It is widely known that hypertension increases the risk of adverse cardiovascular events. High blood pressure raises the possibility of events caused by cardiovascular diseases, and if the systolic blood pressure is over 115 mmHg or the diastolic blood pressure is over 75 mmHg, then the blood pressure and cardiovascular events show a linear relationship with each other.1) It is known that an increase of systolic blood pressure by 20 mmHg or increasing the diastolic blood pressure by 10 mmHg doubles the mortality caused by ischemic heart diseases or strokes. However, blood pressure is not fixed, but it changes continuously according to the acute or chronic changes of various external factors. Therefore, when predicting the cardiovascular risks posed by blood pressure, it is believed that it is more reliable to measure blood pressure not just once in an office, but for 24 hours through ambulatory blood pressure monitoring. In addition, there is increasing interest in various patterns of the variation or reactivity of blood pressure (exaggerated blood pressure responsiveness to external stimuli, an abnormal response to the diurnal rhythm, seasonal variations of blood pressure, etc.), and many researches have been conducted to see if such patterns are related to the increase of cardiovascular risks. The present review purposed to examine the meanings of the changes in the pattern of blood pressure variation.
Blood Pressure Reactivity to External Stimuli
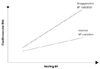
The blood pressure changes and it is sensitive to external stimuli (emotional stress, exercise, the change of posture, etc.). Blood pressure reactivity does not necessarily increase at high blood pressure, and high blood pressure reactivity is known to increase the cardiovascular risks (Fig. 1).2-6) The white coat effect is also related to this fact and exaggerated blood pressure responses are sometimes observed during exercise.7) A rise in the exercise systolic blood pressure to >200 mmHg during the first 6 minutes of bicycle exercise predicts a doubling of the cardiovascular disease incidence in middle-aged men. Exaggerated blood pressure reactivity is caused by the augmentation of the sympathetic nervous system, vascular abnormalities (endothelial dysfunction, increased arterial stiffness), a lowered ability to cope with stress and dysfunction of the aortocarotid baroreflex.8) In the case of normal blood pressure or young hypertensive patients, the cardiac output is increased by external stimuli and a related increase in pulse pressure is observed. On the contrary, old hypertensive patients or chronic hypertensive patients show the lability of systolic blood pressure and this is explained with the increase of their arterial stiffness. In addition, arterial stiffness is believed to contribute to a blunted baroreflex and an increase of sympathetic activity. Moreover, it is known that hypercholesterolemia or insulin resistance related to endothelial dysfunction raises the blood pressure reactivity, and high blood pressure reactivity can be improved by treating these risk factors with using statin or thiazolidinedione.9) Further, exercise is known to restore the baroreflex, endothelial function and arterial compliance, and exercise consequently lessens the blood pressure reactivity. As described above, the white coat effect (an abnormal rise of blood pressure when the blood pressure is measured in an office) can be explained by the blood pressure reactivity. According to a previous study, when blood pressure is measured using a cuff, then the increase of blood pressure varies widely and the systolic blood pressure increases by 0-50 mmHg.10)
Circadian Variation in Blood Pressure
Diurnal blood pressure variation over time can be typically characterized by a 10 mmHg decrease during the nighttime, and this diurnal variation is believed to come from changes in the sympathetic nervous system activity, the renin-angiotensin system activity and the salt-volume balance.11-13) If blood pressure rises excessively during the process of variation through a day, then this is related to the occurrence of cardiovascular events. It has been reported that the morning surge, which is the excessive increase of blood pressure just after rising in the morning, is related to the time of the occurrence of cardiovascular events, to many cases of myocardial infarction and ischemia, to sudden cardiac death and to stroke that occurs in the morning. Diurnal variation is observed not only in the blood pressure, but also in other physiological phenomena. The heart rate, sympathetic neurotransmission, vascular tone, platelet aggregability and the coagulation parameters have also shown harmful changes in the morning, which contributes to the occurrence of cardiovascular events.
It is known that compared to the patients who show a normal nocturnal blood pressure decrease (dippers), those patients whose nocturnal blood pressure decrease is small (less than 10 mmHg, non-dippers) have higher cardiovascular risks,14) and the prognosis is worse for those patients whose nocturnal blood pressure is higher than the daytime blood pressure (risers or reverse dippers).15) However, it was reported that lacunar stroke and silent myocardial ischemia occur frequently in people whose nocturnal blood pressure decrease is over 20 mmHg (extreme-dippers).12)13) As mentioned earlier, there have been reports that if the circadian variation is high through the day, that is, if the rise of blood pressure in the morning is excessive (morning surge), then the cardiovascular risks increase. According to a previous report, the risk of stroke is 2.7 times higher in old hypertensive patients who show a morning blood pressure surge (>55 mmHg difference between the mean systolic blood pressure during the 2 hours after waking and arising minus the mean systolic blood pressure during the hour that included the lowest blood pressure during sleep).16)
The causes of abnormal circadian variation are as various as the patterns of variation. Arterial stiffness is an independent predictor of cardiovascular risks in hypertensive patients,17) and this is particularly remarkable in the aged. However, there is no clear mechanism that can explain the relation between arterial stiffness and the cardiovascular death rate. According to recent researches, arterial stiffness is believed to be related to circadian blood pressure variation. That is, it is believed that blood pressure variation is high in the elderly whose arterial stiffness has been increased and that extremedippers have both the increase of arterial stiffness and the decrease of circulating blood volume. It has been known that increased blood pressure reactivity is associated with exaggerated cyclic variation of blood pressure.
Seasonal Variation in Blood Pressure
With the seasonal change of temperature, the frequencies of cardiovascular diseases also change from season to season. Diseases such as acute myocardial infarction, ischemic and hemorrhagic stroke, and aortic rupture or dissection more frequently take place during the winter.18-20) According to data from the US National Registry of Myocardial Infarction, the frequency of acute myocardial infarction increases by 53% in the winter.18) Compared to that noted in the summer, the blood pressure rises in the winter.21) In addition, if one is exposed to coldness, sympathetic activity increases and the circulatory system goes into a pro-thrombotic state; as a result, the fibrinogen level rises by up to 23%.22) Moreover, the platelet count and the red blood cell count go up and the blood viscosity is also increased.23) These changes are related to the increase in the incidence of cardiovascular diseases during the winter, but in particular, the seasonal variation of blood pressure is considered the most important influential factor and exaggerated seasonal blood pressure variation is thought to be related to increased cardiovascular risk. The seasonal variation of blood pressure is observed in normal people as well,24) but it is known to be severe in hypertensive patients,21)25) the elderly,26)27) smokers28) and thin people.29) Seasonal variation is also related to factors affecting circadian variation, and arterial stiffness is known to independently increase the seasonal variation of blood pressure.30)
Conclusion
Not only the absolute value of blood pressure, but also the patterns of its excessive variation are closely related to the occurrence of cardiovascular events, so these patterns are clinically important. It may be difficult to explain the exact mechanisms of various abnormal short-term and long-term blood pressure variations at present. But several common hypotheses that include the sympathetic nervous system and the increase of arterial stiffness have been suggested as the causes of abnormal blood pressure variations. Efforts to understand these underlying disease mechanisms and to normalize blood pressure variation are expected to contribute to further reducing the cardiovascular risks, in addition to administering the currently available blood pressure treatments.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download