Introduction
In patients with situs inversus totalis, the superior vena cava is normally positioned on the left side and drains into a left-sided right atrium (RA). If these patients also have right superior vena cava (RSVC), it should be thought of as a combined congenital anomaly. This venous anomaly can often be recognized during the implantation of a pacemaker or implantable cardioverter defibrillator (ICD), and it also can be used as a route for lead access.1) Here, we present a case of successful pacemaker lead revision through the RSVC in a patient with situs inversus totalis.
Case
A 44-year-old woman was admitted to our hospital for pulse generator revision. She had previously been diagnosed with congenitally corrected transposition of the great arteries with situs inversus totalis. She had undergone atrial septal defect patch closure and aortic valve replacement (AVR) due to severe aortic regurgitation 18 years earlier. In the operation field, both right and left superior vena cava had been observed. The left superior vena cava (LSVC) was 0.5 cm in size and drained directly to a left-sided right atrium (RA); the RSVC was 3 cm in size and drained to the RA via an enlarged coronary sinus. Fifteen years earlier, she complained of dizziness during the postoperative care of redo AVR. Her electrocardiography (ECG) showed complete atrioventricular (AV) blockage. She underwent permanent VVI pacemaker implantation through the LSVC (Fig. 1).
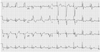
During the follow-up, pacemaker interrogation revealed that replacement of the pulse generator was indicated, although the pacing was still working (Fig. 2). Echocardiography showed corrected transposition of great arteries (TGA) and slightly depressed function of the right-sided left ventricle, with an estimated ejection fraction of 45%. There were no intra-cardiac shunts and the prosthetic aortic valve had normal function. The coronary sinus was enlarged, and its diameter was 1.6 cm. During the revision procedure, we noticed that the pacing threshold of the ventricular lead was greater than 5 V and the lead impedance was 750 ohm. Thus, we planned to insert a new pacemaker lead. After puncturing the left axillary vein, we attempted to insert a guide wire into the LSVC. However, the LSVC was obstructed (Fig. 3A), so we decided to use the RSVC for the insertion of a new lead. In spite of its long distance and tortuosity, we were able to insert a lead through the RSVC (arrowheads in Fig. 3B) and successfully placed the new lead on the left-sided RV apex (Fig. 4). Pacemaker interrogation showed that the impedance and threshold were 742 ohm and 0.3 V, respectively. The patient was discharged 4 days after the procedure. At one month follow-up, the pacing status was good (impedance 850 ohm; threshold <0.5 V), and the follow-up ECG showed that the pacemaker was functioning well (Fig. 5).
Discussion
Situs inversus is a rare congenital condition in which major visceral organs are reversed or mirrored from their normal position. If the heart is swapped to the right side of the thorax, it is known as situs inversus totalis. Compared to LSVC with situs solitus, there have been few reports on RSVC in patients with situs inversus.2) In patients with situs solitus, LSVC is an asymptomatic and infrequently observed anomaly. Its prevalence in the general population is approximately 0.3%,2) while it is much higher in patients with congenital cardiac abnormalities, ranging from 2.8% to 4.3%.3)4) The incidence was not different (0.47%) in patients undergoing implantation of a pacemaker or implantable cardioverter defibrillator.5) LSVC is the most common form of anomalous venous drainage involving SVC, which results from the failure of the left common cardinal vein to become occluded.6) In most cases, blood drains into the right atrium via an enlarged coronary sinus,6) but in 8% of patients, it drains directly into the left atrium through a defect in the form of an unroofed coronary sinus.7) The RSVC was absent in 1% of patients with persistent LSVC, and is frequently associated with alteration of cardiac situs.8) Associated cardiac anomalies include stenosis or atresia of the pulmonary artery, D-transposition, complete atrioventricular septal defects, anomalous pulmonary vein drainage, and cor triatriatum.9-12)
Persistence of LSVC in patients with situs solitus is almost always found incidentally during an invasive procedure such as central catheter insertion or pacemaker and ICD implantation. In pacemaker implantation, the most common problems related to the unusual anatomic access to the heart were reaching a convenient pacing site and ensuring stable lead placement.13-15) Once the RA is reached, further placement of the lead to the RV is not easy because of acute angulation between the coronary sinus and the tricuspid valve opening. During the pacemaker revision for this case, the pacemaker lead could not be easily placed in the right ventricle using LSVC. Fortunately, the RSVC drained into the right atrium, and we were able to successfully insert pacemaker leads into the apex of the RV through the RSVC and the coronary sinus.
To the best of our knowledge, this is the first report on pacemaker lead insertion through the RSVC in a patient with situs inversus totalis.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download