chest pain. Her medical history was unremarkable except for the fact that she had undergone mitral annuloplasty due to severe mitral regurgitation two years prior to the current presentation. Coronary angiography obtained just before mitral annuloplasty showed normal coronary arteries. The patient had no history of angina, hypertension, or diabetes mellitus. The night before presentation, one of her relatives died, and she was under emotional stress. During physical examination, the patient was alert and oriented. Her vital signs were as follows: blood pressure 105/66 mmHg, heart rate 62 beats/min, respiratory rate 20/min, and body temperature 36.3℃. Her electrocardiogram demonstrated a normal sinus rhythm with T wave inversion in V1 and V2 (Fig. 1). Laboratory examination revealed mild elevations in the cardiac enzyme levels: creatine kinase (CK) 711 IU/L, creatine kinase-MB (CK-MB) 30.7 ng/mL, and troponin-I 1.64 ng/mL. Chest X-ray showed cardiomegaly and pulmonary congestion. Transthoracic echocardio graphy performed in the emergency department revealed severe depression in the LV systolic function (LV ejection fraction=35%) and akinetic motion in the mid-segments of both the LV and RV, with hypercontraction in the basal and apical segments (Fig. 2A and B). This abnormal wall motion was more evident on cardiac computed tomographic images (Fig. 2C and D). A trivial degree of mitral and tricuspid regurgitation was noted on transthoracic echocardiography, with an estimated systolic pulmonary arterial pressure of 31 mmHg on the assumption of a right atrial pressure of 10 mmHg {Tricuspid Regurgitation (TR) Vmax=2.31 m/sec}. Coronary computed tomographic angiography was immediately performed to rule out the presence of epicardial coronary artery stenosis, but we could not find any coronary artery stenosis. On the basis of our findings, the diagnosis of stress-induced cardiomyopathy was established. The patient was started on dobutamine and diuretics and successfully stabilized. Four days later, she underwent a follow-up echocardiographic examination, during which substantial improvement in the LV systolic function was noted (LV ejection fraction 49%). One month after the first manifestation, LV systolic function was completely restored; the LV ejection fraction was 56%, and no regional wall motion abnormality was noted (Fig. 3).
Stress-induced cardiomyopathy is known to involve the LV apical segments.4)8) Although many cases of apical ballooning syndrome and a variety of precipitating factors have been described since the initial Japanese report was issued in 1991, atypical manifestations of this unique disease have been recently reported worldwide.4-7)9) Physical and/or emotional stressors preceding clinical presentation suggest the possibility of a complex interplay between the autonomic nervous system (through catecholamines and adrenergic surges) and the heart. However, no definite pathophysiology has been elucidated until now.2)4) Lee et al.2) suggested a unique distribution of hypokinetic or akinetic myocardium with histological evidence of increased adrenergic receptor density at the apex, resulting in increased vulnerability of the LV apex to sudden rises in circulating catecholamines. This theory may account for the classic transient LV apical ballooning syndrome. Atypical forms of stress-induced cardiomyopathy (as in the present case) cannot be adequately interpreted in the context of this theory, although individual variations in terms of relative regional distribution of adrenergic receptors might explain these forms.
Novel variants of stress-induced cardiomyopathy are characterized by involvement of non-apical LV segments that exhibit hypokinesis, akinesis, or dyskinesis on echocardiography.2-7)10) Hahn et al.4) nicely demonstrated the clinical, electrocardiographic, and echocardiographic characteristics in patients with apical and non-apical ballooning syndrome. In accordance with that report,4) our patient was relatively young (53 years old), had no risk factors for coronary artery disease, had a less remarkable T wave inversion on electrocardiogram, and had no significant symptoms of heart failure, despite the presence of overt pulmonary edema on chest X-ray. All these characteristics were indicative of a less severe manifestation. Of note, the most unique feature in our patient was isolated mid-segmental involvement of the RV, as depicted in transthoracic echocardiographic and computed tomographic images. Combined right and left stress-induced cardiomyopathy has been previously described.11)12) Haghi et al.11) reported that RV involvement in the setting of stress-induced cardiomyopathy is associated with a more severe form of LV systolic dysfunction. Another study by Elesber et al.12) demonstrated that patients with RV impairment had lower LV ejection fraction, longer hospitalization, and more cardiac complications-including severe congestive heart failure-as compared to those who had normal RV function. Therefore, physicians should not ignore RV functional assessment in patients with stress-induced cardiomyopathy, given its prognostic implications.
Although invasive coronary angiography was not systematically performed in our patient to exclude the presence of coronary artery disease, such testing was unlikely to alter her diagnosis of stress-induced cardiomyopathy, given the high negative predictive value of noninvasive coronary computed tomographic angiography.13)
In summary, we described a peculiar case of transient midventricular ballooning syndrome involving both the LV and the RV, with hypercontraction in the basal and apical segments. Midventricular ballooning syndrome remains enigmatic, and therefore further studies are needed in order to enhance our understanding regarding this unique disease entity.
Figures and Tables
Fig. 1
Electrocardiogram obtained during the emergency department visit. There is poor R progression in combination with T wave inversion in V1 and V2.
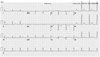
Fig. 2
Initial end-systolic (A) and end-diastolic (B) echocardiographic images obtained in the apical 4-chamber view. Initial end-systolic (C) and end-diastolic (D) computed tomographic images on 4-chamber view. Note isolated akinesia in the mid-portion of both the left and the right ventricles. The mid-portions of both the left and right ventricles exhibit akinesia. Movie files for transthoracic echocardiography and cine computed tomographic images may be requested from the corresponding author.

References
1. Dote K, Sato H, Tateishi H, Uchida T, Ishihara M. Myocardial stunning due to simultaneous multivessel coronary spasms: a review of 5 cases. J Cardiol. 1991. 21:203–214.
2. Lee YP, Poh KK, Lee CH, et al. Diverse clinical spectrum of stress-induced cardiomyopathy. Int J Cardiol. 2008. [Epub ahead of print].
3. Lee HH, Gwon HC, Kim BJ, et al. Clinical manifestation of novel stress-induced cardiomyopathy mimicking acute myocardial infarction: single center prospective registry. Korean Circ J. 2002. 32:1054–1063.
4. Hahn JY, Gwon HC, Park SW, et al. The clinical features of transient left ventricular nonapical ballooning syndrome: comparison with apical ballooning syndrome. Am Heart J. 2007. 154:1166–1173.
5. Hurst RT, Askew JW, Reuss CS, et al. Transient midventricular ballooning syndrome: a new variant. J Am Coll Cardiol. 2006. 48:579–583.
6. Tamura A, Kawano Y, Watanabe T, et al. A report of 2 cases of transient mid-ventricular ballooning. Int J Cardiol. 2007. 122:e10–e12.
7. Yasu T, Tone K, Kubo N, Saito M. Transient mid-ventricular ballooning cardiomyopathy: a new entity of Takotsubo cardiomyopathy. Int J Cardiol. 2006. 110:100–101.
8. Tsuchihashi K, Ueshima K, Uchida T, et al. Transient left ventricular apical ballooning without coronary artery stenosis: a novel heart syndrome mimicking acute myocardial infarction. J Am Coll Cardiol. 2001. 38:11–18.
9. van de Walle SO, Gevaert SA, Gheeraert PJ, De Pauw M, Gillebert TC. Transient stress-induced cardiomyopathy with an "inverted takotsubo" contractile pattern. Mayo Clin Proc. 2006. 81:1499–1502.
10. Shimizu M, Takahashi H, Fukatsu Y, et al. Reversible left ventricular dysfunction manifesting as hyperkinesis of the basal and the apical areas with akinesis of the mid portion: a case report. J Cardiol. 2003. 41:285–290.
11. Haghi D, Athanasiadis A, Papavassiliu T, et al. Right ventricular involvement in takotsubo cardiomyopathy. Eur Heart J. 2006. 27:2433–2439.
12. Elesber AA, Prasad A, Bybee KA, et al. Transient cardiac apical ballooning syndrome: prevalence and clinical implications of right ventricular involvement. J Am Coll Cardiol. 2006. 47:1082–1083.
13. Achenbach S. Computed tomography coronary angiography. J Am Coll Cardiol. 2006. 48:1919–1928.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download