Abstract
An exercise-induced idiopathic Brugada electrocardiographic pattern during the effort phase is very rare. A 42-year-old male visited our cardiology clinic for chest discomfort. He has been treated for myocardial infarction 2 months ago. He underwent a treadmill test according to the Bruce protocol. Typical coved-type ST-segment elevation was found during the effort phase, and it gradually recovered after the exercise. The ST-segment elevation appeared to be unrelated to hypervagotonia. This elevation was not induced by a pharmacological test with flecainide. A significant ventricular arrhythmia was not induced by programmed ventricular stimulation. Hence, we discharged the patient without implantation of an implantable cardioverter defibrillator.
Brugada syndrome shows 2 characteristic findings, namely, ST-segment elevation in the right precordial leads and right bundle branch block.1-4) Generally, the increase in the heart rate during exercise decreases the ST-segment elevation. However, immediately after exercise, there is an increase in the ST-segment elevation during the recovery phase.5) This is related to an increase in the vagal tone.6) In the present case, typical coved-type ST-segment elevation was detected in the effort phase and not in the recovery phase.
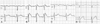
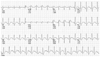
A 42-year-old male visited our cardiology clinic with a complaint of chest discomfort after meals. Two months ago, this patient was transferred to emergency room due to ST-segment elevation myocardial infarction (Fig. 1A). During transfer, he suddenly developed ventricular fibrillation (Fig. 1B); however, paramedics successfully converted his defibrillation to normal sinus rhythm. Coronary angiography revealed significant stenosis at the proximal third of the left anterior descending artery with plaque rupture (Fig. 2A). After predilation using a balloon catheter, a stent (TAXUS® 3.5×28 mm, Boston Scientific, Boston, USA) was implanted in the left anterior descending artery. The condition of the patient improved, and he did not experience chest pain. No echocardiographic and electrocardiographic (ECG) abnormalities were observed after percutaneous coronary intervention. Furthermore, Holter monitoring revealed no ST-segment or T-wave abnormality. The patient was exsmoker. His family history revealed that his grandfather in his fifties had died due to sudden cardiac death. The patient underwent a treadmill test for the evaluation of chest discomfort that developed after meals. The resting ECG finding was normal (Fig. 3A). The patient did not complain of chest pain during the effort phase but showed coved-type ST-segment elevation in V1 and V2 (2 mm in V1 and 6 mm in V2) (Fig. 3B). However, no reciprocal changes were observed (Fig. 4). It is suggested that the findings were not because of coronary disease or vasospasm that might reproduce chest pain. This coved-type ST-segment elevation normalized during the recovery phase (Fig. 3C). Hence, Brugada syndrome was suspected, and the patient was admitted to hospital for risk stratification. The patency of the previously inserted stent was determined by a follow-up coronary angiography, and no newly developed stenosis was observed (Fig. 2B, C). A flecainide infusion test (120 µg/min for 15 min) was performed.7)8) However, typical coved-type ST-segment elevation was not induced during this test (Fig. 3D). Subsequently, a programmed ventricular stimulation study was carried out for risk stratification.8)9) In this study with isoproterenol infusion (1-5 µg/min), only triplet beats were induced without ventricular arrhythmias by triple stimulations. We considered that the patient had a low possibility for ventricular fibrillation and planned a close observation instead of implantation of an implantable cardioverter defibrillator.8)
The QRS complex in Brugada syndrome ends with a positive deflection (or prominent J wave), followed by an elevated downsloping ST-segment (coved-type ST-segment elevation) and a negative T wave with a normal or even short QT interval.10)12) The appearance of the ECG features in the absence of clinical symptoms is referred to as an idiopathic Brugada ECG pattern (and not Brugada syndrome).1) In the present case, the patient first developed ventricular fibrillation, which might be caused by ST-segment elevation myocardial infarction and not by Brugada syndrome. Thus, it is certain that this patient had idiopathic Brugada ECG pattern.
Generally, typical coved-type ST-segment elevation decreases during exercise with an increase in the heart rate. Immediately after exercise, the ST-segment elevation increases during the recovery phase.5) This is related to the increment in the vagal tone.6) Arrhythmia and sudden death in Brugada syndrome usually occur during sleep or rest and are commonly associated with bradycardia. In our patient, unexpected coved-type ST-segment elevation was found during the effort phase but not during the recovery phase; this suggests that the ST-segment elevation was not associated with the increment in the vagal tone. A similar case has been reported in Mexico by Guevara-Valdivia et al.13) The present case of idiopathic Brugada ECG pattern that occurred in the effort phase and not in the recovery phase is the first of its kind to be reported in Korea.
Figures and Tables
 | Fig. 1Electrocardiogram (ECG) findings at emergency room. A: the ECG shows ST-segment elevation in V1-V3, thereby implying anterior wall myocardial infarction. B: during transfer, the patient suddenly developed ventricular fibrillation. |
 | Fig. 2Diagnostic coronary angiography at admission and follow-up coronary angiography. A: significant stenosis (arrow) was observed at the proximal third of the left anterior descending artery with plaque rupture. B: the patency of the previously inserted stent was determined by a follow-up coronary angiography, and no newly developed stenosis was observed. C: right coronary angiography revealed no significant luminal narrowing. |
 | Fig. 3Serial electrocardiogram (ECG) findings. A: resting ECG shows no ST-segment elevation in the precordial leads. B: coved-type ST-segment elevation (2 mm in V1 and 6 mm in V2) was observed during the effort phase. C: ST-segment elevation was normalized during the recovery phase. D: a flecainide infusion test (120 µg/min for 15 min) was performed. However, typical Brugada-like ECG pattern was not induced during this test. |
References
1. Wilde AA, Antzelevitch C, Borggrefe M, et al. Proposed diagnostic criteria for the Brugada syndrome. Circulation. 2002. 106:2514–2519.
2. Brugada J, Brugada R, Brugada P. Right bundle-branch block and ST-segment elevation in leads V1 through V3: a marker for dudden death in patients without demonstrable structural heart disease. Circulation. 1998. 97:457–460.
3. Corrado D, Basso C, Buja G, Nava A, Rossi L, Thiene G. Right bundle branch block, right precordial ST-segment elevation, and sudden death in young people. Circulation. 2001. 103:710–717.
4. Brugada J, Brugada R, Brugada P. Determinants of sudden cardiac death in individuals with the electrocardiographic pattern of Brugada syndrome and no previous cardiac arrest. Circulation. 2003. 108:3092–3096.
5. Brugada R, Brugada P, Brugada J. Electrocardiogram interpretation and class I blocker challenge in Brugada syndrome. J Electrocardiol. 2006. 39:Suppl. S115–S118.
6. Mizumaki K, Fujiki A, Tsuneda T, et al. Vagal activity modulates spontaneous augmentation of ST elevation in the daily life of patients with Brugada syndrome. J Cardiovasc Electrophysiol. 2004. 15:667–673.
7. Brugada R, Brugada J, Antzelevitch C, et al. Sodium channel blockers identify risk for sudden death in patients with ST-segment elevation and right bundle branch block but structurally normal hearts. Circulation. 2000. 101:510–515.
8. Brugada P, Brugada R, Brugada J. Should patients with an asymptomatic Brugada electrocardiogram undergo pharmacological and electrophysiological testing? Circulation. 2005. 112:279–292.
9. Priori SG, Napolitano C, Gasparini M, et al. Natural history of Brugada syndrome: insight for risk stratification and management. Circulation. 2002. 105:1342–1347.
10. Bjerregaard P, Gussak I, Antzelevitch C. The enigmatic ECG manifestation of Brugada syndrome. J Cardiovasc Electrophysiol. 1998. 9:109–112.
11. Lee MY. Brugada syndrome. Korean Circ J. 2002. 32:461–466.
12. Gussak I, Antzelevitch C, Bjerregaard P, Towbin JA, Chaitman BR. The Brugada syndrome: clinical, electrophysiologic and genetic aspects. J Am Coll Cardiol. 1999. 33:5–15.
13. Guevara-Valdivia ME, de Micheli A, Iturralde P, et al. Infrequent electrocardiographic changes during exercise stress test in a patient with Brugada's syndrome. Arch Cardiol Mex. 2003. 73:212–217.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download