Introduction
It is known that there's a marked variation in the frequency of variant angina attacks according to the circadian rhythm. The attack frequency is usually highest in the early morning and lowest in the afternoon. Patients studied by means of ambulatory electrocardiogram (ECG), and even those without clinically apparent angina pectoris, show more frequent ST segment elevations in the morning.1-4) But whether or not the alterations of the normal sleep and awake cycle will affect the circadian variations of chest pain attacks is uncertain. We describe a middle-aged woman with variant angina whose chest pain occurred only during the daytime.
Case
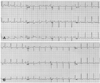
A 48-year-old woman visited the emergency room due to severe resting chest pain. She owned a snack bar for the last ten years and because of her job, she sleeps from noon to 6 pm. For one month she experienced a squeezing heaviness in the mid-chest only during 2 to 3 pm. She had no history of smoking, diabetes or hypertension. She was not yet in menopause. She denied alcohol use and any medications. She weighed 77 kg and had a body-mass index of 30 kg/m2. On arrival, the patient's blood pressure was 128/68 mmHg and the heart rate was 80/min. No precordial murmurs or abnormal sounds were heard, and her lungs were clear. ECG revealed ST-segment elevation in leads II, III, and aVF and reciprocal ST-segment depression in leads I and aVL. She had normal electrolytes and renal function. The hemoglobin was 13.3 g/dL and the platelet count was 250,000/uL. The total cholesterol was 155 mg/dL. The high-density lipoprotein cholesterol level was 48 mg/dL and the triglyceride level was 53 mg/dL. The serum creatinine kinase was 32 U/L with an MB fraction of 0.2 ng/mL; the troponin I level was 0.01 ng/mL. She was treated with intravenous nitroglycerin and the ST-segment elevation was immediately normalized (Fig. 1). Transthoracic echocardiography revealed normal valves, normal atrial and ventricular sizes and functions, and an ejection fraction of 73.5%. She was transferred to our hospital for coronary angiography.
She did not complain of chest pain after transfer to our hospital. The next day coronary angiography was performed. Intravenous nitroglycerin was discontinued four hours before procedure. Right coronary angiography showed diffuse spastic change with subtotal occlusion of the mid right coronary artery, and this was resolved by the administration of intracoronary nitroglycerine (Fig. 2). The left anterior descending artery and left circumflex artery showed no lesions. During the spasm, the patient experienced chest pain with ST-segment elevation in leads II, III and aVF. After relief of spasm, intravascular ultrasound (IVUS) was performed and concentric atherosclerotic plaque was observed at the site of the spasm (Fig. 3). The diagnosis of variant angina was made. She was treated with oral nitrates and calcium-channel blocker.
Discussion
Attacks of variant angina tend to be clustered between midnight and 8 am. However, the fundamental mechanism of circadian variation has not been clearly established. Although autonomic nervous activity and fibrinopeptide A could be related to the circadian variation, further studies are required to confirm this.5)6) Variant angina is considered to occur usually during REM sleep, and some studies have reported that sympathetic activity plays a role in triggering attacks during REM sleep.7) In this case, it was difficult to determine the sleep level because we did not perform electroencephalography or polysomnography.
The sites of spasm in variant angina may be adjacent to atheromatous plaque. In some patients with apparently normal vessels on angiography, the vasospasm occurs at the sites of at least minimal atherosclerotic change, as has been detected by intravascular ultrasonography, like for this case.8) It has been suggested that in this subgroup of patients, the basic abnormality may be hypercontractility of the arterial wall that is associated with the atherosclerotic process itself.9)
This is a rare case of a reversed circadian variation of variant angina. These findings suggest that the alterations of the sleep and wake cycle can affect the circadian variation of variant angina and that taking a good history of the patient's sleep cycle is important for making the correct diagnosis.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download