Abstract
Background and Objectives
Myocardial injury after percutaneous coronary intervention (PCI) occurs frequently and it is associated with an adverse clinical outcome. Mechanical factors have been implicated in this complication and the role of inflammation has not yet been clearly determined. We evaluated the effect of an inflammatory response during PCI on periprocedural myocardial injury.
Subjects and Methods
We prospectively studied 231 patients (mean age: 62.8±10.6 years, males: 60.6%) who underwent elective coronary stenting. For the exclusion of mechanical injury to the myocardium, we excluded those patients who developed complications during PCI. Blood samples for measuring the high sensitivity C-reactive protein (hsCRP) and troponin T (TnT) were obtained before the procedure and at 6 hours and 24 hours after PCI. The inflammatory response to PCI was calculated as the difference between the peak postprocedural hsCRP level and the preprocedural hsCRP level (delta CRP). We divided the patients according to the median value of delta CRP: Group I <2.2 mg/dL and Group II ≥2.2 mg/dL.
Results
Postprocedural TnT elevation was were observed in 72 (31.2%) patients. The baseline clinical and angiographic characteristics were not difference between the two groups. The incidence of any TnT elevations was higher in the Group II than that in Group I (19.8% vs 42.6%, respectively, p<0.001). The incidences of TnT levels over 3 times the upper normal limit and 5 times the upper normal limit were also higher in Group II than in Group I (11.2% vs 21.7%, respectively, p=0.031, for a TnT level 3 times the upper normal limit, and 6.0% vs 13.9%, respectively, for a TnT level 5 times the upper normal limit). Multivariate analysis revealed that postprocedural hsCRP elevation and complex lesion were the significant independent predictors of postprocedural TnT elevation.
During the past three decades, percutaneous coronary intervention (PCI) has become one of the cardinal treatment strategies for stenotic coronary artery disease. As PCI has developed, it has decreased the incidence of major adverse cardiac events for patients with coronary artery disease. However, the incidence of post-procedural cardiac marker elevation has not decreased, in spite of the improved outcome of PCI.1)
The relatively low-level release of cardiac enzymes after PCI occurs in about 25% of the patients treated with stents.2-4) It was demonstrated that periprocedural myocardial injury is associated with a worse long-term clinical outcome.5-7) Cardiac troponin T and I were consistently found to be more sensitive than creatinine kinase-MB (CK-MB) for detecting myocardial injury in this setting.8)9)
Vascular injury during PCI is associated with a systemically measurable inflammatory response, and the degree of inflammation has been shown to correlate with the cardiovascular risk.10)11) C-reactive protein (CRP) is an acute-phase reactant and it is the most widely used marker of systemic inflammation. Although the mechanism is unclear, elevated preprocedural CRP levels have been associated with an increased risk for short- and long-term cardiac events.12-14) However, little is known regarding the role of the inflammatory response during PCI and the periprocedural myocardial injury. Therefore, we prospectively studied the inflammatory response to coronary stenting, as estimated by the serial CRP changes and the periprocedural myocardial injury.
We prospectively studied patients who underwent elective coronary stenting. The exclusion criteria included 1) an elevated troponin T level before the procedure; 2) known inflammatory, neoplastic or infectious disease; 3) myocardial infarction (MI) within 1 month before the procedure and 4) inflammatory or infectious signs after PCI. All the patients gave us an informed written consent according to a protocol approved by the Ethical Committee of Wonkwang University Hospital.
PCI was performed according to the standards of current clinical practice at the physician's discretion. We used drug-eluting stent in all patients. The patency of the treated artery on the diagnostic coronary angiography was evaluated by the thrombolysis in myocardial infarction (TIMI) score. Angiographic success of PCI was defined as TIMI III flow with any residual stenosis below 20%.
All the patients received a loading dose of aspirin (300 mg/day) and clopidogrel (300 mg/day) before the procedure. An intra-venous bolus of 5,000 U of unfractionated heparin was given, and then additional heparin boluses were given to maintain an activated clotting time of >300 s during the procedure. To exclude those patients with mechanical injury to the myocardium, we excluded the patients who developed complications during PCI. The complications consisted of slow flow, any visible side branch occlusion, distal embolization and major dissection.
Venous blood samples were obtained before intervention and at 6 and 24 hours after the procedure for troponin T and CRP determination. The cut-off value for abnormal cardiac troponin T was 0.1 ng/mL. High-sensitivity assay was used to measure the CRP concentration. The inflammatory response to coronary stenting was calculated as the difference between the peak postprocedural CRP level and the preprocedural CRP level (ΔCRP). We divided the patients according to the median value of delta CRP: Group I <2.2 mg/dL and Group II ≥2.2 mg/dL.
All measurements are represented as means (standard deviations. Inter-group analysis was done using independent t-tests and (2 tests, which were conducted using SPSS 11.0 for Window (SPSS Inc., Chicago, IL). A multivariable logistic regression model was constructed for predicting troponin elevation after PCI. The following variables, which were selected according to the literature data1 and they were significant on univariate analysis, were inserted into the logistic regression analysis: age, complex lesion, multivessel stenting, the stent length and number, the preprocedural CRP levels and ΔCRP, diabetes, no prior use of statin, the LDL cholesterol level and the serum creatinine level. For continuous variables, the median value was used as a cut-off point to define the two subgroups on the logistic regression analysis. Statistical significance was set at p<0.05.
The study population included 247 patients who underwent elective coronary angiography followed by coronary stenting between March 2005 and November 2006. For excluding those patients with mechanical injury to the myocardium, we excluded the patients who developed complication during PCI such as slow flow (4 cases), side branch occlusion (11 cases), and major dissection (1 case). Overall, 231 patients (mean age: 62.8±10.6 years, males: 60.6%) were enrolled in this study. The clinical diagnoses in admission were silent ischemia in 46 patients (19.9%) and stable angina in 185 patients (80.1%).
The mean ΔCRP was 6.6±11.5 mg/dL, and the median value was 2.2 mg/dL. We divided the patients according to the median value of the delta CRP: Group I <2.2 mg/dL and Group II ≥2.2 mg/dL. The baseline clinical characteristics and angiographic data are described in Table 1 and 2. There was no significant difference of the most relevant clinical characteristics between the two groups (Table 1).
We used drug-eluting stents in all the patients. None of the patients were received glycoprotein IIb/IIIa inhibitors. The mean stent length and number of stents were similar between the two groups (Table 2). Multivessel stenting was more frequently performed in Group II than in Group I.
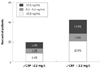
Postprocedural myocardial infarction (CK-MB elevation >3 times the upper normal limit) occurred in 2 cases (1.7%) in Group I and in 2 cases (1.7%) in Group II. Neither in-hospital death nor Q-wave MI was developed by any patients. Cardiac troponin T elevation was detected after coronary intervention in 72 (31.2%) patients (Fig. 1). The incidence of any TnT elevation was higher in the Group II than that in Group I (19.8% vs 42.6%, respectively, p<0.001). The incidence of TnT over 3 times the upper normal limit and over 5 times the upper normal limit was also higher in the Group II than that in Group I (11.2% vs 21.7%, respectively, p=0.031 for the TnT over 3 times the upper normal limit, and 6.0% vs 13.9%,
Multivariate analysis revealed that postprocedural hsCRP elevation (OR 2.5, 95% CI 1.3-4.6, p=0.005) and complex lesion (OR 2.3, 95% CI 1.0-5.3, p=0.043) were significantly associated with postprocedural TnT elevation (Table 3).
In this study, we showed that elevated hsCRP levels were associated with a higher risk of postprocedural troponin elevation in patients undergoing uncomplicated PCI. This finding is important because a higher degree of postprocedural myonecrosis is associated with an increased risk of adverse events during follow-up.
Vascular injury during PCI is associated with a systemic inflammatory response, and the degree of inflammation has been shown to correlate with the cardiovascular risk.10)11) Preprocedural elevation of the CRP levels has recently emerged as a clinical predictor for periprocedural myocardial injury. The increase in the serum CRP concentration follows the increase in the serum IL-6 concentration by 12-36 hours, and the serum CRP concentration reaches its peak value by 24 hours after the procedure.15)16) Bonz et al.16) found the increase in the serum concentrations of both IL-6 and CRP to be more obvious in patients with concomitant post-procedural troponin T elevation. Saadeddin et al.17) reported preprocedural CRP elevation in 41% of 85 patients with stable angina and who undergoing PCI, and this was associated with a 2.27-fold higher risk of developing periprocedural myocardial injury, and the latter was defined by a postprocedural troponin I elevation of >2 ng/mL. Ellis et al.18) confirmed a nearly 4-fold higher preprocedural CRP level among the patients who developed postprocedural CK-MB elevation. Additionally, Hong et al.19) demonstrated that elevated preprocedural CRP levels are associated with neointimal hyperplasia and restenosis after PCI.
Yet contradictory results have reported. Gaspardone et al.20) excluded the patients with any postprocedural cardiac marker elevation and they still found CRP elevation (>0.5 mg/dL) within 48 hours after PCI in 99% of these patients. Saleh et al.21) reported no significant relationship between CRP and postprocedural troponin elevation in patients with stable or unstable angina. More recently, Gach et al.22) reported no correlation between the delta CRP and the delta troponin in stable angina patients. In our study, the baseline CRP level was similar between the two groups, yet the inflammatory response (ΔCRP) during intervention was more associated with periprocedural myocardial injury. Although the subsets of patients or their medications in our study were different from those of other studies, our results consolidated the association between CRP and the troponin changes during PCI.
Different strategies such as platelet GP IIb/IIIa inhibitors and high dose clopidogrel and statin have been proposed and tested to prevent peri-procedural myocardial infarction.23-25) Many studies have demonstrated that early statin therapy among PCI patients is associated with significant advantages for decreased mortality and morbidity in different patient subsets.10,26-28) Although the mechanism is not entirely clear, the anti-inflammatory effects of statins might contribute to the reduced myocardial injury during PCI. In the present study, prior statin therapy had no significant effect on postprocedural troponin elevation. However, only 12% of all the study patients were receiving prior statin therapy, and this lowered the power to detect differences between the patients with and without statin therapy.
The results of the present study suggest that systemic factors may affect the susceptibility to postprocedural troponin elevations. With excluding mechanical causes, structural and functional microvascular obstruction have been implicated in most cases of postprocedural myonecrosis.1)29) Thus, CRP may be related to such pathological conditions as friability and hypercoagulability of the atheromatous lesion, which predispose to a patient to microembolization or clot formation at the site of the PCI-induced arterial injury. Systemic inflammation also provides a link between PCI-associated infarction and long-term events, the same as was reported by previous studies.30) So, other therapeutic strategies that can inhibit the inflammatory response are needed to prevent periprocedural myocardial injury.
In conclusion, elevated hsCRP levels were associated with a higher risk of postprocedural troponin elevation in those patients who are undergoing uncomplicated PCI. These results emphasized the role of inflammation in the pathogenesis of periprocedural myocardial injury.
Figures and Tables
Fig. 1
Incidence of postprocedural troponin T elevations >1, 3 to 5, and >5 times above the upper normal limit according to the delta C-reactive protein (CRP).
References
1. Herrmann J. Peri-procedural myocardial injury: 2005 update. Eur Heart J. 2005. 26:2493–2519.
2. Brener SJ, Ellis SG, Schneider J, Topol EJ. Frequency and long-term impact of myonecrosis after coronary stenting. Eur Heart J. 2002. 23:869–876.
3. Fujii K, Carlier SG, Mintz GS, et al. Creatinin kinase-MB enzyme elevation and long-term clinical events after successful coronary stenting in lesions with ruptured plaque. Am J Cardiol. 2005. 95:355–359.
4. Herrmann J, von Birgelen C, Haude M, et al. Prognostic implication of cardiac troponin T increase following stent implantation. Heart. 2002. 87:549–553.
5. Kornowski R, Fuchs S, Hong MK, et al. Prognostic value of recurrent episodes of creatine kinase-MB elevation following repeated catheter-based coronary interventions. Catheter Cardiovasc Interv. 2000. 51:131–137.
6. Ghazzal Z, Ashfaq S, Morris DC, et al. Prognostic implication of creatine kinase release after elective percutaneous coronary intervention in the pre-IIb/IIIa antagonist era. Am Heart J. 2003. 145:1006–1012.
7. Stone GW, Mehran R, Dangas G, Lansky AJ, Kornowski R, Leon MB. Differential impact on survival of electrocardiographic Q-wave versus enzymatic myocardial infarction after percutaneous intervention: a device-specific analysis of 7147 patients. Circulation. 2001. 104:642–647.
8. Garbarz E, Iung B, Lefevre G, et al. Frequency and prognostic value of cardiac troponin I elevation after coronary stenting. Am J Cardiol. 1999. 84:515–518.
9. Shyu KG, Kuan PL, Cheng JJ, Hung CR. Cardiac troponin T, creatine kinase, and its isoform release after successful percutaneous transluminal coronary angioplasty with or without stenting. Am Heart J. 1998. 135:862–867.
10. Chan AW, Bhatt DL, Chew DP, et al. Early and sustained survival benefit associated with statin therapy at the time of percutaneous coronary intervention. Circulation. 2002. 105:691–696.
11. Kim YC, Sung KC, Park SH, et al. The effect of systemic inflammation on the elevation of troponin I after percutaneous transluminal coronary angioplastry with stent in patients with stable angina. Korean Circ J. 2004. 34:265–270.
12. Chew DP, Bhatt DL, Robbins MA, et al. Incremental prognostic value of elevated baseline C-reactive protein among established markers of risk in percutaneous coronary intervention. Circulation. 2001. 104:992–997.
13. Choi SY, Yang HM, Tahk SJ, et al. Preprocedural hs-CRP level serves as a marker for procedure-related myocardial injury during coronary stenting. Korean Circ J. 2005. 35:140–148.
14. Buffon A, Liuzzo G, Biasucci LM, et al. Preprocedural serum levels of C-reactive protein predict early complications and late restenosis after coronary angioplasty. J Am Coll Cardiol. 1999. 34:1512–1521.
15. Sanchez-Margalet V, Cubero JM, Martin-Romero C, Cubero J, Cruz-Fernandez JM, Goberna R. Inflammatory response to coronary stent implantation in patients with unstable angina. Clin Chem Lab Med. 2002. 40:769–774.
16. Bonz AW, Lengenfelder B, Jacobs M, et al. Cytokine response after percutanous coronary intervention in stable angina: effect of selective glycoprotein IIb/IIIa receptor antagonism. Am Heart J. 2003. 145:693–699.
17. Saadeddin SM, Habbab MA, Sobki SH, Ferns GA. Association of systemic inflammatory state with troponin I elevation after elective uncomplicated percutaneous coronary intervention. Am J Cardiol. 2002. 89:981–983.
18. Ellis SG, Chew D, Chan A, Whitlow PL, Schneider JP, Topol EJ. Death following creatine kinase-MB elevation after coronary intervention: identification of an early risk period: importance of creatine kinase-MB level, completeness of revascularization, ventricular function, and probable benefit of statin therapy. Circulation. 2002. 106:1205–1210.
19. Hong YJ, Jeong MH, Lim SY, et al. Elevated preprocedural high-sensitivity C-reative protein levels are associated with neointimal hyperplasia and restenosis development after successful coronary artery stenting. Circ J. 2005. 69:1477–1483.
20. Gaspardone A, Crea F, Versaci F, et al. Predictive value of C-reactive protein after successful coronary-artery stenting in patients with stable angina. Am J Cardiol. 1998. 82:515–518.
21. Saleh N, Svane B, Velander M, Nilsson T, Hansson LO, Tornvall P. C-reactive protein and myocardial infarction during percutaneous coronary intervention. J Intern Med. 2004. 255:33–39.
22. Gach O, Legrand V, Biessaux Y, Chapelle JP, Vanbelle S, Pierard LA. Long-term prognostic significance of high-sensitivity C-reactive protein before and after coronary angioplasty in patients with stable angina pectoris. Am J Cardiol. 2007. 99:31–35.
23. Lincoff AM, Tcheng JE, Califf RM, et al. Sustained suppression of ischemic complications of coronary intervention by platelet GP IIb/IIIa blockade with abciximab: one-year outcome in the EPILOG trial: evaluation in PTCA to improve long-term outcome with abciximab GP IIb/IIIa blockade. Circulation. 1999. 99:1951–1958.
24. Patti G, Colonna G, Pasceri V, Pepe LL, Montinaro A, Di Sciascio G. Randomized trial of high dose of clopidogrel for reduction of periprocedural myocardial infarction in patients undergoing coronary intervention: results from the ARMYDA-2 (Antiplatelet therapy for Reduction of Myocardial Damage during Angioplasty) study. Circulation. 2005. 111:2099–2106.
25. Bonz AW, Lengenfelder B, Strotmann J, et al. Effect of additional temporary glycoprotein IIb/IIIa receptor inhibition on troponin release in elective percutaneous coronary interventions after pretreatment with aspirin and clopidogrel (TOPSTAR trial). J Am Coll Cardiol. 2002. 40:662–668.
26. Herrmann J, Lerman A, Baumgart D, et al. Periprocedural statin medication reduces the extent of periprocedural non-Q-wave myocardial infarction. Circulation. 2002. 106:2180–2183.
27. Chang SM, Yazbek N, Lakkis NM. Use of statin prior to percutaneous coronary intervention reduces myonecrosis and improves clinical outcome. Catheter Cardiovasc Interv. 2004. 62:193–197.
28. Veselka J, Prochazkova S, Duchonova R, Homolova I, Tesar D, Bybee KA. Preprocedural statin therapy reduces the risk and extent of cardiac biomarker release following percutaneous coronary intervention. Heart Vessels. 2006. 21:146–151.
29. Topol EJ, Yadav JS. Recognition of the importance of embolization in atherosclerotic vascular disease. Circulation. 2000. 101:570–580.
30. Zebrack JS, Muhlestein JB, Horne BD, Anderson JL. C-reactive protein and angiographic coronary artery disease: independent and additive predictors of risk in subjects with angina. J Am Coll Cardiol. 2002. 39:632–637.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download