Introduction
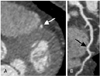
Myocardial bridging (MB) is defined as a segment of a major epicardial coronary artery that proceeds intramurally through the myocardium beneath the muscle bridge (Fig. 1A and B). It is generally confined to the midportion of the left anterior descending coronary artery (LAD). The incidence of MB varies substantially between angiographic series (0.5-4.5%) in the general population1-4) and autopsy specimens (15-85%).1)2)5) Although MB is clinically silent in most cases, it has been associated with myocardial ischemia, myocardial infarction, arrhythmia, and sudden death.1)2)6-9) A diagnosis of MB is made possible via the tunneled segment and its systolic compression as seen on conventional coronary angiography (CCA)(Fig. 1C and D) and as detected by intravascular ultrasound (IVUS) and intracoronary Doppler ultrasound (ICD). CCA is the gold standard for detection, but it is invasive and may not be sensitive enough to detect a thin bridge.1)2) Recently, rapid technical developments in multidetector CT (MDCT) have made possible the clear detection of the entire running courses of coronary arteries and the MB itself. MDCT is accepted as a reliable and sensitive tool for the diagnosis of MB and the evaluation of associated intracoronary hemodynamics.10-21) The purpose of this article is to briefly review the literature and to analyze information concerning the prevalence, anatomic features, pathophysiologic mechanisms, clinical manifestations, and therapeutic options associated with MB. We also review the classical appearance on various imaging modalities, with a particular emphasis on MDCT coronary angiography using 64-slice MDCT and dualsource CT.
Prevalence and Morphology
The real prevalence of MB is still unknown, ranging from 0.5% to 4.9% in angiographic series and from 15% to 85% in autopsies. This is not just because most patients with MB have unrelated overt symptoms and are rarely referred for CCA, but also because thin bridges cause little compression on CCA. CCA with provocation testing enhances systolic myocardial compression, and hence the rate of MB rises to 40%. Furthermore, atherosclerotic plaques located in the segment proximal to the tunneled segment cause underdiagnosis on CCA.1)2) A high prevalence of MB has been reported in patients with hypertrophic cardiomyopathy2)22) and in heart transplant recipients.1)23)
Since MDCT has been widely used for the noninvasive evaluation of coronary artery disease (CAD),24)25) radiologists have encountered MB more frequently than previously reported.
The incidence of MB reported in MDCT coronary angiographic series has ranged from 3.5% to 30.5% in patients with chest pain or with suspected or known CAD.15)17)19) MB is generally confined to the mid-portion of the LAD, even though it may be located in any coronary artery. Ferreira et al.5) defined two types of bridging: 1) superficial bridges (75% of cases) crossing the LAD transversely towards the apex of the heart at an acute angle or perpendicularly, and 2) deep bridges (25% of cases) arising from the right ventricular apical trabeculae that cross the LAD transversely, obliquely, or helically before terminating in the interventricular septum.
The "Protective" Role of Myocardial Bridging
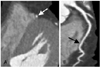
Atherosclerotic plaques are often located in the segment proximal to the bridged segment, although the tunneled segment is typically spared (Fig. 2). This "protective" role of MB has been further confirmed by recent studies using MDCT. This phenomenon can be explained by pathologic studies, which found that the intima beneath the tunneled segment always consisted solely of contractile-type smooth muscle cells. The intima lacked synthetic-type smooth muscle cells, which produce collagen fibrils and elastic fibers in the intima as atherosclerosis progresses. In addition, low wall shear stress proximal to the tunneled segment promotes atherosclerotic plaque formation. However, the high wall shear stress seen in the tunneled segment is thought to exert a protective effect against atherosclerosis.1)2)
Mechanism of Ischemia and Clinical Significance
Since 85% of coronary blood flow normally occurs in diastole, systolic compression of the tunneled segment alone cannot sufficiently explain ischemia and associated symptoms. Myocardial ischemia and its associated symptoms are related to the length and depth of the tunneled segment, the degree of systolic dysfunction, stress- and exercise-induced sympathetic drive, increased local shear force, and local coronary endothelial dysfunction.1)2) Although MB is clinically silent in most cases, it has been associated with angina, myocardial ischemia, myocardial infarction, left ventricular dysfunction, myocardial stunning, paroxysmal atrioventricular (AV) blockade, exercise-induced ventricular tachycardia, and sudden cardiac death.1)2)6-9) MB is frequent in patients with hypertrophic cardiomyopathy, representing a potential increased risk of sudden death in young patients (Fig. 3). MB must be considered in symptomatic young patients at low risk for coronary atherosclerosis.1) Occasionally, MB has caused technical problems during coronary bypass surgery (Fig. 4).26)
Imaging Findings on Conventional Coronary Angiography, Intracoronary Ultrasound, and Intracoronary Doppler Ultrasound
The typical angiographic findings of the "milking effect" and the "step down-step up" phenomena are induced by systolic compression of the tunneled segment (Fig. 1C and D). CCA is likely to underestimate the prevalence of MB by delivering a visualization that is limited to the vessel lumen, thus necessitating that investigators rely on indirect signs. Even though demonstration of systolic compression and the milking effect are considered diagnostic, these signs are rather insensitive in the superficial type of MB that demonstrates minimal systolic compression or none at all. Similarly, the step down-step up phenomenon may be absent in superficial MB. CCA has gradually relinquished its position as the gold standard for diagnosing MB because deeply located tunneled segments usually appear to be sufficiently compressed during systolic phase, and atherosclerotic stenosis proximal to the MB may hamper identification of the tunneled segment.1)2) IVUS demonstrates the "half-moon phenomenon" in the tunneled segment. ICD with pullback of the Doppler wire reveals a characteristic flow pattern: the "fingertip phenomenon" or the "spike-and-dome pattern". IVUS is a sensitive method for assessing wall thickness and vessel size prior to stenting the MB to avoid coronary perforation. Even though CCA, IVUS, and ICD can reveal the morphological and functional features of MB, these procedures are invasive.1)2)27)
Imaging Findings on Multidetector CT Coronary Angiography
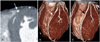
The recent advent of MDCT scanners using 16, 40, and 64 slices has enabled clear and reliable visualization of the coronary arteries.10-21) The latest 64-slice MDCT scanners render 64 slices per rotation and offer a maximum temporal resolution of 165 ms and an unprecedented spatial resolution of isotropic 0.4 mm3. Multiplanar reformatted images assessed by MDCT provide information about the lumen and walls of the coronary arteries and the myocardium in any plane. Therefore, MB can be demonstrated on MDCT coronary angiography, regardless of the thicknesses and directions of muscle bundles in the MB. Furthermore, MDCT coronary angiography is effective in the evaluation of concomitant atherosclerotic coronary lesions. According to recent studies, MDCT coronary angiography is a reliable noninvasive imaging modality for the diagnosis of MB that allows for evaluation of the real incidence and anatomical characteristics of MB in vivo. The differences in the prevalence (3.5-30.5%) of MB using MDCT can be explained by the better temporal and spatial resolution obtained using the latest 64-slice MDCT scanners, by differences in postprocessing techniques used to delineate MB, and by inclusion or exclusion of superficial MB.20) The location of MB varies in MDCT coronary angiographic series even though MBs are principally confined to the mid-segment of the LAD (Fig. 5).13)15)17) Konen et al.15) defined three useful anatomical patterns of MB in the LAD according to the depth and course of the tunneled segment on CT: the "superficial" type (Fig. 6), seen in 29% of all intramuscular LAD segments, in which the tunneled segment had a superficial course along the interventricular septum and was covered by a thin layer of tissue (<1 mm thick); the "deep" type (Fig. 7), seen in 41% of all tunneled LAD segments, in which the tunneled segment penetrated the interventricular septum at a depth between 1 and 6.2 mm; and the "right ventricular" type (Fig. 8), seen in 29% of all tunneled LAD segments, in which the tunneled segment crossed through the right ventricular anterior wall adjacent to the interventricular septum.
In general, MB may be a coincidental finding, but MB has been implicated as a causative factor in symptomatic patients. The deep tunneled segment could compromise coronary diastolic flow and result in ischemia, compared with the superficial tunneled segment.1)2)5)27) It is known that the degree of tunneled artery obstruction is dependent on such factors as location, thickness, length of the muscle bridges, and degree of cardiac contractility. Leschka et al.18) demonstrated that the degree of systolic MB compression on CCA was significantly correlated with tunneled segment depth, but not length. However, they did not investigate the relationship between MB and clinical symptoms.
Measurement of the systolic compression of the tunneled segment with 64-slice MDCT may be inaccurate because the limited temporal resolution of CT scanners does not allow for reliable coronary anatomical delineation during the end-systolic phase. Dual-source CT, with 2 arrays consisting of an X-ray tube and detectors arranged at 90 degrees to each other, and with a gantry rotation time of 330 ms, allows for a temporal resolution of 83 ms at the center of the rotation when half-scan image reconstruction algorithms are used. The high temporal resolution enables visualization of the vessel lumen during most of the cardiac cycle. Hence, the milking effect can be observed in the 4D reconstruction (Fig. 9).21)
Treatment
Asymptomatic MB warrants no treatment. Symptomatic MB may be treated medically or surgically. Medical treatment as a first-line therapy includes nitrates, beta-blockers, and calcium antagonists. In patients with severe angina and clinically relevant ischemia, surgical treatments such as myotomy and coronary artery bypass grafting are considered.1)2) Coronary stent implantation may be the treatment of choice for patients whose conditions are complicated by infarction or recalcitrance.1)2)29)30)
Conclusion
MB is a common anatomical variant characterized by myocardial encasement of a coronary artery segment. Even though this variant is considered a benign condition, early diagnosis and treatment are important due to the complications associated with MB. Diagnosis of MB is made possible with the tunneled segment and the systolic compression seen on various imaging modalities. MDCT coronary angiography is accepted as a reliable non-invasive method for the diagnosis of MB because MDCT directly depicts the length and depth of the tunneled segment, along with its degree of compression during systole.




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download