Abstract
Background and Objectives
Subjects and Methods
Results
Conclusion
Figures and Tables
 | Fig. 1Venn Diagram illustrating the population qualifying for pharmacotherapy according to NCEP-ATP III or SHAPE guideline. Data are expressed as number (% of total participants). *Individuals qualifying for pharmacotherapy according to NCEP-ATP III guideline, †According to SHAPE guideline, ‡Individuals not qualifying for pharmacotherapy according to neither guidelines, §Significant stenosis was defined as more than 50% luminal narrowing on MDCT. NCEP-ATP: National Cholesterol Education Program- Adult Treatment Panel, SHAPE: Screening for Heart Attack Prevention and Education. |
 | Fig. 2Risk stratification for coronary heart disease across the severity of subclinical coronary atherosclerosis detected by MDCT. Individuals were categorized into each risk groups according to NCEP-ATP III guideline (A), and SHAPE guideline (B). *Significant stenosis was defined as more than 50% luminal narrowing on MDCT. MDCT: multi-detector computed tomography, NCEP-ATP: National Chole-Sterol Education Program-Adult Treatment Panel, SHAPE: Screening for Heart Attack Prevention and Education. |
 | Fig. 3Receiver operating characteristics curves for the presence of the plaque with significant stenosis. Significant stenosis was defined as more than 50% luminal narrowing on MDCT. NCEP-ATP III: NCEP-ATP III risk stratification (AUC, 0.64; 95% confidence interval, 0.59-0.68). SHAPE: SHAPE risk stratification (AUC, 0.84; 95% confidence interval, 0.78-0.88). AUC: area under the curve, MDCT: multi-detector computed tomography, NCEP-ATP: National Cholesterol Education Program-Adult Treat-Ment Panel, SHAPE: Screening for Heart Attack Prevention and Education. |
 | Fig. 4Proportion of individuals qualifying for pharmacotherapy according to NCEP-ATP III or SHAPE guideline across the severity of subclinical coronary atherosclerosis detected by MDCT. *Significant stenosis was defined as more than 50% luminal narrowing on MDCT, †p was calculated for McNemar test, ‡Numbers are percentage of individuals qualifying for pharmacotherapy according to each guideline. MDCT: multi-detector computed tomography, NCEP-ATP: National Cholesterol Education Program-Adult Treatment Panel, SHAPE: Screening for Heart Attack Prevention and Education. |
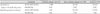
Table 1

Data are expressed as number (%) and mean±SD. BMI: body mass index, WC: waist circumference, SBP: systolic blood pressure, DBP: diastolic blood pressure, F/Hx: family history, CHD: coronary heart disease, FBS: fasting blood sugar, LDL-C: low density lipoprotein-cholesterol, HDL-C: high density lipoprotein-cholesterol, BUN: blood urea nitrogen, CRP: C-reactive protein, CACS: coronary artery calcium score
Table 2

Data are expressed as number of individuals (% of total participants). Individuals classified as very high risk (CACS>400) were combined with those categorized as high risk (CACS 100-399) in SHAPE risk stratification. *Individuals were classified as low-risk (0-1 risk factor), moderate-risk (≥2 risk factors but <10% risk of CHD at 10 years), moderately high-risk (≥2 risk factors and 10% to 20% risk of CHD in 10 years), or high-risk (≥2 risk factors and >20% risk of CHD in 10 years). SHAPE: Screening for Heart Attack Prevention and Education, NCEP-ATP: National Cholesterol Education Program-Adult Treatment Panel, CACS: coronary artery calcium score, CHD: coronary heart disease
Table 3

Data are expressed as number of individuals (% of individuals categorized into the same risk group). Individuals classified as very high risk (CACS>400) were combined with those categorized as high risk (CACS 100-399) in SHAPE risk stratification. SHAPE: Screening for Heart Attack Prevention and Education, NCEP-ATP: National Cholesterol Education Program-Adult Treatment Panel, CACS: coronary artery calcium score, N/A: not applicable
Table 4
Data are expressed as number (%). *Occlusive plaque was defined as more than 50% luminal narrowing on maximum intensity projection images or multi-planar reconstruction images. CAD: coronary arterial disease, NCEP-ATP: National Cholesterol Education Program-Adult Treatment Panel, SHAPE: Screening for Heart Attack Prevention and Education




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download