Abstract
Background and Objectives
The presence of elevated troponin after percutaneous coronary intervention (PCI) is considered to reflect irreversible myocardial injury. However, its prognostic value remains unclear. The purpose of this study was to investigate the incidence, risk factors, and clinical outcomes of troponin I (TnI) elevation after the implantation of drug-eluting stent (DES).
Subjects and Methods
We performed a retrospective analysis of 335 patients who had undergone PCI with DES. Patients who had acute coronary syndrome with elevated TnI levels before PCI were excluded. TnI levels were measured 6 and 24 hours after PCI.
Results
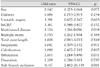
Baseline clinical characteristics were similar in the elevated TnI and normal TnI groups. Elevated postprocedural TnI (>1.5 ng/mL) occurred in 52 patients (15.5%). Univariate analysis revealed that the clinically significant variables were multi-vessel disease (p<0.001), multiple stent implantation (p=0.003), total stent length (p=0.001), side-branch occlusion (p<0.001), and bifurcation lesion (p=0.003). Multivariate analysis indicated that the independent predictors of elevated TnI after DES implantation were multi-vessel disease (p=0.019), side-branch occlusion (p=0.001), and bifurcation (p=0.011). There were no significant differences in major adverse cardiovascular events between the elevated TnI and normal TnI groups (p=0.461).
The elevation of troponin I (TnI) after successful percutaneous coronary intervention (PCI) is relatively common, and directly reflects the extent of irreversible myocardial injury.1)2) The mechanisms responsible for the elevation of TnI after PCI have been identified as distal embolization, side-branch occlusion, and prolonged balloon inflation.1-6) Several studies have shown varying incidences and independent predictors of elevated TnI following PCI.5-8)
Although it is widely accepted that the elevation of creatine kinase (CK)-MB after PCI increases the incidence of cardiac events and mortality,9-14) the prognostic significance of the elevation of troponin after PCI is less well-established. Some studies have reported that postprocedural troponin elevation is not associated with worse clinical outcomes,6)15-18) whereas other studies have suggested that it has prognostic significance.19-21) However, few studies have included cases of PCI with drug-eluting stent (DES).
The aim of this study was to assess the incidence and predictive factors of TnI elevation after implantation of DES, and to investigate whether the elevation of TnI after PCI using DES is associated with poor clinical outcomes.
The patient cohort included a consecutive series of patients who had undergone PCI with DES between October 2003 and April 2005 at KangNam St. Mary's Hospital. All patients had experienced ischemic chest symptoms and coronary artery stenosis of more than 50% of the luminal diameter on coronary angiography. Baseline clinical, procedural, and angiographic data were collected for all patients.
Exclusion criteria were: 1) ST elevation with myocardial infarction in the two weeks before PCI; 2) elevated preprocedural TnI levels; 3) serum creatinine levels >1.5 mg/dL; 4) left ventricular (LV) ejection fraction of <40%; or 5) unavailable TnI results. The study protocol was approved by the institutional review board at our hospital, and all of our patients gave their written informed consent for the coronary procedure.
A total of 518 patients were initially considered for inclusion in the study, 335 of whom were considered eligible. One hundred and eighty-three patients were excluded for the following reasons: myocardial infarction with ST segment elevation on admission (n=52), elevated preprocedural TnI levels (n=106), renal insufficiency (n=9), significant LV systolic dysfunction (n=12), and unavailable TnI results at 6 or 24 hours after PCI (n=4). Finally, 335 patients with 466 stented coronary vessels were available for analysis.
Serum TnI levels were measured before PCI (baseline), and 6 and 24 hours after PCI, using Dimension equipment (Dade Behring, Newark, DE, USA). Serum CK-MB levels were measured in the same manners using ADVIA Centaur (Bayer Corporation, Tarrytown, NY, USA). The upper cutoff level for a diagnosis of elevated troponin I was 1.5 ng/mL, and that of elevated CK-MB was 5 ng/mL.
The following parameters were recorded and analyzed: baseline demographics, smoking history, presence of diabetes and/or hypertension, clinical syndromes that led to PCI (stable or unstable angina), baseline hematology, and blood chemistry. All cineangiograms were reviewed by experienced operators to identify the morphological characteristics of lesions, including bifurcation, irregularity, calcification, angulation, ostial lesion, total occlusion, and the presence of thrombus.
Angiographic dissection was based on the A to F classification of the National Heart, Lung and Blood Institute. Side-branch occlusion was considered to be a flow grade of less than thrombolysis in myocardial infarction (TIMI) 3 in a side branch with a diameter of more than 1.5 mm, with normal flow occurring before the procedure.
Angiographic success was defined as less than 30% residual diameter stenosis, with TIMI 3 flow, at the end of the procedure. Clinical success was defined as angiographic success without in-hospital complications such as death, Q-wave myocardial infarction, or urgent bypass surgery.
Patients were selected for coronary stenting by the operator based on preintervention lesion characteristics. All patients underwent PCI with Cypher (Cordis Corporation, Miami, FL, USA), Taxus (Boston Scientific, Natick, MA, USA), or both. All patients received aspirin (100 mg daily) before and after PCI. Clopidogrel was administered at a loading dose of 450 mg prior to PCI. Bolus intravenous heparin, with doses adjusted according to body weight (100 U/kg), was given after the insertion of the sheath, followed by the administration of additional boluses as needed. After the procedure, clopidogrel (75 mg/day) or ticlopidine (500 mg/day) was administered for at least six months in addition to lifelong aspirin therapy. Other medications, including beta-blockers, nitrate, angiotensin-converting enzyme inhibitors, and statins, were used as clinically indicated. Patients were excluded from the analysis if they had received glycoprotein IIb/IIIa inhibitors.
All patients were followed up for 400 days. Information was obtained from a review of patient medical records and by telephone interviews with either the patient or the family of the patient. Patient death was ascertained from family members or hospital discharge summaries.
The primary end object of the study was the composite of death, acute myocardial infarction (AMI), subsequent revascularization, coronary bypass surgery, and stroke. AMI during follow-up was defined biochemically by a minimum rise in CK-MB to three times the normal upper limit, or electrocardiographically by the development of new Q waves. Deaths were classified as being of cardiac origin if they were associated with congestive heart failure, arrhythmia, AMI, sudden death, or any other cardiac disease.
Statistical analysis was performed using SPSS version 12.0 (SPSS Inc., Chicago, IL, USA). Continuous variables with normal distributions were expressed as means±SD, and were compared using an unpaired Student's t-test. Categorical variables were compared with Fisher's exact test or the χ2-test, where appropriate. All comparisons were two-sided, and p of <0.05 were regarded as statistically significant.
Logistic regression analysis was used to assess clinical, angiographic, and procedural characteristics associated with TnI elevation. Variables with a significance level of ≤0.25 in univariate analysis were considered to be candidate variables for inclusion in the multivariate analysis. Variables included in the model were gender, diabetes, diagnosis of unstable angina, high sensitivity C-reactive protein (hsCRP), multi-vessel disease, multiple stent implantation, total stent length, irregularity, calcification, bifurcation, and the occurrence of dissection and side-branch occlusion during PCI. Multivariate logistic regression analysis was performed to identify independent predictors of TnI elevation after DES implantation.
Event rates at 400 days were estimated using the Kaplan-Meier method.
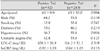
TnI was elevated in 52 (15.5%) of the 335 patients after DES implantation. Table 1 lists the baseline clinical characteristics of these patients. No statistically significant differences between the TnI-positive and TnI-negative groups were detected. There was a non-significant trend toward a greater number of male patients and higher hsCRP levels in the TnI-positive group.
Angiographic and procedural characteristics of the TnI-positive and TnI-negative groups are shown in Table 2. After univariate analysis, the significant predictors (p<0.05) of elevated TnI after DES implantation were as follows: multi-vessel disease (two or more), left circumflex artery involvement, multiple stent implantation, total stent length, bifurcation, and side-branch occlusion. Other characteristics that were associated with the TnI-positive group but not the TnI-negative group were irregularity, calcification, and the occurrence of dissection during PCI.
Logistic regression analysis (enter method) was used to identify independent predictors of elevated TnI after DES implantation. The significant independent predictors of elevated TnI after DES implantation were multi-vessel disease, side-branch occlusion, and bifurcation lesion (Table 3).
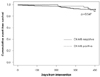
Fig. 1 shows freedom from clinical events during the 400-day follow-up period. There were three cases of stroke, one case of death, and 19 cases of subsequent revascularization in the TnI-negative group. One case of death and five cases of subsequent revascularization were observed in the TnI-positive group. These findings were not clinically significant (p=0.461). Myocardial infarction did not occur in either group. In addition, CK-MB elevation did not affect adverse clinical outcomes (p=0.547) (Fig. 2).
This study investigated the incidence, predictive factors, and prognostic significance of elevated TnI after successful DES implantation. In this study, the incidence of elevated post-PCI troponin (15.5%) was similar to those reported by previous studies, which have indicated incidences ranging from 13.6% to 44.2%.7-10)15-17)22-26) The wide variation in the findings of these reports can be explained by differences in clinical syndromes, procedural characteristics, troponin type, assay methods, and cutoff levels used in each study.
The predictive factors associated with the elevation of postprocedural troponin in the present study correspond to those reported in earlier studies. Most studies have shown that multi-vessel disease, total lesion length, stent length, and side-branch occlusion are independent predictors of troponin elevation after PCI.1)5)7)19)23) Contrary to our results, some studies have demonstrated that thrombus formation is an important predictor.22)26) The thrombus burden increases with the total length of a lesion, and is probably associated with distal embolization.
We found that the elevation of TnI after successful PCI was not associated with recognizable adverse clinical outcomes. Recent large clinical trials and meta-analyses have shown that the elevation of TnI after PCI does not influence long-term mortality.15)16)18) Some studies have suggested that the elevation of TnI after PCI is associated with in-hospital complications. However, they observed that TnI elevation did not result in worse late-term clinical outcomes.24)25) In contrast to our findings, some reports have demonstrated that postprocedural troponin elevation is predictive of increased cardiac events. Ricciardi et al.26) reported that a three-fold elevation of TnI after successful elective PCI is predictive of future cardiac events. However, the major adverse cardiac event that occurred was not cardiovascular death or myocardial infarction, but the need for revascularization. In that study, most patients were treated with balloon angioplasty or a bare metal stent. Our study included patients treated with DES only, which could play a significant role in lowering the need for revascularization. Other studies that have shown significant differences in mortality included high-risk patients, some of whom had elevated troponin levels at baseline, renal insufficiency, and left ventricular systolic dysfunction.20-22) Such high-risk patients were excluded from our study. Therefore, our findings may be more applicable to very low-risk populations. Natarajan et al.23) showed that isolated TnI elevation without concomitant CK-MB elevation after PCI had no significant prognostic value in a series of 1128 patients, and showed similarity to our results.
The limitations of the present study are related to its small sample size. Because we aimed to include low-risk patients, our study population is relatively small, and this is reflected by the low incidence of clinical events. In addition, the length of follow-up was relatively short with regard to the low-risk study population. Because of both of these issues, the power of this study to detect significant differences in clinical outcome might have been limited. However, our findings could provide baseline data for larger prospective evaluations in patients undergoing successful PCI with DES. Further investigations should determine whether the release of TnI after DES implantation in patients, including those in high-risk groups, is correlated with adverse clinical outcomes.
In conclusion, our observations indicate that the significant predictors of elevated TnI after successful implantation of DES were multi-vessel disease, left circumflex artery involvement, multiple stent implantation, total stent length, bifurcation lesion, and side-branch occlusion. The independent predictors of elevated TnI following DES implantation were multi-vessel disease, side-branch occlusion, and bifurcation. The elevation of TnI after PCI with DES had no significant prognostic value in terms of 400-day adverse clinical events.
Figures and Tables
Fig. 1
Kaplan-Meier curves for event-free survival in troponin I (TnI)-positive and TnI-negative groups after implantation of drug-eluting stents.
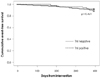
Fig. 2
Kaplan-Meier curves for event-free survival in creatinine kinase (CK)-MB-positive and CK-MB-negative groups after implantation of drug-eluting stents.
References
1. Selvanayagam JB, Porto I, Channon K, et al. Troponin elevation after percutaneous coronary intervention directly represents the extent of irreversible myocardial injury: insights from cardiovascular magnetic resonance imaging. Circulation. 2005. 111:1027–1032.
2. Ricciardi MJ, Wu E, Davidson CJ, et al. Visualization of discrete microinfarction after percutaneous coronary intervention associated with mild creatine kinase-MB elevation. Circulation. 2001. 103:2780–2783.
3. Mehran R, Dangas G, Mintz GS, et al. Atherosclerotic plaque burden and CK-MB enzyme elevation after coronary interventions: intravascular ultrasound study of 2256 patients. Circulation. 2000. 101:604–610.
4. Califf RM, Abdelmeguid AE, Kuntz RE, et al. Myonecrosis after revascularization procedures. J Am Coll Cardiol. 1998. 31:241–251.
5. Kim JH, Jeong MH, Sim DS, et al. The usefulness of cardiac troponin as a marker for the detection of minor myocardial injury following percutaneous coronary intervention. Korean Circ J. 2002. 32:413–419.
6. Cho BR, Hong KP, Gwon HC, et al. Impact on long-term adverse cardiac events of troponin T or creatine kinase-MB release after percutaneous transluminal coronary angiography. Korean Circ J. 2002. 32:949–957.
7. Segev A, Goldman LE, Cantor WJ, et al. Elevated troponin-I after percutaneous coronary interventions: incidence and risk factors. Cardiovasc Radiat Med. 2004. 5:59–63.
8. Mandadi VR, DeVoe MC, Ambrose JA, et al. Predictors of troponin elevation after percutaneous coronary intervention. Am J Cardiol. 2004. 93:747–750.
9. Stone GW, Mehran R, Dangas G, Lansky AJ, Kornowski R, Leon MB. Differential impact on survival of electrocardiographic Q-wave versus enzymatic myocardial infarction after percutaneous intervention: a device-specific analysis of 7147 patients. Circulation. 2001. 104:642–647.
10. Brener SJ, Ellis SG, Schneider J, Topol EJ. Frequency and longterm impact of myonecrosis after coronary stenting. Eur Heart J. 2002. 23:869–876.
11. Ellis SG, Chew D, Chan A, Whitlow PL, Schneider JP, Topol EJ. Death following creatine kinase-MB elevation after coronary intervention: identification of an early risk period: importance of creatine kinase-MB level, completeness of revascularization, ventricular function, and probable benefit of statin therapy. Circulation. 2002. 106:1205–1210.
12. Saucedo JF, Mehran R, Dangas G, et al. Long-term clinical events following creatine kinase: myocardial band isoenzyme elevation after successful coronary stenting. J Am Coll Cardiol. 2000. 35:1134–1141.
13. Tardiff BE, Califf RM, Tcheng JE, et al. Clinical outcomes after detection of elevated cardiac enzymes in patients undergoing percutaneous intervention. J Am Coll Cardiol. 1999. 33:88–96.
14. Kornowski R, Fuchs S, Hong MK, et al. Prognostic value of recurrent episodes of creatine kinase-MB elevation following repeated catheter-based coronary interventions. Catheter Cardiovasc Interv. 2000. 51:131–137.
15. Cavallini C, Savonitto S, Violini R, et al. Impact of the elevation of biochemical markers of myocardial damage on long-term mortality after percutaneous coronary intervention. Eur Heart J. 2005. 26:1494–1498.
16. Kini AS, Lee P, Marmur JD, et al. Correlation of postpercutaneous coronary intervention creatine kinase-MB and troponin I elevation in predicting mid-term mortality. Am J Cardiol. 2004. 93:18–23.
17. Bertinchant JP, Polge A, Ledermann B, et al. Relation of minor cardiac troponin I elevation to late cardiac events after uncomplicated elective successful percutaneous transluminal coronary angioplasty for angina pectoris. Am J Cardiol. 1999. 84:51–57.
18. Wu AH, Boden WE, McKay RG. Long-term follow-up of patients with increased cardiac troponin concentrations following percutaneous coronary intervention. Am J Cardiol. 2002. 89:1300–1302.
19. Ramirez-Moreno A, Cardenal R, Pera C, et al. Predictors and prognostic value of myocardial injury following stent implantation. Int J Cardiol. 2004. 97:193–198.
20. Gruberg L, Fuchs S, Waksman R, et al. Prognostic value of cardiac troponin I elevation after percutaneous coronary intervention in patients with chronic renal insufficiency: a 12-month outcome analysis. Catheter Cardiovasc Interv. 2002. 55:174–179.
21. Cantor WJ, Newby LK, Christenson RH, et al. Prognostic significance of elevated troponin I after percutaneous coronary intervention. J Am Coll Cardiol. 2002. 39:1738–1744.
22. Nallamothu BK, Chetcuti S, Mukherjee D, et al. Prognostic implication of troponin I elevation after percutaneous coronary intervention. Am J Cardiol. 2003. 91:1272–1274.
23. Natarajan MK, Kreatsoulas C, Velianou JL, Mehta SR, Pericak D, Goodhart DM. Incidence, predictors, and clinical significance of troponin-I elevation without creatine kinase elevation following percutaneous coronary interventions. Am J Cardiol. 2004. 93:750–753.
24. Garbarz E, Iung B, Lefevre G, et al. Frequency and prognostic value of cardiac troponin I elevation after coronary stenting. Am J Cardiol. 1999. 84:515–518.
25. Fuchs S, Kornowski R, Mehran R, et al. Prognostic value of cardiac troponin-I levels following catheter-based coronary interventions. Am J Cardiol. 2000. 85:1077–1082.
26. Ricciardi MJ, Davidson CJ, Gubernikoff G, et al. Troponin I elevation and cardiac events after percutaneous coronary intervention. Am Heart J. 2003. 145:522–528.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download