Abstract
Background and Objectives
Endothelial dysfunction plays a key role in atherogenesis and it can predict future cardiovascular events in subjects with and without coronary artery disease. This study was designed to evaluate the association between endothelial dysfunction and major adverse cardiovascular events (MACEs), and especially future stroke in patients who have undergone percutaneous coronary intervention (PCI).
Subjects and Methods
The study subjects consisted of 182 patients (mean age; 59 years, 120 males) who underwent PCI and flow-mediated brachial arterial dilation (FMD) using high-resolution ultrasound. They were followed up for a mean of 28 months (maximum; 34 months). MACEs included cardiac death, non-cardiac death, acute myocardial infarction (AMI), stroke, coronary artery bypass graft (CABG), target lesion revascularization (TLR) and PCI due to de novo lesion during follow-up.
Results
The study subjects were divided into two groups according to the median value of the FMD; one was a patient with a high FMD (3.61% and the other was a patients with a low FMD<3.61%. There were 74 MACEs in 66 patients; 3 AMIs, 7 strokes, 49 TLRs, 2 CABGs and 13 de novo PCIs. FMD showed no significant differences between the patients with and without MACEs (3.9±2.3% vs. 4.1±2.1%, respectively, p>0.05). Univariate analysis showed that the patients with a lower FMD had a higher incidence of stroke (7 vs. 0, respectively, p=0.005) than those patients with a higher FMD, while there was no significant difference between the two groups in terms of AMI (1 vs. 2, respectively), TLR (28 vs. 21, respectively), de novo PCI (6 vs. 7, respectively), CABG (0 vs. 2, respectively) and cardiac death (0 vs. 0, respectively). On the multivariate Cox regression analysis, FMD was the strongest predictor of stroke (OR; 0.418, 95% CI; 0.185 to 0.940, p=0.035).
Figures and Tables
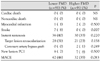
 | Fig. 1Kaplan-Meier analysis of event-free survival curves according to the level of flow-mediated dilation (FMD). A: analysis for all major adverse cardiovascular events (MACE). B: analysis for stroke. |
Table 1
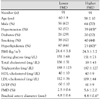
Patients demographics according to the presence of MACE

*p<0.05 compared with group of with MACE. MACE: major adverse cardiovascular event, BMI: body mass index, HDL: high density lipoprotein, LDL: low density lipoprotein, Hs-CRP: high sensitivity-C reactive protein, LVEF: left ventricle ejection fraction, FMD: flow mediated dilation, AMI: acute myocardial infarction, MI: myocardial infarction, DS: diameter stenosis
References
1. Celermajer DS, Sorensen KE, Gooch VM, et al. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet. 1992. 340:1111–1115.
2. Wildlansky ME, Gokce N, Keaney JF Jr, Vita JA. The clinical implications of endothelial dysfunction. J Am Coll Cardiol. 2003. 42:1149–1160.
3. Celermajer DS, Sorensen KE, Bull C, Robinson J, Deanfield JE. Endothelium-dependent dilation in the systemic arteries of asymptomatic subjects relates to coronary risk factors and their interaction. J Am Coll Cardiol. 1994. 24:1468–1474.
4. Yoon HJ, Bae JH, Kim KY, Kim JK. Age, gender, and number of atherosclerotic risk factors are the independent factor of endothelial dysfunction in patients with coronary atherosclerosis. Korean Circ J. 2005. 35:302–308.
5. Heitzer T, Schlinzig T, Krohn K, Meinertz T, Munzel T. Endothelial dysfunction, oxidative stress, and risk of cardiovascular events in patients with coronary artery disease. Circulation. 2001. 104:2673–2678.
6. Schachinger V, Britten MB, Zeiher AM. Prognostic impact of coronary vasodilator dysfunction on adverse long-term outcome of coronary heart disease. Circulation. 2000. 101:1899–1906.
7. Gokce N, Keaney JF Jr, Hunter LM, et al. Predictive value of noninvasively determined endothelial dysfunction for long-term cardiovascular events in patients with peripheral vascular disease. J Am Coll Cardiol. 2003. 41:1769–1775.
8. Park KR, Bae JH. Differential endothelial function according to the presence of restenosis in patients having undergone percutaneous transluminal coronary angioplasty. Korean Circ J. 2001. 31:1117–1122.
9. Patti G, Pasceri V, Melfi R, et al. Impaired flow-mediated dilation and risk of restenosis in patients undergoing coronary stent implantation. Circulation. 2005. 111:70–75.
10. Targonski PV, Bonetti PO, Pumper GM, Higano ST, Holmes DR, Lerman A. Coronary endothelial dysfunction is associated with an increased risk of cerebrovascular events. Circulation. 2003. 107:2805–2809.
11. Bae JH, Bassenge E, Kim KB, et al. Postprandial hypertriglyceridemia impairs endothelial function by enhanced oxidant stress. Atherosclerosis. 2001. 155:517–523.
12. Corretti MC, Anderson TJ, Benjamin EJ, et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of brachial artery. J Am Coll Cardiol. 2002. 39:257–265.
13. Kannel WB, Wolf PA, Verter J. Manifestations of coronary diasease predisposing to stroke. JAMA. 1983. 250:2942–2946.
14. Park KR, Bae JH. Comparison of the endothelial function between healthy subjects and patients with coronary artery diasease or risk factors of atherosclerosis. Korean Circ J. 2001. 31:544–550.
15. Felmeden DC, Spencer CG, Chung NA, et al. Relation of thrombogenesis in systemic hypertension to angiogenesis and endothelial damage/dysfunction (a substudy of the Anglo-Scandinavian Cardiac Outcomes Trial [ASCOT]). Am J Cardiol. 2003. 92:400–405.
16. Paniagua OA, Bryant MB, Panza JA. Role of endothelial nitric oxide in shear stress-induced vasodilation of human microvasculature. Circulation. 2001. 103:1752–1758.
17. McAllister AC, Atkinson AB, Johnston GD, Hadden DR, Bell PM, McCance DR. Basal nitric oxide production is impaired in offspring of patients with essential hypertension. Clin Sci. 1999. 97:141–147.
18. Vane JR, Anggard EE, Botting RM. Regulatory functions of the vascular endothelium. N Engl J Med. 1990. 323:27–36.
19. Hse HY, Chen YT, Sheu WHH, Sheng WY, Chao AC. Comparison of brachial artery flow-mediated vasodilation in symptomatic and asymptomatic patients with carotid arterial stenosis. Am J Cardiol. 2002. 90:814–816.
20. O'Driscoll G, Green D, Taylor RR. Simvastatin, an HMG-coenzyme A reductase inhibitor, improves endothelial function within 1 month. Circulation. 1997. 95:1126–1131.
21. Mancini J, Henry GC, Macaya C, et al. Angiotensin-converting enzyme inhibition with quinapril improves endothelial vasomotor dysfunction in patients with coronary artery disease. Circulation. 1996. 94:258–265.
22. Kleindorfer D, Broderick J, Khoury J, et al. The unchanging incidence and case-fatality of stroke in the 1990s: a population-based study. Stroke. 2006. 37:2473–2478.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download