Abstract
Background and Objectives
Pulmonary arterial hypertension (PAH) is a rare disease with a poor prognosis. The aim of this study was to characterize PAH in pediatric patients by evaluating the patients demographics, clinical and hemodynamic variables, treatments, and outcomes.
Subjects and Methods
Sixty-five patients who were diagnosed with PAH at Seoul National University Children's Hospital between January 1985 and August 2007 were retrospectively reviewed.
Results
There was no difference in gender distribution (males, 33; females, 32). The mean age at the time of diagnosis was 5.7±5.2 years and the mean follow-up period was 6.3±5.5 years. The major causes of PAH were congenital heart disease (CHD) in 32 patients (49.2%) and idiopathic PAH in 11 patients (16.9%). The most common presenting symptom was dyspnea in 44 patients (67.7%). The mean cardiothoracic ratio was 58.9±8.3%, which decreased to 55.9±8.3% after vasodilator therapy (p=0.011). The mean pulmonary arterial pressure at the time of cardiac catheterization was 59.7±18.7 mmHg and the mean pulmonary vascular resistance was 14.9±9.7 wood units · m2. Forty-three of 65 patients (66.2%) had vasodilator therapy (prostacycline, sildenafil, and bosentan). A statistically significant decrease in tricuspid valve regurgitation velocity (4.8±0.8 m/sec vs. 3.6±1.0 m/sec, p=0.001), and an increase in diastolic dimension of the left ventricle (28.3±12.1 mm vs. 33.2±10.2 mm, p=0.021) on echocardiography before and after vasodilator therapy was demonstrated. The 5-, 10-, and 15-year survival rates were 96%, 92% and 65%, respectively. Six of 65 patients (9.2%) with PAH died. There was no significant correlation between outcome and the immediate response to the vasodilators.
Pulmonary arterial hypertension (PAH) is a rare disease of the small pulmonary arteries that is characterized by intimal and medial proliferation and remodeling. It results in a progressive increase in pulmonary arterial resistance, and ultimately right ventricular failure and death.1)2) PAH can be idiopathic, familial, or associated with a number of conditions or disease, such as congenital heart disease (CHD), portal hypertension, connective tissue disease, human immunodeficiency virus (HIV) infection, and exposure to toxins and drugs including appetite suppressants.3)
Information relative to the natural history of PAH has been derived from a national registry conducted in the United States in the early 1980s, in which 187 adult patients were described.4) Although considerable medical advances with respect to PAH have been achieved in the last 2 decades,5) the studies on pediatric PAH are limited.6-10)
Moreover, the characterization of PAH in Korean children has not been determined. The aim of this study was to characterize pediatric PAH by evaluating the demographic, clinical and hemodynamic variables, treatments, and outcomes.
The study population included all patients who met the diagnostic criteria of PAH at Seoul National University Children's Hospital between January 1985 and August 2007. During this period, 178 patients were diagnosed with PAH. A retrospective data analysis of the medical records was conducted with particular attention to the following findings: clinical history, physical examination, laboratory tests, chest radiograph, echocardiography, and cardiac catheterization.
PAH is defined as follows: 1) mean pulmonary arterial pressure (PAP) >25 mmHg at rest or >30 mmHg with exercise and 2) pulmonary capillary wedge pressure ≤15 mmHg at the time of cardiac catheterization.1)7)11-13) If cardiac catheterization was not available, tricuspid valve regurgitation (TR) velocity repeatedly >3.5 m/sec on echocardiography in the cases with no pulmonary stenosis was included.14)15)
We included Eisenmenger syndrome and the patients who showed persistent PAH for >6 months after corrective operation of CHD. We also included infants with PAH subsequent to chronic lung disease and bronchopulmonary dysplasia (BPD) after 3 months of age.
The exclusion criteria were: 1) preoperative PAH and short-term reversible PAH, regressed within 6 months in the case of CHD, 2) PAH associated with BPD, <3 months of age, and 3) persistent pulmonary hypertension of the newborn (PPHN). Among 178 patients, 65 patients consistent with the diagnostic criteria were retrospectively reviewed.
In agreement with the recent clinical classification,3) PAH was classified as idiopathic, familial, or associated with CHD, portal hypertension, or interstitial lung disease (ILD).
Most patients in this study had at least one short-term trial with a vasodilator. Before testing, we attempted to establish a steady state by waiting to obtain baseline hemodynamic values. Then, the hemodynamic response to 100% oxygen breathing was evaluated in most patients. The protocol for vasodilator testing has remained unchanged, but the selected vasodilator drug for short-term challenge has changed over the years (tolazoline and nitric oxide). On the basis of the hemodynamic response to the short-term vasodilator trial, we classified the patients into 2 groups (responders and non-responders). The criteria for a favorable response to vasodilator treatment included the following: 1) a significant decrease in mean PAP or pulmonary vascular resistance index (Rp, >10% from baseline) and 2) a significant increase in oxygen saturation (>10% from baseline).
All statistical analyses were performed with the Statistical Package for Social Science (SPSS) 12.0 for Windows (SPSS Inc., Chicago, IL, USA). Continuous data are presented as the mean with standard deviation when distributed normally and as the median with range otherwise. Discrete data were given as counts or as percentages. Analysis of demographics, and laboratory and hemodynamic characteristics of the patients was performed using the paired t-test and the Wilcoxon signed rank test. For each of the analyses, p<0.05 was considered statistically significant. For survival analysis, we used life table analysis and the Kaplan-Meier method.
The demographic findings are presented in Table 1. There were 65 patients, 33 of whom were males and 32 of whom were females. Ten patients (15.4%) were diagnosed with Down syndrome. The median age was 11.9 years with a range from 6 months to 36 years. The median age at the time of diagnosis was 5.7 years with a range from 3 months to 17 years. We followed up all the survivors with the initial diagnosis and the follow-up period varied from 3 months to 24 years, with a mean of 6.3 years.
The distribution of patients within the various types of PAH is shown in Table 1. About one-fifth of the enrolled patients presented with idiopathic (16.9%) or familial (3.1%) PAH. PAH associated with CHD with a left-to-right shunt was most common, occurring in 32 patients (49.2%). Underlying CHD included the following cardiac malformations: ventricular septal defect (VSD) in 9 patients (28.1%), atrial septal defect in 8 patients (25.0%), complex pulmonary atresia with aortopulmonary collateral arteries in 3 patients (9.4%) and transposition of the great arteries (TGA) in 3 patients (9.4%). Among the patients with PAH and CHD, 16 patients (50.0%) underwent cardiac surgery, 10 patients (31.3%) were diagnosed with Eisenmenger syndrome, and 6 patients (18.8%) did not undergo surgery. ILD with bronchiolitis obliterans organizing pneumonia occurred in 5 patients (55.6%) and BPD was diagnosed in 4 patients (44.4%). Left heart disease, comprised of coarctation of aorta, mitral valve stenosis, or dilated cardiomyopathy (DCMP) existed in 3 (42.9%), 3 (42.9%), and 1 (14.3%) patients, respectively. Other associations with PAH consisted of sleep apnea (n=2), portal hypertension (n=1), and pulmonary veno-occlusive disease (n=1). The age of the PAH group associated with ILD was significantly younger than the other subgroups (p<0.05).
Fifty-eight of 65 patients developed symptoms, 14 of who had ≥2 symptoms. At the time of diagnosis, dyspnea was the most frequent symptom {43 patients (74.1%)}, followed by cyanosis {15 patients (25.9%)}, hemoptysis {4 patients (6.9%)}, peripheral edema {4 patients (6.9%)}, syncope {3 patients (5.2%)}, chest pain {3 patients (5.2%)}, fatigue {2 patients (3.4%)} and palpitations {2 patients (3.4%)}. Eight of 65 patients (12.3%) complained of no symptoms.
The chest radiograph showed the typical changes associated with pulmonary hypertension. The mean cardiothoracic (CT) ratio was 58.9±8.3%; the majority of the patients (89.1%) had a CT ratio >50%. After vasodilator therapy, the mean CT ratio decreased to 55.9±8.3% (p=0.011). Before and after vasodilator therapy, the hemoglobin, hematocrit, prothrombin time international normalized ratio (PT INR), and aspartate aminotransferase (AST), alanine aminotransferase (ALT), and total bilirubin levels did not change significantly (data not shown).
Hemodynamic profiles were measured at the time when the patients underwent diagnostic tests, including cardiac catheterization or echocardiography. The data are summarized in Table 2. Cardiac catheterization was available in 36 patients (55.4%) at the time of diagnosis. The remaining patients were diagnosed by echocardiography. The mean PAP ranged from 32 to 92 mmHg, with a median of 60.0 mmHg. The systolic PAP ranged from 36 to 136 mmHg, with a median of 85.8 mmHg. The median right atrial pressure was 6.6 mmHg (range, 1-10 mmHg). The median right ventricular systolic pressure was 91.8 mmHg (range, 40.5-135 mmHg). The median pressure ratio of the left to right ventricle was 1.3. The mean Rp was 15.0 wood units · m2. On echocardiography, the mean peak TR velocity was 4.3 m/sec and the median pressure gradient was 75.6 mmHg, ranging from 49 to 144 mmHg. The mean peak pulmonary valve regurgitation velocity was 3.3 m/sec.
The data on the hemodynamic response to the short-term administration of vasodilators was available for 21 of the patients. Nine of the 21 patients did not respond to vasodilator therapy. In these patients, neither the mean PAP nor the Rp decreased by administration of the drug (non-responder, p>0.05). In other patients, the mean PAP and Rp decreased after the vasodilator test (responder, p<0.05). The result of the vasodilator test is presented in Fig. 1. We found no significant correlation between gender and the immediate response to the vasodilator.
Anticoagulation therapy was administered to 13 patients (20.0%). Digoxin, furosemide, and spironolactone were given to 21, 14, and 9 patients, respectively. Twenty-two of the 65 patients (35.4%) had no vasodilator treatment. Among them, 14 patients had no medications.
Forty-three patients were treated with vasodilator therapy. The vasodilators were usually initiated with oral prostacyclin analogues (PGI, 48.8%) which were recently switched to sildenafil and/or bosentan in 14 cases. Cough and wheezing were reported in 1 patient treated with PGI for 60 months, who then discontinued the PGI and had no vasodilator therapy.
Eighteen patients (41.9%) were treated with sildenafil, a phosphodiesterase-5 inhibitor. Sildenafil was administered for an average of 15.8 months. Eight of 19 patients (CHD, 4 patients; ILD, 4 patients) discontinued sildenafil because of an improvement in symptoms. One of 18 patients continued sildenafil and 5 patients were treated with sildenafil in combination with bosentan. Rash was reported in one patient, who discontinued sildenafil. In this group, 4 patients died.
Four patients (9.3%) were treated with bosentan, a non-specific endothelin antagonist. Two patients discontinued bosentan therapy because of hepatic side effects in one patient and lack of response in one patient.
Two patients (4.7%) underwent vasodilator combination therapy. One patient was treated with a combination of PGI and sildenafil, and the other was treated with sildenafil and bosentan.
We performed echocardiography and cardiac catheterization during the follow-up period. There was a statistically significant decrease in TR velocity (4.8±0.8 m/sec before therapy vs. 3.6±1.0 m/sec after therapy, p=0.001) and an increase in the diastolic dimension of the left ventricle on echocardiography (28.3±12.1 mm before therapy vs. 33.2±10.2 mm after therapy, p=0.021). We found no statistically significant differences in hemodynamic findings based on cardiac catheterization.
By August 2007, 54 of the 65 patients (83.1%) survived and 6 (9.2%) had died. Five patients (7.7%) were lost to follow-up. The clinical outcomes for each subgroup of PAH patients are presented in Table 3. The most common cause of death was left ventricular failure in 2 patients. Table 4 shows detailed data of the expired patients. We found no significant correlation between outcome and the immediate response to the vasodilator.
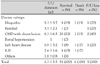
The 5-, 10-, and 15-year survival rates were 96%, 92%, and 65%, respectively (Fig. 2).
Pulmonary arterial hypertension has previously been shown to have a very poor prognosis in children.16) In the 1960s, in a series of 35 patients with idiopathic (primary) PAH,17) 22 patients died within 1 year of the onset of symptoms and none of the patients survived longer than 7 years. Similarly, in 1995 the median survival of 18 children with primary PAH was approximately 4 years.9) Recent advances in understanding the pathophysiology of hypertensive pulmonary circulations have led to a broader pharmacologic arsenal and improved prognosis of children with PAH.
The frequency of PAH in children as well as in adults is not well-known. The estimate of the incidence of idiopathic PAH (IPAH) ranges from one to two new cases per million people in the general population.18) The gender ratio of adult women to men with IPAH has been reported to be 1.7 : 1.4) In children, variability in gender incidence has been reported. Some studies have suggested an equal frequency in children before adolescence, with a 1.5 : 1 male to female frequency in adolescence. Other studies have suggested a 1.5 : 1 female to male ratio at all ages of diagnosis.11)12) In our study, the male to female frequency was the same.
Historically, IPAH exhibits a course of relentless deterioration and early death.19) Unfortunately, the data pertaining to children is less complete than the data pertaining to adult patients. Familial PAH (FPAH) accounts for 6% to 12% of all cases of IPAH.4)8) In our experience, 2 of 13 patients with IPAH were diagnosed with FPAH (15.4%). A variety of CHD can cause PAH. Patients with cyanotic congenital cardiac lesions, such as complex pulmonary atresia with aortopulmonary collateral arteries, TGA, tricuspid atresia, and double outlet right ventricle may also develop PAH.16) VSD was the most frequent underlying defect among all patients with PAH and CHD (28.1%). As in another study,20) patients with CHD and Down syndrome suffered from persistent PAH; in addition, most of them were non-responders.
The presenting symptoms in children with PAH are highly variable and may differ when compared with adult patients. As in adults with IPAH,4)8)21) dyspnea is the most common symptom at diagnosis in children with the disease. Our results were in general agreement with previous reports.12) Peripheral edema, as a reflection of right ventricular failure, is less frequent in children (10%) than in adults (20%) with IPAH. In our study, peripheral edema was present in 4 patients (6.9%). Chest pain or angina is an uncommon symptom in children.
The chest radiograph in patients with PAH may show cardiac enlargement with a prominent main pulmonary artery segment. There might be decreased vasculature in the peripheral lung fields due to a paucity of pulmonary blood flow. In the present study, the mean CT ratio decreased after vasodilator therapy (p=0.011).
Echocardiography is the most valuable non-invasive test for the detection of PAH. A high correlation has been reported between cardiac catheterization and Doppler measurement of systolic pulmonary pressure.14)15) TR of measurable quality has been reported in as many as 86% of cardiovascular patients.22) Although non-invasive tests are useful in the evaluation of suspected PAH, cardiac catheterization remains the gold standard for diagnosis.
The use of pulmonary vasodilator therapy is based on the treatment of IPAH.23) The main concept is that patients with PAH have a restricted pulmonary circulation.1) Increased oxygen demand may worsen pulmonary hypertension and right heart failure. There are currently three major drug classes available for the long-term treatment of PAH. As a potent vasodilator, prostacyclin has been shown to improve hemodynamic function, exercise tolerance, and the quality of life.5) Phosphodiesterase-5 inhibitors, such as sildenafil, have an acute pulmonary vasodilator effect. Sildenafil causes an increase in cyclic guanosine monophosphate (cGMP) levels, which have a role in causing pulmonary vasodilation. Many reports have documented the benefit of sildenafil therapy in children with various clinical conditions, such as IPAH, PAH with CHD, and PAH with lung disease.24)25) Bosentan, an orally active agent dual blocking both the endothelin-A and -B receptors, has been shown to improve pulmonary functional capacity and hemodynamics. Several studies have shown that bosentan is effective in lowering pulmonary artery pressure and PVR, and improving exercise tolerance in adults and in children.26)27) The most frequently reported adverse events associated with bosentan are flushing, headaches, and increased liver aminotransferase levels.27) We have experienced only one patient with elevated liver enzymes.
The median survival among patients diagnosed with PAH in the USA between 1981 and 1985 was 2.8 years. The first large prospective study8) showed an actuarial survival rate of 68% to 77%, 40% to 56%, and 22% to 38% at 1, 3, and 5 years, respectively. Although the 5-year survival rate was 96%, there were some limitations in our study. During the follow-up period, only 6 patients had died, suggesting that survival improved under the therapies presently in use, as compared to data published 17 years ago.8) In one study of infants with BPD who underwent cardiac surgery for the repair of CHD, 25% of those with PAH died.28) The detailed data of the expired patients are presented in Table 4.
A major limitation of our study was that it is a retrospective analysis of data collected from one hospital. As a consequence, due to a lack data, some of our results represent imprecise estimates. PAH is commonly defined by measurements obtained during cardiac catheterization.14)29) However, data from cardiac catheterization is seldom available in this registry. The criterion of PAH, detected by echocardiography, is not clearly defined; PAH is suggested when an echocardiography-derived estimate of systolic PAP exceeds 40 mmHg at rest.30)
This is the first study that has investigated the characterization of PAH in Korean children. In the future, the confirmation of this clinical entity requires analysis of detailed registries throughout the country.
Figures and Tables
Fig. 1
Comparison of mean pulmonary arterial pressure (PAP) and pulmonary vascular resistance (Rp) change during the vasodilator test. After the vasodilator test, (A) the mean PAP and (B) Rp decreased significantly (p<0.05).

Fig. 2
Kaplan-Meier survival curve in patients with pulmonary arterial hypertension. The 5-, 10-, and 15-year survival rates were 96%, 92%, and 65%, respectively.
Table 1
Clinical data at diagnosis for each subgroup of patients with pulmonary arterial hypertension

Acknowledgments
A preliminary version of this work was presented at the 51st Annual Scientific Meeting of The Korean Society of Circulation, 11-13 October 2007.
References
1. Runo JR, Loyd JE. Primary pulmonary hypertension. Lancet. 2003. 361:1533–1544.
2. Farber HW, Loscalzo J. Pulmonary arterial hypertension. N Engl J Med. 2004. 351:1655–1665.
3. Simonneau G, Galie N, Rubin LJ, et al. Clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2004. 43:12 Suppl S. 5S–12S.
4. Rich S, Dantzker DR, Ayres SM, et al. Primary pulmonary hypertension: a national prospective study. Ann Intern Med. 1987. 107:216–223.
5. Humbert M, Sitbon O, Simonneau G. Treatment of pulmonary arterial hypertension. N Engl J Med. 2004. 351:1425–1436.
6. Humbert M, Sitbon O, Chaouat A, et al. Pulmonary arterial hypertension in France: results from a national registry. Am J Respir Crit Care Med. 2006. 173:1023–1030.
7. Jung JW. Pulmonary arterial hypertension of congenital heart disease: from reversible pulmonary hypertension to Eisenmenger syndrome. Korean Circ J. 2007. 37:287–297.
8. Dalonzo GE, Barst RJ, Ayres SM, et al. Survival in patients with primary pulmonary hypertension: results from a national prospective registry. Ann Intern Med. 1991. 115:343–349.
9. Sandoval J, Bauerle O, Gomez A, et al. Primary pulmonary hypertension in children: clinical characterization and survival. J Am Coll Cardiol. 1995. 25:466–474.
10. Duffels MG, Engelfriet PM, Berger RM, et al. Pulmonary arterial hypertension in congenital heart disease: an epidemiologic perspective from a Dutch registry. Int J Cardiol. 2007. 120:198–204.
11. Widlitz AC, Barst RJ. Pulmonary arterial hypertension in children. Eur Respir J. 2003. 21:155–176.
12. Rosenzweig EB, Widlitz AC, Barst RJ. Pulmonary arterial hypertension in children. Pediatr Pulmonol. 2004. 38:2–22.
13. Chin KM, Rubin LJ. Pulmonary arterial hypertension. J Am Coll Cardiol. 2008. 51:1527–1538.
14. McQuillan BM, Picard MH, Leavitt M, Weyman AE. Clinical correlates and reference intervals for pulmonary artery systolic pressure among echocardiographically normal subjects. Circulation. 2001. 104:2797–2802.
15. Bossone E, Bodini BD, Mazza A, Allegra L. Pulmonary arterial hypertension: the key role of echocardiography. Chest. 2005. 127:1836–1843.
16. Rashid A, Ivy D. Pulmonary hypertension in children. Curr Paediatr. 2006. 16:237–247.
17. Thilenius OG, Nadas AS, Jockin H. Primary pulmonary vascular obstruction in children. Pediatrics. 1965. 36:75–87.
18. Rubin LJ. Primary pulmonary hypertension. N Engl J Med. 1997. 336:111–117.
19. Lee WD, Kim DS, Lee JH, et al. A clinical review of primary pulmonary hypertension. Korean Circ J. 2003. 33:507–512.
20. Suzuki K, Yamaki S, Mimori S, et al. Pulmonary vascular disease in Down's syndrome with complete atrioventricular septal defect. Am J Cardiol. 2000. 86:434–437.
21. Lee WS, Kim KH, Jeong DH, et al. Clinical characteristics and prognostic factors of patients with severe pulmonary hypertension. Korean Circ J. 2007. 37:265–270.
22. Borgeson DD, Seward JB, Miller FA Jr, Oh JK, Tajik AJ. Frequency of Doppler measurable pulmonary artery pressures. J Am Soc Echocardiogr. 1996. 9:832–837.
23. Barst RJ, Maislin G, Fishman AP. Vasodilator therapy for primary pulmonary hypertension in children. Circulation. 1999. 99:1197–1208.
24. Humpl T, Reyes JT, Holtby H, Stephens D, Adatia I. Beneficial effect of oral sildenafil therapy on childhood pulmonary arterial hypertension: twelve-month clinical trial of a single-drug, open-label, pilot study. Circulation. 2005. 111:3274–3280.
25. Karatza AA, Bush A, Magee AG. Safety and efficacy of sildenafil therapy in children with pulmonary hypertension. Int J Cardiol. 2005. 100:267–273.
26. Rubin LJ, Badesch DB, Barst RJ, et al. Bosentan therapy for pulmonary arterial hypertension. N Engl J Med. 2002. 346:896–903.
27. Barst RJ, Ivy D, Dingemanse J, et al. Pharmacokinetics, safety, and efficacy of bosentan in pediatric patients with pulmonary arterial hypertension. Clin Pharmacol Ther. 2003. 73:372–382.
28. McMahon CJ, Penny DJ, Nelson DP, et al. Preterm infants with congenital heart disease and bronchopulmonary dysplasia: postoperative course and outcome after cardiac surgery. Pediatrics. 2005. 116:423–430.
29. Barst RJ, McGoon M, Torbicki A, et al. Diagnosis and differential assessment of pulmonary arterial hypertension. J Am Coll Cardiol. 2004. 43:12 Suppl S. 40S–47S.
30. Rubin LJ, Badesch DB. Evaluation and management of the patient with pulmonary arterial hypertension. Ann Intern Med. 2005. 143:282–292.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download