Abstract
Femoral arterial closure devices are now commonly used after both diagnostic and therapeutic coronary procedures. They have been shown to reduce the time to ambulation and to decrease the length of the hospital stay. Angioseal is a commercially available femoral artery closure device that has been approved by the Food and Drug Administration (FDA). The device sandwiches an intra-arterial absorbable anchor on the luminal side of the vessel and a thrombin plug on the surface of the vessel with using a self-cinching stitch. We report here on three patients who presented with acute and delayed arterial occlusive complications that were found to be due to an Angioseal anchor that was not appropriately reabsorbed.
Arterial closure devices are increasingly being used after percutaneous endovascular procedures. They shorten the time to hemostasis and the duration of bed rest, and they may also decrease the length of the hospital stay and increase the patients' comfort.1) Angioseal® (St. Jude Medical) is a commercially available femoral artery closure device that has been approved by the Food and Drug Administration (FDA). Angioseal consists of a polymer mixture anchor placed on the inner side of the artery and it is connected, through an absorbable suture, to a bovine collagen plug, which compresses the artery externally.
The two parts are pressed against each other, squeezing the vascular puncture site like a sandwich.2) At our medical center, the frequency of using Angioseal is 75 cases per year and the incidence of Angioseal-related vascular complication that require surgical repair is about 4%. We report here on three cases of Angioseal-induced arterial occlusions in patients who presented with pain, numbness and claudication that was found to be caused by an Angioseal anchor that did not resorb appropriately.
A 74-year-old male suffering with acute myocardial infarction had been catheterized 40 days ago into a right femoral artery for emergency coronary intervention. The patient then presented with right leg intermittent claudication and a tingling sensation 40 days after a percutaneous cororonary intervention and puncture site closure with using a 6 Fr Angioseal. The patient had no history of symptomatic peripheral vascular disease.
The physical examination was remarkable for the reduced popliteal and pedal pulses. All the left lower limb pulses were normal. Lower extremities Doppler studies showed evidence of reduced arterial blood flow, with a lesion at the iliac and common femoral artery levels. An abdominal aortogram revealed normal common, external and internal iliac arteries bilaterally. A completely occluded lesion was present in the right common femoral artery at the level of the femoral head, which was the previous puncture site (Fig. 1A). Using access via the right common femoral artery, we attempted balloon dilatation of the lesion using a 7×40 mm balloon (Ultrathin, Boston Scientific). Following balloon deflation, severe residual stenosis was angiographically observed in the common femoral artery. The occluded vascular lumen was not fully expanded and stenosed due to dense fibrotic thrombus remained, so reduced blood flow in the distal superficial femoral artery was present.
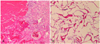
Elective surgery for removal of the residual foreign body was performed. The occluded proximal femoral artery was resected and graftinterposed with an 8 mm expanded polytetrafluoroethylene (ePTFE) vascular graft. The gross features (Fig. 2) and microscopic findings (Fig. 3) demonstrated that the anchor of the Angioseal had not been absorbed, and it had induced foreign body reaction with fibrosis and this eventually obstructed the vascular lumen.
The patient had an uncomplicated postoperative recovery and was discharged on postoperative day 7. One month later, the patient was well with no recurrent symptoms.
An elective coronary intervention and right femoral catheterization were performed to a 72-year-old diabetic female with unstable angina. The patient complained of right lower leg pain, numbness and poikilothermia one hour after a percutaneous endovascular procedure and closure of the femoral artery puncture site with using a 6 Fr Angioseal. The patient had no history of symptomatic peripheral vascular disease. The physical examination revealed the aggravated tendency of rubor and pallor with remarkably reduced popliteal and dorsalis pedal pulses of the right leg. Doppler sonography of the right lower extremities showed reduced arterial blood flow with a lesion at the right superficial femoral artery from the puncture site level. We conducted CT angiography of the lower extremities to confirm the exact obstructed level. There was a completely diffuse occluded lesion in the right superficial femoral artery from the puncture site to the mid- to distal portion of the right superficial femoral artery (Fig. 1B), but the popliteal and trifurcation levels were intact. The patient developed rapidly progressive numbness, rubor change and leg pain. Emergency surgical thrombectomy and a graft operation were performed. The occluded superficial femoral artery was resected and graft-interposed with an 8 mm ePTFE vascular graft. The gross and microscopic findings demonstrated that the Angioseal had not been absorbed, and there was thrombotic debris with a foreign body reaction. The patient had an uncomplicated postoperative recovery and she was discharged on postoperative day 7. One month later, there were no definite complications on the follow-up physical examination.
Elective coronary intervention and right femoral catheterization were performed for evaluation of unstable angina to a 72-year-old female. The patient presented with right leg coldness and paresthesia immediately after a percutaneous coronary intervention and the puncture site had been closed with a 6 Fr Angioseal. The patient had no history of symptomatic peripheral vascular disease. The physical examination was remarkable for the reduced popliteal and dorsalis pedal pulses of the lower right leg. After confirming decreased blood flow on Doppler sonography, we planned emergency CT angiography of the lower extremities. The CT angiography showed complete thrombotic occlusion of the right popliteal artery (Fig. 1C), while the other arterial lumen was intact. After three hours of intravenous heparinization, we were able to palpate the pulse in the right dorsalis pedal artery. After one month of management with warfarin and aspirin combination therapy at the outpatient department, there were no significant complications.
The Angioseal® device is composed of a collagen sponge and an absorbable polymer anchor that attaches to the hole in the arteriotomy site.3) The Angioseal anchor softens and is reabsorbed with complete dissolution in approximately 30 days, as determined by microscopy, and in nearly 90 days, as determined by chemical analysis.4) A large multicenter trial reported the incidence of Angioseal-related groin complications that required surgical repair to be 0.5%.5) In a meta-analysis by Koreny et al., the device-related vascular complications were classified into major (pseudoaneurysm, AV fistula, common femoral artery thrombosis, retroperitoneal hematoma, infection, bleeding from the puncture site that required transfusion, and death) and minor (localized allergic reaction, hematoma not requiring transfusion and continuous oozing at the puncture site).6) The rate of major complications ranged from 0% to 15.8%, while that of the minor complications ranged from 0% to 23%.7) However, many complications may not have become apparent in the strictly controlled pre-marketing investigational trials. In any case, manual compression, although uncomfortable for the patient and it is fatiguing and timeconsuming for the staff, is cheap, and this is still associated with a very low complication rate.3)
To the best of our knowledge, acute or delayed vascular occlusive complications after Angioseal deployment have very rarely been reported in Korea. The patients in our cases presented with vascular thrombosis associated with the plug of an Angioseal device. The patients commonly had pain, pallor, poikilothermia, paresthesia and disabling claudication with weak popliteal and pedal arterial pulsation. Physical examinations of the pulses and auscultation of the femoral area should be performed prior to catheterization and immediately after the insertion of closure devices. Diagnostic tool-ultrasound imaging demonstrated non-significant occlusive stenosis that was not immediately detected on the physical examination after the procedure. On the gross and microscopic findings of the surgically removed debris, the patients of our prior two cases were found to have a significant amount of focal intimal hyperplasia and thrombosis in the proximal femoral artery. Endarterectomy and patch angioplasty successfully cleared the obstruction and this relieved the symptoms of the patients. Improper deployment of the Angioseal device may result in complete occlusion of the femoral artery at the site of arterial puncture, and the anchor may subsequently destroy/break loose a large posterior wall of atherosclerotic plaque and so occlude the lumen.7)
Most Angioseal complications manifest early. In one study, half of the adverse events were recognized soon after the initial procedure and half presented from two to nine days later.8) In our first case, the patient did not become symptomatic until six weeks after the procedure. We presume that a progressive obstructive process that was due to slow propagation of a thrombus was likely delayed due to the post-stent use of antiplatelet agents. Our three cases illustrate that vascular complications can have acute or delayed clinical presentations, and physicians who use arterial closure devices must be alert for possible complications. Thrombogenic occlusion, reactive stenosis and embolism are possible device-specific complications, and they should be directly managed with anticoagulation and thrombolytic agents.9) However, if the complications are not resolved, then physicians must not delay interventional and surgical treatment because dissolution of the material and the apposition of thrombotic material increases the mass of the occluding material and so makes complete extraction more difficult.
Figures and Tables
Fig. 1
Images of the obstructive lesions at the distal portion of the femoral artery puncture site. The abdominal aortogram showed a completely occluded lesion in the right common femoral artery at the level of the femoral head, at the site of a previous puncture (A). CT angiography demonstrated completely diffuse occluded lesion in the right superficial femoral artery from a puncture site (B). Complete thrombotic occlusion (arrow) of the right popliteal artery was observed by CT angiography (C).

Fig. 2
Surgical findings of the occluded lesion. A large obstructive lesion (1.5×1.0 cm sized) was visible in the proximal superficial femoral artery (A). This mass-like lesion was attached to the intima and it was easily detached from the vessel wall by forceps. The mass was nodular, hard and yellowish in color and showed red colored pigmentation from blood and brownish coloration from the thrombus (B).

References
1. Seok JH, Park YH, Kim MK, et al. Efficacy and complications of Angio-Seal® device in patients undergoing coronary angiography and angioplasty. Korean Circ J. 2003. 33:574–582.
2. Mukhopadhyay K, Puckett MA, Roobottom CA. Efficacy and complications of Angioseal in antegrade puncture. Eur J Radiol. 2005. 56:409–412.
3. Ferreira AC, Eton D, de Marchena E. Late clinical presentation of femoral artery occlusion after deployment of the angio-seal closure device. J Invasive Cardiol. 2002. 14:689–691.
4. Applegate RJ, Rankin KM, Little WC, Kahl FR, Kutcher MA. Restick following initial Angioseal use. Catheter Cardiovasc Interv. 2003. 58:181–184.
5. Ward SR, Casale P, Raymond R, Kussmaul WG 3rd, Simpfendorfer C. Efficacy and safety of a hemostatic puncture closure device with early ambulation after coronary angiography. Am J Cardiol. 1998. 81:569–572.
6. Koreny M, Riedmüller E, Nikfardjam M, Siostrzonek P, Müllner M. Arterial puncture closing devices compared with standard manual compression after cardiac catheterization: systematic review and meta-analysis. JAMA. 2004. 291:350–357.
7. Gonze MD, Sternbergh WC 3rd, Salartash K, Money SR. Complications associated with percutaneous closure devices. Am J Surg. 1999. 178:209–211.
8. Gwechenberger M, Katzenschlager R, Heinz G, Gottsauner-Wolf M, Probst P. Use of a collagen plug versus manual compression for sealing arterial puncture site after cardiac catheterization. Angiology. 1997. 48:121–126.
9. Goyen M, Manz S, Kröger K, Massalha K, Haude M, Rudofsky G. Interventional therapy of vascular complications caused by the hemostatic puncture closure device angio-seal. Catheter Cardiovasc Interv. 2000. 49:142–147.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download