Abstract
The amlodipine/atorvastatin single tablet has been shown to improve patients' achievement of national guideline recommended blood pressure and lipid target levels and exhibits a safety profile consistent with the parent compounds. The single tablet formulation has the potential to improve adherence and decrease prescription costs. These potential benefits are associated with important implications because hypertensive patients with additional risk factors represent a large proportion of those at risk for cardiovascular events. Combination low-dose drug treatment increases efficacy and reduces adverse effects. Fixed low-dose combination drug treatment increases efficacy and reduces adverse effects. This combination has greater potency and a similar side effect profile to monotherapy and represents a highly effective approach for attaining goal blood pressure levels using a therapeutic strategy that very effectively lowers blood pressure, is well-tolerated, and minimizes increasing doses of monotherapy-induced metabolic effects.
Hypertension is the leading risk factor for cardiovascular disease (CVD) mortality, which accounts for approximately 30% of all deaths worldwide. According to an analysis based on the Framingham data, 78% of hypertensive males and 82% of hypertensive females have at least one other cardiovascular (CV) risk factor.1) The Health Survey for England reported in 1998 that 19% of males and 26% of females with hypertension also had high total cholesterol levels.2)
Patients with hypertension are also more likely to have associated CV risk factors; for example, approximately 50% of patients with hypertension have hypercholesterolaemia and 20-40% of patients with hypertension have hyperglycaemia. The presence of multiple risk factors increases the risk of CV events associated with hypertension. The most common risk factors for CVD include advanced age (> 55 years for males and >65 years for females), smoking, dyslipidaemia, family history of premature CVD, abdominal obesity, abnormal C-reactive protein levels, and clinical conditions, such as diabetes and renal disease.3)
For the appropriate control and improving compliance in hypertensive patients, fixed-dose combination therapy for better blood pressure (BP) and risk control are currently recommended.
Recent evidence suggests that large-scale reductions in cardiovascular events are observed when hypertension and dyslipidemia are treated. For example, it has been calculated that almost one-half of the coronary heart disease events occurring in hypertensive patients could be prevented by controlling BP and lipid levels. However, several different medications with varying frequencies of dosing are important contributory factors to poor compliance, particularly in elderly patients. Therefore, efforts should be made to simplify drug regimens to reduce the frequency of drug administration, as well as the number of tablets to be taken. This can be achieved using long-acting agents and fixed-dose combinations. For example, a single tablet, such as an amlodipine/atorvastatin compound to treat hypertension and dyslipidemia, can be taken by everyone at increased risk for CVD or stroke.
Blood pressure and low density lipoprotein-cholesterol (LDL-C)-lowering are key therapeutic strategies for preventing cardiovascular events in hypertensive patients with additional risk factors. However, this approach is confounded by poor patient adherence to antihypertensive and lipid-lowering medications. Pill count is an important issue for hypertensive patients that are less likely to refill their antihypertensive and lipid-lowering prescriptions as their total number of prescriptions increases.4) Synchronizing the initiation of antihypertensive and lipid-lowering therapy also improves adherence in comparison to patients starting one therapy more than 30 days prior to the other,5) and adherence decreases as the time between initiation of antihypertensive and lipid-lowering therapies is prolonged. Patient adherence to medication has also been shown to be significantly greater with a single-pill regimen compared to a two-pill regimen for antihypertensive therapy alone.6) Recently, the increased cost of multiple prescriptions has been reported to have a large impact on adherence.7) Physicians may therefore be able to significantly improve medication adherence by initiating antihypertensive and lipid-lowering therapy concomitantly, thereby reducing pill burden and costs.
Amlodipine/atorvastatin (Caduet®) is a once-daily fixed-dose combination of the dihydropyridine calcium channel antagonist, amlodipine, and the HMG-CoA reductase inhibitor, atorvastatin. It is indicated for the management of hypertension and dyslipidemia in patients in whom treatment with both agents is appropriate.
In clinical trials, the fixed-dose combination of amlodipine/atorvastatin effectively manages two important risk factors simultaneously in hypertensive patients at risk of CVD or in those patients with concomitant hypertension and dyslipidemia. The combination is bioequivalent to amlodipine and atorvastatin given alone, and does not modify the efficacy of either single agent. Amlodipine/atorvastatin is generally well-tolerated, with a tolerability profile consistent with that of each single agent. Compared with the co-administration of each single agent, the convenience of single-tablet amlodipine/atorvastatin has the potential to improve patient adherence and the management of cardiovascular risk in selected patients, thereby improving clinical outcomes.
Amlodipine is a dihydropyridine calcium channel blocker (CCB) that inhibits extracellular calcium influx into vascular smooth muscle via blockade of L-type calcium channels, causing relaxation of vascular smooth muscle and leading to a reduction in BP. Atorvastatin is a HMG-CoA reductase inhibitor that impedes mevalonic acid formation, which subsequently reduces cholesterol formation and increases the rate of LDL-C clearance from plasma.8) Atorvastatin (40 mg/day) increases flow mediated dilation (FMD) and decreases the carotid-radial pulse wave velocity (PWV) at 8 weeks of administration in patients with moderate hypercholesterolemia (total cholesterol: 200-250 mg/dL). The combined administration of amlodipine and atorvastatin may have an additive or potentially synergistic beneficial effect on atherosclerotic plaque formation and some molecular markers of endothelial function (Table 1).
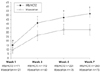
Administration of the fixed-dose combined amlodipine/atorvastatin tablet does not alter the rate or extent of absorption of either agent. The pharmacokinetic and pharmacodynamic properties of amlodipine and atorvastatin make them well-suited for combination in a single tablet to manage CV risk.9) The half-lives of both agents facilitate once-daily dosing, and both can be administered at any time of the day with or without food.10) Randomized, controlled trials, such as Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT), Valsartan Antihypertensive Long-term Use Evaluation (VALUE), Comparison of Amlodipine versus Enalapril to Limit Occurrences of Thrombosis (CAMELOT), and Anglo-Scandinavian cardiac outcomes trial-blood pressure lowering arm (ASCOT-BPLA), have demonstrated that amlodipine reduces CV events and deaths in patients with hypertension and reduces CV events in normotensive patients with coronary artery disease (CAD). Statins have been unequivocally established as first-line pharmacotherapy for the majority of patients with dyslipidemia.11) Moreover, atorvastatin has demonstrated clinical efficacy in inhibiting atherosclerosis and preventing cardiovascular events in randomized, controlled trials in patients with diabetes. The co-administration of amlodipine and atorvastatin has been demonstrated to be safe and effective for lowering both BP and LDL-C in patients with concomitant hypertension and dyslipidemia (Fig. 1).12) The fixed-dose combination of amlodipine/atorvastatin is generally well-tolerated in patients with hypertension with or without dyslipidemia, with an overall tolerability profile similar to each single agent. In clinical trials, the most common treatment-related adverse events associated with amlodipine and atorvastatin administered as a fixed-dose combination or concomitantly as separate agents were peripheral edema, myalgia, and sinusitis. Most adverse events were mild-to-moderate in severity. Neither drug has any adverse effects on the other's efficacy or tolerability (Fig. 2).13)
Amlodipine/atorvastatin is the first single-tablet therapy available for the treatment of more than one CV risk factor. Single-tablet amlodipine/atorvastatin may provide an important strategy to help narrow the existing practice-outcome gap for CV risk reduction.
It is difficult to achieve adequate BP control with monotherapy in most patients, even when the dose is optimised.14) Response rates with any class of antihypertensive administered as monotherapy range from 30-60%; however, no monotherapy has been shown to achieve target BP in more than 20-30% of the overall hypertensive population (Fig. 3).15)
By contrast, combining two complementary antihypertensive agents has been shown to improve the response rate to 75-90%. Compared with high-dose monotherapy, combination therapy is associated with fewer adverse effects. Guidelines advocate combination therapy with once daily treatment regimens that provide 24-h efficacy.16) Firstline combination treatment is recommended in Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC)-717) for patients with a BP >20 mmHg above the systolic goal or 10 mmHg above the diastolic goal. Hypertension guidelines from the International Society on Hypertension in Blacks (ISHIB)18) suggest the use of combination therapy when BP is >15 mmHg above the systolic goal and/or >10 mmHg above the diastolic goal.
Fixed-dose combination antihypertensive drugs have been available for the treatment of hypertension for over 40 years. Reserpine/dihydralazine/hydrochlorothiazide (Unipres®) and methyldopa/hydrochlorothiazide (Aldoril®) were marketed in the 1960s. Fixed-dose combination antihypertensive drugs subsequently lost popularity because of a perception of increased toxicity compared to monotherapy. However, a large variety of fixed-dose combination agents have been developed in recent years for patients requiring multiple antihypertensive agents for BP control (Table 2).19)
The advantages of combination therapy include improved adherence to therapy20) and minimization of BP variability. In addition, combining two antihypertensive agents with different mechanisms of action may provide greater protection against major CV events and the development of end-organ damage.16) The challenge remains to translate the evidence and recommendations outlined in the current hypertension management guidelines into clinical practice, as combination therapy remains underused, especially in high-risk patients. Table 4 shows the expected reduction in blood pressure with one, two, and three BP-lowering drugs used at one-half standard doses.21) The reductions with two and three drugs are based on the additive effect.
The dose-response relationship is clear for thiazides, β-blockers, and calcium channel blockers. Thiazides and CCB infrequently cause symptoms (2.0 and 1.6%, respectively) at one-half the standard doses, but commonly (9.9 and 8.3%, respectively) at standard doses (p<0.001). β-blockers cause symptoms in 5.5% of patients at one-half standard doses and in 7.5% at standard doses (p=0.04). Cough (3.9%) was virtually the only symptom with angiotensin converting enzyme (ACE) inhibitors and did not vary with dose, a finding consistent with earlier studies.12)13) No excess symptoms occurred at standard doses or one-half standard doses with angiotensin II receptor blockers (ARB) (Table 5).21)
In 66 trial arms, single drugs caused symptoms in 5.2% (3.6-6.6%) of participants on average (prevalence in the treated group minus prevalence in the placebotreated group). In 33 trial arms, 2 drugs together caused symptoms in 7.5% (5.8-9.3%), which is significantly lower than the value of 10.4% (5.2%×2) expected with an additive effect (p<0.03). One drug does not therefore potentiate the adverse effects of another. Many antihypertensive agents work by affecting fluid and sodium balance, blocking the renin-angiotensin-aldosterone system (RAAS), or the sympathetic nervous system, and decreasing systemic vascular resistance by blocking L-type calcium channels. Combinations of ACE inhibitors, ARB, diuretics, and CCB have additive effects in controlling BP and minimizing adverse effects of individual components. Combination therapy using ARB with hydrochlorothiazide (HCTZ) provides greater potency and fewer side effects than higherdose monotherapy with either agent, and potentially offers benefits beyond those of BP-lowering alone, particularly in high-risk hypertensives. The combination of an ARB and HCTZ has been reported to be effective in difficult-to-treat and severely hypertensive patients for several ARB, including losartan, candesartan, telmisartan, and eprosartan. A high fixed-dose combination of irbesartan (300 mg)/HCTZ (25 mg) given once daily was also effective and well-tolerated in patients with previously uncontrolled hypertension. As well as significantly reducing BP measured in the clinic in anambulatory setting, 12 weeks of treatment preserved the circadian profile, as shown by trough-to-peak ratios and smoothness index values for systolic and diastolic BP (Fig. 4).22) No metabolic changes were observed at these doses, and no patients discontinued the study because of treatment-related side effects. Fixed-dose combinations of HCTZ and ARBs provide effective, simple, aggressive, and well-tolerated BP control and are now rapidly gaining acceptance with physicians. The usefulness of ARB/HCTZ combinations in hypertension has now been demonstrated in clinical trials for most of the ARBs.23) Some of the most detailed recent data have been obtained with valsartan. In a recent double-blind, multicenter study of 24 weeks duration involving 1,088 patients, fixed-dose combinations of valsartan (160 mg) with HCTZ (15.5 or 25 mg) were found to reduce BP to a similar degree to amlodipine alone (10 mg).24) However, adverse events were significantly less frequent with the ARB/HCTZ combination and discontinuation rates as a result of adverse events were 4.2%, 3.5%, and 18.2% in the valsartan/HCTZ (12.5 mg), valsartan/HCTZ (25 mg), and amlodipine groups, respectively (Fig. 5).24)
Calcium channel blockers effectively and safely lower BP and reduce long-term CV risk in a wide range of patient populations. As CCBs have a different mode of action to commonly used inhibitors of the RAAS pathway (such as ACE inhibitors and ARB), combinations with these agents should provide synergistic or complementary effects compared with using two agents that inhibit the same pathway.25)
The Avoiding Cardiovascular events through COMbination therapy in Patients Living with Systolic Hypertension (ACCOMPLISH) study is the first outcomes trial to compare initial therapy with two different combinations. Patients will be randomized to amlodipine/benazepril (5/20 mg) or benazepril/HCTZ (20/12.5 mg), and will have their doses force-titrated to standard maintenance doses of amlodipine/benazepril (5/40 mg) and benazepril/HCTZ (40/12.5) mg during the first 2 months. The doses can be increased to 10/40 mg or 40/25 mg, respectively, and after 3 months, other antihypertensive agents (excluding the drug classes involved in the primary treatments) can be added to achieve a BP <140/90 mmHg (<130/80 mmHg for patients with diabetes or renal insufficiency). Investigators will be strongly encouraged to reach target blood pressure in all patients.
Patients will be seen at 3 and 6 months, and thereafter at 6-month intervals until the end of the trial (mean, 39 months). The amlodipine/benazepril-treated group showed 20% less CV mortality/morbidity compared with the benazepril/HCTZ-treated group. The ACCOMPLISH trial will provide compelling evidence for initial combination therapy with angiotensin converting enzyme inhibitor (ACEI)/calcium channel blocker (CCB) and challenge current diuretic-based guidelines.
Global risk reduction is very important for prevention of CV event in patients with hypertension. Single-tablet amlodipine/atorvastatin (Caduet®) is the first single-tablet therapy available for the treatment of more than one CV risk factor, and increases compliance, decreases multiple CV risk factors, and decreases morbidity and mortality with CAD. Caduet may provide an important strategy to help reduce the existing practiceoutcome gap for CV risk reduction.
Fixed low-dose combination therapy of antihypertensive agents whose mechanisms of action are complementary is an effective, safe, and cost-effective method of decreasing BP in most patients with essential hypertension. Because many neurohormonal and cellular mechanisms cause hypertension, defining a specific etiology and creating a cause-specific treatment plan is difficult. Reduction in BP is only about 20% less at one-half standard dose than at standard dose, but adverse effects are much less common.
The efficacy of drugs in combination is additive, but the prevalence of adverse effects is less than additive. Fixed-low dose combinations of two or three drugs at low dose are therefore preferable to one or two drugs at standard dose to improve compliance and reduce cost, consequently to help improve CV outcome.
Figures and Tables
 | Fig. 1Efficacy of amlodipine/atorvastatin compared with single-agent therapy or placebo in patients with concomitant hypertension and dyslipidemia. *p=.225 versus atorvastatin; p<.001 versus amlodlpine, †p<.001 versus atorvastatin; p=.520 versus amlodipine, ‡p<.001 versus atorvastatin; p<.001 versus amlodlpine. NCEP ATP III: national cholesterol education program adult treatment panel guideline III, JNC: Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. |
 | Fig. 2Tolerability of amlodipine/atorvastatin compared with single-agent therapy or placebo. The graph shows adverse events in patients with co-existing hypertension and dyslipidemia who were randomized to once-daily amlodipine plus atorvastatin (any of eight dose combinations; n=885), amlodipine (5 or 10 mg alone; n=221), atorvastatin (10, 20, 40, or 80 mg alone; n=443), or placebo (n=111) in the double-blind, double-dummy, multicenter RESPOND trial. |
 | Fig. 3Two-to-four antihypertensive agents are required to achieve effective BP control to target levels. BP: blood pressure, DBP: diastolic blood pressure, MAP: mean arterial pressure, SBP: systolic blood pressure. |
 | Fig. 4Comparison of the antihypertensive effects of irbesartan/HCTZ (150/12.5 mg) and valsartan/HCTZ (80/12.5 mg) in hypertensive patients in the COmparative Study of Efficacy of Irbesartan/HCTZ with Valsartan/HCTZ Using Home Blood Pressure Monitoring in the TreAtment of Mild-to-Moderate Hypertension (COSIMA) study.22) *p=0.0317, †p=0.0002, ‡p=0.0005, §p<0.0001. Error bars represent 95% Confidence Intervals. n: number controlled, HCTZ: hydrochlorothiazide. |
 | Fig. 5Rates of (A) total AEs, (B) total discontinuations, and (C) total discontinuations as a result of AEs in the groups that received valsartan (160 mg) plus hydrochlorothiazide (12.5 mg [V+HCTZ12.5]), valsartan (160 mg) plus HCTZ (25 mg [V+HCTZ 2S]), and amlodipine (10 mg [A10]). *p<0.05 vs. combination-therapy groups. HCTZ: hydrochlorothiazide. |
Table 1
Summary of the pharmacodynamic effects of amlodipine (AML), atorvastatin (ATO), or a combination of AML and ATO on endothelial cell function and atherosclerotic plaque

Table 4
Efficacy: blood pressure-lowering effects of drugs when used at one-half standard dose separately and in combination. The reductions with two and three drugs are based on an additive effect

References
1. Kannel WB. Fifty years of Framingham Study contributions to understanding hypertension. J Hum Hypertens. 2000. 14:83–90.
2. Health Survey for England. 1998. Available at http://www.archive.official-documents.co.uk/document/doh/survey98/hse-00.htm.
3. Asmar R, Vol S, Pannier B, Brisac AM, Tichet J, El Hasnaoui A. High blood pressure and associated cardiovascular risk factors in France. J Hypertens. 2001. 19:1727–1732.
4. Chapman RH, Benner JS, Petrilla AA, et al. Predictors of adherence with antihypertensive and lipid-lowering therapy. Arch Intern Med. 2005. 165:1147–1152.
5. Agarwal S, McLaughlin T, Joyce A, Schwartz S, Tang S. Synchronizing antihypertensive and lipid-lowering therapies increases patient adherence. J Clin Hypertens. 2006. 8:Suppl A5. A214(P-519). Abstract.
6. Dezii CM. A retrospective study of persistence with single-pill combination therapy vs. concurrent two-pill therapy in patients with hypertension. Manag Care. 2000. 9:Suppl. 2–6.
7. Safran DG, Neuman P, Schoen C, et al. Prescription drug coverage and seniors: findings from a 2003 national survey. Health Aff (Millwood). 2005. Suppl Web Exclusives:W5-152–W5-66.
8. Lee YS, Kim KS. The short-term effect of atorvastatin on flow-mediated vasodilation, pulse wave velocity and carotid intimamedia thickness in patients with moderate cholesterolemia. Korean Circ J. 2008. 38:144–151.
9. Blank R, LaSalle J, Reeves R, Maroni J, Tarasenko L, Sun F. Single pill therapy in the treatment of concomitant hypertension and dyslipidemia (the Amlodipine/Atorvastatin Gemini Study). J Clin Hypertens (Greenwich). 2005. 7:264–273.
10. Chung M, Calcagni A, Glue P, Bramson C. Effect of food on the bioavailability of amlodipine besylate/atorvastatin calcium combination tablet. J Clin Pharmacol. 2006. 46:1212–1216.
11. Chun KJ, Chung NS, Ha JW, et al. Efficacy and safety of atorvastatin in patients with elevated LDL-cholesterolemia. Korean Circ J. 1999. 29:1309–1316.
12. Fogari R, Derosa G, Lazzari P, et al. Effect of amlodipine-atorvastatin combination on fibrinolysis in hypertensive hypercholesterolemic patients with insulin resistance. Am J Hypertens. 2004. 17:823–827.
13. Preston RA, Sun F, Tarasenko L. Safety and tolerability of coadministered amlodipine and atorvastatin in patients with concomitant hypertension and dyslipidemia in the Respond study. Am J Hypertens. 2005. 18:A92–A93. Abstract.
14. Materson BJ, Reda DJ, Cushman WC. Department of veterans Affairs single-drug therapy of hypertension study: revised figures and new data. Am J Hypertens. 1995. 8:189–192.
15. Morgan TO, Anderson AI, MacInnis RJ. ACE inhibitors, beta-blockers, calcium blockers, and diuretics for the control of systolic hypertension. Am J Hypertens. 2001. 14:241–247.
16. Mancia G, De Backer G, Dominiczak A, et al. 2007 Guidelines for the Management of Arterial Hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2007. 25:1105–1187.
17. Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003. 289:2560–2572.
18. Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. N Engl J Med. 2000. 342:145–153.
19. Lip GY, Hall JE. Comprehensive Hypertension. 2007. 1st ed. Philadelphia: Mosby Elsevier;1061–1065.
20. Bangalore S, Kamalakkannan G, Parkar S, Messerli FH. Fixed-dose combinations improve medication compliance: a meta-analysis. Am J Med. 2007. 120:713–719.
21. Law MR, Wald NJ, Morris JK, Jordan RE. Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ. 2003. 326:1427.
22. Bobrie G, Delonca J, Moulin C, et al. A home blood pressure monitoring study comparing the antihypertensive efficacy of two angiotensin II receptor antagonist fixed combinations. Am J Hypertens. 2005. 18:1482–1488.
23. Flack JM. Maximising antihypertensive effects of angiotensin II receptor blockers with thiazide diuretic combination therapy: focus on irbesartan/hydrochlorothiazide. Int J Clin Pract. 2007. 61:2093–2102.
24. Ruilope LM, Malacco E, Khder Y, Kandra A, Bonner G, Heintz D. Efficacy and tolerability of combination therapy with valsartan plus hydrochlorothiazide compared with amlodipine monotherapy in hypertensive patients with other cardiovascular risk factors. Clin Ther. 2005. 27:578–587.
25. Andreadis EA, Tsourous GI, Marakomichelakis GE, et al. High-dose monotherapy vs low-dose combination therapy of calcium channel blockers and angiotensin receptor blockers in mild to moderate hypertension. J Hum Hypertens. 2005. 19:491–496.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download